Supplementary Data - European Heart Journal
advertisement
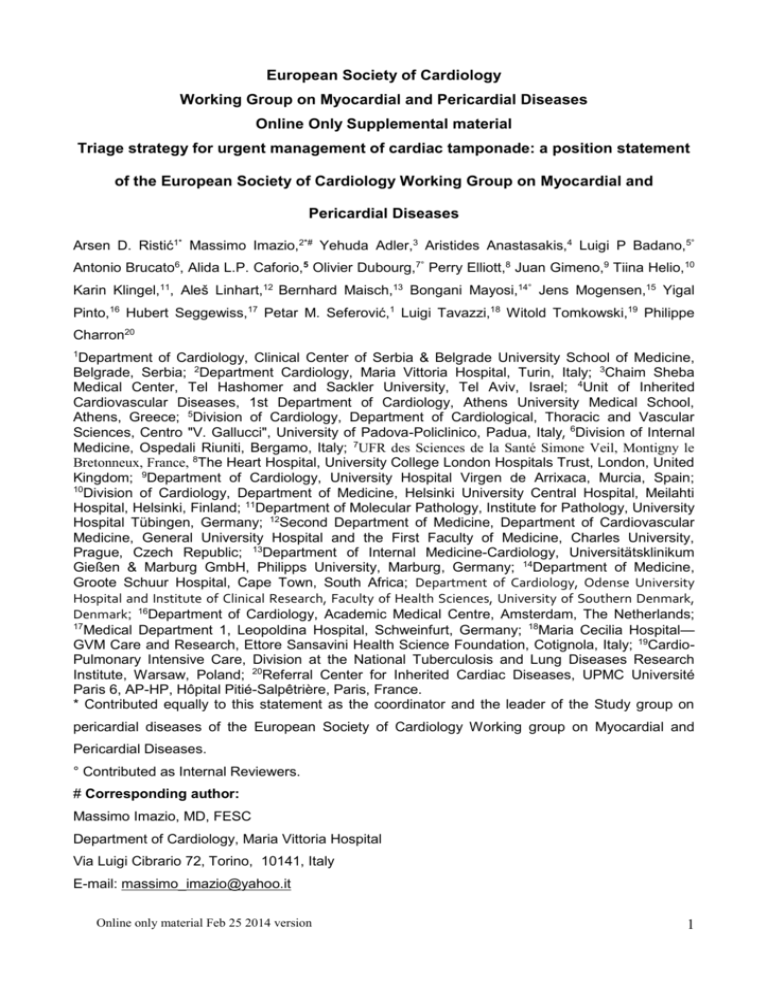
European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Online Only Supplemental material Triage strategy for urgent management of cardiac tamponade: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases Arsen D. Ristić1* Massimo Imazio,2*# Yehuda Adler,3 Aristides Anastasakis,4 Luigi P Badano,5° Antonio Brucato6, Alida L.P. Caforio,5 Olivier Dubourg,7° Perry Elliott,8 Juan Gimeno,9 Tiina Helio,10 Karin Klingel,11, Aleš Linhart,12 Bernhard Maisch,13 Bongani Mayosi,14° Jens Mogensen,15 Yigal Pinto,16 Hubert Seggewiss,17 Petar M. Seferović,1 Luigi Tavazzi,18 Witold Tomkowski,19 Philippe Charron20 1 Department of Cardiology, Clinical Center of Serbia & Belgrade University School of Medicine, Belgrade, Serbia; 2Department Cardiology, Maria Vittoria Hospital, Turin, Italy; 3Chaim Sheba Medical Center, Tel Hashomer and Sackler University, Tel Aviv, Israel; 4Unit of Inherited Cardiovascular Diseases, 1st Department of Cardiology, Athens University Medical School, Athens, Greece; 5Division of Cardiology, Department of Cardiological, Thoracic and Vascular Sciences, Centro "V. Gallucci", University of Padova-Policlinico, Padua, Italy, 6Division of Internal Medicine, Ospedali Riuniti, Bergamo, Italy; 7UFR des Sciences de la Santé Simone Veil, Montigny le Bretonneux, France, 8The Heart Hospital, University College London Hospitals Trust, London, United Kingdom; 9Department of Cardiology, University Hospital Virgen de Arrixaca, Murcia, Spain; 10 Division of Cardiology, Department of Medicine, Helsinki University Central Hospital, Meilahti Hospital, Helsinki, Finland; 11Department of Molecular Pathology, Institute for Pathology, University Hospital Tübingen, Germany; 12Second Department of Medicine, Department of Cardiovascular Medicine, General University Hospital and the First Faculty of Medicine, Charles University, Prague, Czech Republic; 13Department of Internal Medicine-Cardiology, Universitätsklinikum Gießen & Marburg GmbH, Philipps University, Marburg, Germany; 14Department of Medicine, Groote Schuur Hospital, Cape Town, South Africa; Department of Cardiology, Odense University Hospital and Institute of Clinical Research, Faculty of Health Sciences, University of Southern Denmark, Denmark; 16Department of Cardiology, Academic Medical Centre, Amsterdam, The Netherlands; 17 Medical Department 1, Leopoldina Hospital, Schweinfurt, Germany; 18Maria Cecilia Hospital— GVM Care and Research, Ettore Sansavini Health Science Foundation, Cotignola, Italy; 19CardioPulmonary Intensive Care, Division at the National Tuberculosis and Lung Diseases Research Institute, Warsaw, Poland; 20Referral Center for Inherited Cardiac Diseases, UPMC Université Paris 6, AP-HP, Hôpital Pitié-Salpêtrière, Paris, France. * Contributed equally to this statement as the coordinator and the leader of the Study group on pericardial diseases of the European Society of Cardiology Working group on Myocardial and Pericardial Diseases. ° Contributed as Internal Reviewers. # Corresponding author: Massimo Imazio, MD, FESC Department of Cardiology, Maria Vittoria Hospital Via Luigi Cibrario 72, Torino, 10141, Italy E-mail: massimo_imazio@yahoo.it Online only material Feb 25 2014 version 1 Diagnostic algorithm Clinical diagnosis The causes of cardiac tamponade are varied and discussed in the main text (1-13). Cardiac tamponade includes a haemodynamic spectrum ranging from incipient or preclinical tamponade (pericardial pressure equals right atrial pressure but it is lower than left atrial pressure) to initial cardiac tamponade when pericardial pressure equals left atrial pressure (1-3). Cardiac tamponade is moderate when the pericardial pressure is higher than 10-12 mmHg and an abnormal jugular pulse can be detected along with signs of compression of right heart chambers (4). Further elevation of pericardial pressure is responsible for advanced tamponade characterized by significant reduction of the stroke volume, blood pressure, and by sinus tachycardia (Table 1s). At this stage pulsus paradoxus becomes evident (13,20,21). The rate of pericardial fluid accumulation is critical for the clinical presentation. If pericardial fluid is quickly accumulating, even less than 250 ml, may cause acute cardiac tamponade (often called “surgical tamponade”) within few minutes. Conversely, a slowly accumulating pericardial fluid may allow the collection of 1000-1500 ml or even larger effusions within days or weeks before a significant elevation of intrapericardial pressure and the development of cardiac tamponade. Such clinical presentations are less dramatic and have been also reported as “medical tamponade” to underline that different medical non-traumatic causes are the underlying cause and different therapeutic approaches may be considered (13,22). Classical symptoms of cardiac tamponade include tachycardia, tachypnea, dyspnea on exertion progressing to orthopnea, chest pain, oliguria and/or a sensation of fullness (1,20). Additional occasional symptoms due to local compression may include nausea (diaphragm), dysphagia (oesophagus), hoarseness (recurrent laryngeal nerve), hiccups 2 (phrenic nerve) (22). Right upper quadrant pain may be present as a symptom related to hepatic venous congestion. Nonspecific symptoms include also cough, weakness, fatigue, anorexia, and palpitations reflecting the compressive effect of the pericardial fluid on contiguous anatomic structures or reduced blood pressure and secondary sinus tachycardia. The classical findings of cardiac tamponade were described by the thoracic surgeon Beck in 1935 (23) as a triad including hypotension, increased jugular venous pressure, and a small and quiet heart. This triad has classically been identified in “surgical tamponade” with acute haemodynamic collapse due to intrapericardial hemorrhage caused by trauma, myocardial or aortic rupture. The triad may be lacking in patients with slowly accumulating pericardial fluid (24). Hypotension may be absolute or relative. Acute cardiac tamponade is usually associated with low blood pressure (<100 mmHg) but blood pressure is only slightly reduced in subacute, chronic tamponade. Hypertensive patients may have normal or even mild elevation of blood pressure concomitant to cardiac tamponade due to the increased adrenergic tone and circulating catecholamines (25). Fever is a non-specific sign that may be associated with infectious or immune-mediated pericarditis. On physical examination classical signs include neck vein distention with elevated jugular venous pressure, pulsus paradoxus, and diminished heart sounds on cardiac auscultation. Pulsus paradoxus was described first by Kussmaul in 1873 as a palpable reduction of radial pulse on inspiration in patients with cardiac tamponade (“waxing and waning” of the peripheral pulse, in contrast to the unvarying strength of the apical cardiac impulse) (26). Pulsus paradoxus is defined as an inspiratory reduction of at least 10 mmHg of the systolic blood pressure. It can be easily detected recording the systolic pressure at which Korotkoff sounds are first audible and the systolic pressure at which they are audible through the whole respiratory cycle. Online only material Feb 25 2014 version 3 Laboratory findings and imaging-based diagnosis There are no specific laboratory data in cardiac tamponade. Sinus tachycardia is the major finding at electrocardiography (ECG). The ECG may show low QRS voltage and electrical alternans (electrical alternans is an electrocardiographic phenomenon of alternation of QRS complex amplitude or axis between beats. It is seen in cardiac tamponade and severe pericardial effusion and is thought to be related to changes in the ventricular electrical axis due to a swinging heart within the pericardial sac) (Figure 1s). Both findings are usually considered suggestive of a large pericardial effusion, but have a low reported sensitivity (<50%) (20). However, a prospective study has demonstrated that low QRS voltages may be a feature of cardiac tamponade but not of pericardial effusion per se. Low QRS voltage (defined as maximum QRS amplitude <0.5 mV in the limb leads) was found in 61% of patients with cardiac tamponade but in none with effusions without cardiac tamponade (27). Normalization of the QRS amplitude was not recorded immediately after pericardiocentesis but only after a week (27). ECG findings seem to have limited sensitivity for cardiac tamponade: low QRS voltage had a sensitivity of 42%, and electrical alternans of only 16-21%. Atrial arrhythmias have been rarely reported, whereas widespread ST segment elevation with or without PR depression in the setting of acute pericarditis was noted frequently (20). Chest x-ray In patients with mild to moderate pericardial effusions cardiac silhouette is usually normal, while the cardiac silhouette has a typical “water bottle” appearance with a large effusion (Figure 2s). Such a simple sign in the appropriate clinical context (symptomatic patients 4 with large pericardial effusion) has a high sensitivity for the diagnosis of cardiac tamponade, but does not determine the urgency of pericardiocentesis. On well-penetrated chest x-rays in the lateral view (or better in fluoroscopy), pericardial fluid may be suggested by lucent lines within the cardiac shadow (epicardial halo sign) (28,29). Echocardiography Echocardiography is the first level diagnostic method for the assessment of the presence, size and hemodynamic importance of pericardial effusion (3,30) and to guide pericardiocentesis (Figure 3s). According to a common semiquantitative assessment pericardial effusions are graded according to the echo-free space in diastole (3, 31,32) as small (<10 mm), moderate (10-20 mm), and large (>20 mm). Echocardiography is mandatory for the initial assessment and follow-up of all patients with suspected pericardial diseases (33). Most cases of cardiac tamponade show moderate to large pericardial effusion. The swinging of the heart within the pericardial fluid is a common finding (Supplemental movie 1 and 2) (34). Echocardiographic findings in cardiac tamponade are determined by transient chambers collapse and increased ventricular interdependence (34,35). Major signs (Table 2s) include: 1. Diastolic prolonged collapse of the right atrium (RA) is an early sign that can be detected with moderate to large pericardial effusions without cardiac tamponade, because the RA is the cardiac chamber with the lowest pressures. A ratio of RA collapse time to cardiac cycle length >0.34 is a very specific sign of cardiac tamponade. At the end of diastole the RA volume is minimal while pericardial pressure is maximal (36), thus diastolic collapse of the RA usually occurs at late diastole while collapse of RV happens at early diastole. 2. The diastolic collapse of the right ventricle (RV) was first described by Schiller and Botvinick in 1977 (37). It is less sensitive for the presence of cardiac tamponade than Online only material Feb 25 2014 version 5 the RA collapse but more specific. This sign may be absent in cases of RV hypertrophy or elevated RV diastolic pressure (38). 3. A left ventricular (LV) collapse is recorded in about 25% of cases with cardiac tamponade. It is a not usual but specific sign, because LV pressures are higher and the LV is thicker than RV. This sign can be sometimes seen in regional compression (39). 4. Respiratory variations in volumes and flows of cardiac chambers. Increased ventricular interdependence observed in cardiac tamponade is responsible for reciprocal changes of LV and RV volumes and mitral and tricuspid flows during respiratory phases, as well as for abnormal septal motion during respiratory phases (interventricular septum moving towards the LV during inspiration and towards the RV during expiration, septal bounce). 5. Variations in peak velocities during respiration across the mitral valve, tricuspid valve, and pulmonary outflow that are greater than 25%, 50%, and 30% respectively indicate cardiac tamponade, but similar changes are also observed in constrictive pericarditis (Figure 4s) (17,40,41). 6. Inferior vena cava (IVC) plethora. Less than 50% reduction in the diameter of a dilated IVC (>20 mm) during inspiration reflects a marked elevation in central venous pressure and is frequently reported in patients with cardiac tamponade (42). It is a very sensitive, but not very specific sign, common in other pathologic conditions (e.g. heart failure, tricuspid regurgitation) (20). In the setting of a large pericardial effusion, IVC plethora is a sign of cardiac compression by the effusion (Figure 4s). Points 4 and 5 are consequences of ventricular interdependence. The left (LV) and right ventricles (RV) are enclosed in a stiff envelope, the pericardium. They have similar enddiastolic volumes, and there is limited space for acute ventricular dilatation within a normal pericardium, this limit is even more evident in the presence of large effusion with cardiac 6 tamponade or a rigid pericardium such as in constrictive pericarditis. Thus, when RV enddiastolic volume increases owing to increased RV loading such as during inspiration, it can only occur at the expense of the space devoted to the left ventricle, thus increased right ventricle volume and right flows only occur at the expenses of a reduction of the left ventricle volume and flows. In a prospective clinical study on the correlation between clinical and echocardiographic findings in patients with moderate to large pericardial effusions (43), any chamber collapse had a high sensitivity (90%) but a relatively low specificity (65%). The specificity was higher for abnormal right-sided venous flows (91%), which were not detectable in one third of cases. The integration of chamber collapse and abnormal venous flows provided the highest specificity (98%). In patients with recent cardiac surgery or trauma the presence of localized cardiac tamponade should be carefully considered. In these clinical conditions standard transthoracic echocardiography views can be difficult to obtain due to the inability to put the patient in an appropriate position, and the surgical wounds. In this setting transesophageal echocardiography (TEE) may have a higher diagnostic accuracy than transthoracic echocardiography also for the detection of loculated effusions and localized compression by hematoma (i.e. especially on the RA) (1,44). Other imaging techniques Other imaging techniques, such as computed tomography (CT) and cardiovascular magnetic resonance (CMR) may detect pericardial effusion and suggest signs of cardiac tamponade (i.e. large pericardial effusion, distension of venae cavae and hepatic veins, deformity and compression of cardiac chambers, bowing of the interventricular septum) (Figure 5s) (45). Moreover CT attenuation values of pericardial effusion can help in the differentiation of blood, exudative fluid (20–60 Hounsfield units), as found with purulent Online only material Feb 25 2014 version 7 pericarditis, and simple transudative fluid (<10 Hounsfield units). Coronary sinus compression, an early sign of cardiac tamponade (46), RV wall flattening and pericardial thickening on CT have been described with hemodynamically significant pericardial effusion (47). CT and CMR have a large field view and multiplanar capability, and can image the entire pericardium as well as the complete chest including abnormalities of the surrounding mediastinum and lungs, which is important if aortic pathology or neoplastic diseases have to be considered as underlying causes (48). CT guided catheter insertion with drainage may be useful in the hands of experts, particularly for loculated effusions or accumulation of fluid in unusual sites. Cardiac catheterization and invasive haemodynamics Cardiac catheterization may be considered in case of iatrogenic effusion during percutaneous interventions, but also when there is a discrepancy between the clinical picture and non-invasive imaging data, and may particularly useful for the evaluation of patients with complex hemodynamic disorders (49). Patients in cardiac tamponade usually demonstrate low arterial pressure and tachycardia, an elevated right atrial pressure, with a prominent x descent and a diminished or absent y descent (cardiac compression, which interrupts the venous return is maximal at end-diastole). In cardiac tamponade, the jugular pressure declines normally with inspiration (Kussmaul's sign absent), reflecting augmented systemic venous return. On the contrary, in constrictive or effusive-constrictive pericarditis, right heart failure, or severe tricuspid regurgitation, the mean central venous pressure does not decline during inspiration, and may even increase (Kussmaul's sign present). The pulmonary capillary wedge pressure is elevated and nearly equal to the intrapericardial and right atrial pressure. Except in low-pressure tamponade, diastolic pressures in all heart chambers are usually 15 to 30 mmHg. In contrast to constrictive pericarditis, 8 ventricular diastolic pressure does not have the dip and plateau configuration, but is elevated in early diastole and continues to rise throughout the diastole (49). Right-heart pericardiocentesis, catheterization allowing can monitoring be of performed the efficacy simultaneously of drainage. with After pericardiocentesis, if intrapericardial pressure falls to zero or becomes negative, while the right atrial pressure remains elevated, diagnostic alternatives include effusive-constrictive pericarditis (especially in patients with tuberculosis or prior irradiation for neoplastic disease), preexisting left ventricular dysfunction, tricuspid valve disease, and restrictive cardiomyopathy. The value of cardiac catheterization has been clearly demonstrated for cases with effusive-constrictive pericarditis, in whom the intrapericardial pressure decreased after pericardiocentesis, whereas right atrial and end-diastolic right and left ventricular pressures remained elevated, with a dip-plateau morphology (50). The presence of effusive-constrictive physiology may be also clinically suspected when jugular venous pressure remain elevated after pericardiocentesis and echo examination shows constrictive features. Differential diagnosis In a systematic review of the literature (20), five features have been reported in the majority of patients with cardiac tamponade (>70%): dyspnea (85-90%), cardiomegaly on chest radiograph (89%), pulsus paradoxus (82%), tachycardia (77%), and elevated jugular venous pressure (76%). In the setting of a large pericardial effusion, the presence of pulsus paradoxus (inspiratory decrease of systolic blood pressure >10 mmHg) increased the likelihood of cardiac tamponade (likelihood ratio 3.3) (16). Surprisingly, hypotension and soft heart sounds were insensitive (respectively 26% and 28%). Since cardiac tamponade is primarily a clinical diagnosis, echocardiographic signs are only confirmatory (20). Differential diagnosis may include acute myocardial infarction (especially with RV Online only material Feb 25 2014 version 9 involvement), pulmonary embolism, and aortic dissection in acute onset cases. In patients with a subacute onset of symptoms, the differential diagnosis should exclude constrictive pericarditis, congestive heart failure, advanced liver disease with cirrhosis, rarely Ebstein anomaly. Medical management Medical treatment is only an initial measure until pericardiocentesis or surgical relief can be performed. Volume infusion may be useful for patients with hypovolemia until correction of hypovolemia (4), and allows to gain time to perform pericardiocentesis. On the contrary, it may precipitate or worsen tamponade in normovolemic or hypervolemic patients (51-53). The use of inotropes is not supported by clear evidence-based data (51-53). Although severely hypoxic patients must be intubated and ventilated during the preparation for pericardiocentesis, positive end-expiratory pressure (PEEP) ventilation should be avoided since it may decrease the cardiac output further (54,55). It should be especially pointed out that intravenous administration of diuretics is strongly contraindicated and could be fatal (3), while volume infusion is useful for patients with hypovolemia (4). In patients with cardiac arrest associated with cardiac tamponade (cardiac arrest with pulseless electrical activity- PEA is the late manifestation of uncorrected cardiac tamponade), immediate pericardiocentensis is the substantial key of successful resuscitation. 10 Full reference list: 7. Spodick DH. Acute cardiac tamponade. N Engl J Med 2003;349:684-90. 8. Seferović PM, Ristić AD, Imazio M, Maksimović R, Simeunović D, Trinchero R, Pankuweit S, Maisch B. Management strategies in pericardial emergencies. Herz. 2006;31:891-900. 9. Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH; Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587-610. 10. Hoit BD. Pericardial disease and pericardial tamponade. Crit Care Med 2007;35:S355S364. 11. Imazio M, Cecchi E, Demichelis B, Ierna S, Demarie D, Ghisio A, Pomari F, Coda L, Belli R, Trinchero R. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115(21):2739-44. 12. Ariyarajah V, Spodick DH. Cardiac tamponade revisited: a postmortem look at a cautionary case. Tex Heart Inst J. 2007;34:347-51. 13. Sagristà-Sauleda J, Mercé AS, Soler-Soler J. Diagnosis and management of pericardial effusion. World J Cardiol. 2011;3:135-43. 14. Pankuweit S, Ristić AD, Seferović PM, Maisch B. Bacterial pericarditis: diagnosis and management. Am J Cardiovasc Drugs. 2005;5:103-12. 15. Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005;112:3608-16. 16. Refaat MM, Katz WE. Neoplastic pericardial effusion. Clin Cardiol. 2011;34:593-8. Online only material Feb 25 2014 version 11 17. Holmes DR Jr, Nishimura R, Fountain R, Turi ZG. Iatrogenic pericardial effusion and tamponade in the percutaneous intracardiac intervention era. JACC Cardiovasc Interv. 2009;2:705-17. 18. Shabetai R. Pericardial effusion: haemodynamic spectrum. Heart. 2004;90:255-6. 19. Imazio M, Hoit BD. Post-cardiac injury syndromes. An emerging cause of pericardial diseases. Int J Cardiol. 2012 Oct 3. doi:pii: S0167-5273(12)01158-8. 10.1016/j.ijcard.2012.09.052. [Epub ahead of print]. 20. Figueras J, Barrabés JA, Serra V, Cortadellas J, Lidón RM, Carrizo A, Garcia-Dorado D. Hospital outcome of moderate to severe pericardial effusion complicating STelevation acute myocardial infarction. Circulation. 2010;122:1902-9. 21. Gilon D, Mehta RH, Oh JK, Januzzi JL Jr, Bossone E, Cooper JV, Smith DE, Fang J, Nienaber CA, Eagle KA, Isselbacher EM; International Registry of Acute Aortic Dissection Group. Characteristics and in-hospital outcomes of patients with cardiac tamponade complicating type A acute aortic dissection. Am J Cardiol. 2009;103:102931. 22. Imazio M, Brucato A, Rovere ME, Gandino A, Cemin R, Ferrua S, Maestroni S, Barosi A, Simon C, Ferrazzi P, Belli R, Trinchero R, Spodick D, Adler Y. Contemporary features, risk factors, and prognosis of the post-pericardiotomy syndrome. Am J Cardiol. 2011;108:1183-7. 23. Moreno R, Calvo L, Salinas P, Dobarro D, Santiago JV, Sanchez-Recalde A, Galeote G, Riera L, Moreno-Gomez I, Mesa J, Plaza I, Lopez-Sendon J. Causes of perioperative mortality after transcatheter aortic valve implantation: a pooled analysis of 12 studies and 1223 patients. J Invasive Cardiol. 2011;23:180-4. 24. Ristić AD, Seferović PM, Ljubić A, Jovanović I, Ristić G, Pankuweit S, Ostojić M, Maisch B. Pericardial disease in pregnancy. Herz. 2003;28:209-15. 12 25. Imazio M, Brucato A, Rampello S, Armellino F, Trinchero R, Spodick DH, Adler Y. Management of pericardial diseases during pregnancy. J Cardiovasc Med (Hagerstown). 2010;11:557-62. 26. Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007;297:1810-8. 27. Schairer JR, Biswas S, Keteyian SJ, Ananthasubramaniam K. A systematic approach to evaluation of pericardial effusion and cardiac tamponade. Cardiol Rev. 2011;19:233-8. 28. Pericardial effusion and cardiac tamponade. In Maisch B, Ristic A, Seferovic P, and Tsang T. Interventional Pericardiology. Springler 2011. 29. Beck C. Two cardiac compression triads. J Am Med Assoc. 1935;104:714-716. 30. Guberman BA, Fowler NO, Engel PJ, Gueron M, Allen JM. Cardiac tamponade in medical patients. Circulation. 1981;64:633-640. 31. Brown J, MacKinnon D, King A, Vanderbush E. Elevated arterial blood pressure in cardiac tamponade. N Engl J Med. 1992;327:463-466. 32. Kussmaul A. U ̈ ber schwielige Mediastino- Perikarditis und den paradoxen Puls. Berl Klin Wochenschr. 1873;10:433-435. 33. Bruch C, Schmermund A, Dagres N, Bartel T, Caspari G, Sack S, Erbel R. Changes in QRS voltage in cardiac tamponade and pericardial effusion: reversibility after pericardiocentesis and after anti-inflammatory drug treatment. J Am Coll Cardiol. 2001;38:219-26. 34. Eisenberg MJ, Dunn MM, Kanth N, Gamsu G, Schiller NB. Diagnostic value of chest radiography for pericardial effusion. J Am Coll Cardiol. 1993;22:588-93. 35. Woodring JH. The lateral chest radiograph in the detection of pericardial effusion: a reevaluation. J Ky Med Assoc. 1998;96:218-24. Online only material Feb 25 2014 version 13 36. Horowitz MS, Schultz CS, Stinson EB, Harrison DC, Popp RL. Sensitivity and specificity of echocardiographic diagnosis of pericardial effusion. Circulation. 1974;50:239-47. 37. Weitzman LB, Tinker WP, Kronzon I, Cohen ML, Glassman E, Spencer FC. The incidence and natural history of pericardial effusion after cardiac surgery--an echocardiographic study. Circulation. 1984;69:506-11. 38. Imazio M, Spodick DH, Brucato A, Trinchero R, Adler Y. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-28. 39. Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC Jr, Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO; American College of Cardiology; American Heart Association; American Society of Echocardiography. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary Cardiology/American Heart article: a Association report Task of the Force American on Practice College of Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003;108:1146-62. 40. Imazio M, Mayosi BM, Brucato A, Markel G, Trinchero R, Spodick DH, Adler Y. Triage and management of pericardial effusion. J Cardiovasc Med (Hagerstown). 2010;11:928-35. 41. Guntheroth WG. Sensitivity and specificity of echocardiographic evidence of tamponade: implications for ventricular interdependence and pulsus paradoxus. Pediatr Cardiol. 2007;28:358-62. 14 42. Gillam LD, Guyer DE, Gibson TC, King ME, Marshall JE, Weyman AE. Hydrodynamic compression of the right atrium: a new echocardiographic sign of cardiac tamponade. Circulation. 1983;68:294-301. 43. Schiller NB, Botvinick EH. Right ventricular compression as a sign of cardiac tamponade: an analysis of echocardiographic ventricular dimensions and their clinical implications. Circulation. 197;56:774-9. 44. Eisenberg MJ, Schiller NB. Bayes' theorem and the echocardiographic diagnosis of cardiac tamponade. Am J Cardiol. 1991;68:1242-4. 45. Fusman B, Schwinger ME, Charney R, Ausubel K, Cohen MV. Isolated collapse of left-sided heart chambers in cardiac tamponade: demonstration by two-dimensional echocardiography. Am Heart J. 1991;121:613-6. 46. Appleton CP, Hatle LK, Popp RL. Cardiac tamponade and pericardial effusion: respiratory variation in transvalvular flow velocities studied by Doppler echocardiography. J Am Coll Cardiol. 1988;11:1020-30. 47. Tsang TS, Oh JK, Seward JB, Tajik AJ. Diagnostic value of echocardiography in cardiac tamponade. Herz. 2000;25:734-40. 48. Himelman RB, Kircher B, Rockey DC, Schiller NB. Inferior vena cava plethora with blunted respiratory response: a sensitive echocardiographic sign of cardiac tamponade. J Am Coll Cardiol 1988;12:1470-77. 49. Mercé J, Sagristà-Sauleda J, Permanyer-Miralda G, Evangelista A, Soler-Soler J. Correlation between clinical and Doppler echocardiographic findings in patients with moderate and large pericardial effusion: implications for the diagnosis of cardiac tamponade. Am Heart J. 1999;138(4 Pt 1):759-64. 50. Bommer WJ, Follette D, Pollock M, Arena F, Bognar M, Berkoff H. Tamponade in patients undergoing cardiac surgery: a clinical-echocardiographic diagnosis. Am Heart J. 1995;130:1216-23. Online only material Feb 25 2014 version 15 51. Restrepo CS, Lemos DF, Lemos JA, Velasquez E, Diethelm L, Ovella TA, Martinez S, Carrillo J, Moncada R, Klein JS. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007;27:1595-610. 52. Gold MM, Spindola-Franco H, Jain VR, Spevack DM, Haramati LB. Coronary sinus compression: an early computed tomographic sign of cardiac tamponade. J Comput Assist Tomogr. 2008;32:72-7. 53. Kolski BC, Kakimoto W, Levin DL, Blanchard DG. Echocardiographic assessment of the accuracy of computed tomography in the diagnosis of hemodynamically significant pericardial effusions. J Am Soc Echocardiogr. 2008;21:377-9. 54. Alter P, Figiel JH, Rupp TP, Bachmann GF, Maisch B, Rominger MB. MR, CT, and PET imaging in pericardial disease. Heart Fail Rev. 2012 Mar 25. [Epub ahead of print]. 55. Sorajja P. Invasive hemodynamics of constrictive pericarditis, restrictive cardiomyopathy, and cardiac tamponade. Cardiol Clin. 2011;29:191-9. 56. Sagristà-Sauleda J, Angel J, Sánchez A, Permanyer-Miralda G, Soler-Soler J. Effusive-constrictive pericarditis. N Engl J Med. 2004;350:469-75. 57. Gascho JA, Martins JB, Marcus ML, Kerber RE. Effects of volume expansion and vasodilators in acute pericardial tamponade. Am J Physiol 1981;240:H49-H53. 58. Spodick DH. Medical treatment of cardiac tamponade. In: Caturelli G, ed. Cura intensiva cardiologica. Rome: TIPAR Poligrafica, 1991:265-8. 59. Hashim R, Frankel H, Tandon M, Rabinovici R. Fluid resuscitation-induced cardiac tamponade. Trauma 2002;53:1183-4. 60. Cooper JP, Oliver RM, Currie P, Walker JM, Swanton RH. How do the clinical findings in patients with pericardial effusions influence the success of aspiration? Br Heart J 1995;73:351-4. 16 61. Nugue O, Millaire A, Porte H, de Groote P, Guimier P, Wurtz A, Ducloux G. Pericardioscopy in the etiologic diagnosis of pericardial effusion in 141 consecutive patients. Circulation 1996;94:1635-41. 62. Sagristà-Sauleda J, Angel J, Permanyer-Miralda G, Soler-Soler J. Long-term follow-up of idiopathic chronic pericardial effusion. N Engl J Med. 1999;341:2054-9. 63. Hayashi T, Tsukube T, Yamashita T, Haraguchi T, Matsukawa R, Kozawa S, Ogawa K, Okita Y. Impact of controlled pericardial drainage on critical cardiac tamponade with acute type A aortic dissection. Circulation. 2012;126(11 Suppl 1):S97-S101. 64. Halpern DG, Argulian E, Briasoulis A, Chaudhry F, Aziz EF, Herzog E. A novel pericardial effusion scoring index to guide decision for drainage. Crit Pathw Cardiol. 2012;11:85-8. 65. Loukas M, Walters A, Boon JM, Welch TP, Meiring JH, Abrahams PH. Pericardiocentesis: A clinical anatomy review. Clin Anat. 2012 Jan 31. doi: 10.1002/ca.22032. [Epub ahead of print] 66. Fagan SM, Chan KL. Pericardiocentesis: blind no more! Chest. 1999;116:275-6. 67. Silvestry FE, Kerber RE, Brook MM, Carroll JD, Eberman KM, Goldstein SA, Herrmann HC, Homma S, Mehran R, Packer DL, Parisi AF, Pulerwitz T, Seward JB, Tsang TS, Echocardiogr. Wood MA. Echocardiography-guided interventions. J Am Soc 2009;22:213-31; quiz 316-7. Review. Erratum in: J Am Soc Echocardiogr. 2009;22:336. 68. Huang XM, Hu JQ, Zhou F, Qin YW, Cao J, Zhou BY, Zhao XX, Zheng X. Early diagnosis and rescue pericardiocentesis for acute cardiac tamponade during radiofrequency ablation for arrhythmias. Is fluoroscopy enough? Pacing Clin Electrophysiol. 2011;34:9-14. Online only material Feb 25 2014 version 17 69. Rafique AM, Patel N, Biner S, Eshaghian S, Mendoza F, Cercek B, Siegel RJ. Frequency of recurrence of pericardial tamponade in patients with extended versus nonextended pericardial catheter drainage. Am J Cardiol. 2011;108:1820-5. 70. Maisch B, Ristic AD, Seferovic PM, Tsang TS. Interventional Pericardiology: Pericardiocentesis, Pericardioscopy, Pericardial Biopsy, Balloon Pericardiotomy, and Intrapericardial Therapy. Springer Medizin Verlag Heidelberg 2011. 71. Ristić AD, Wagner HJ, Maksimović R, Maisch B. Epicardial halo phenomenon: a guide for pericardiocentesis? Heart Fail Rev. 2013;18:307–316. 72. Maisch B, Rupp H, Ristic´AD, Pankuweit S. Pericardioscopy and epic- and pericardial biopsy-a new window to the heart improving etiological diagnoses and permitting targeted intrapericardial therapy. Heart Fail Rev 2013;18:317-328. 73. Imazio M, Belli R, Beqaraj F, Giammaria M, Lestuzzi C, Hoit B, Lewinter M, Spodick DH, Adler Y. Drainage Or Pericardiocentesis alone for recurrent nonmalignant, nonbacterial pericardial effusions requiring intervention: rationale and design of the DROP trial, a randomized, open-label, multicenter study. J Cardiovasc Med (Hagerstown). 2013 Jul 17. [Epub ahead of print]. 74. Mayosi BM, Ntsekhe M, Bosch J, Pogue J, Gumedze F, Badri M, Jung H, Pandie S, Smieja M, Thabane L, Francis V, Thomas KM, Thomas B, Awotedu AA, Magula NP,Naidoo DP, Damasceno A, Banda AC, Mutyaba A, Brown B, Ntuli P, Mntla P, Ntyintyane L, Ramjee R, Manga P, Kirenga B, Mondo C, Russell JB, Tsitsi JM, Peters F, Essop MR, Barasa AF, Mijinyawa MS, Sani MU, Olunuga T, Ogah O, Adebiyi A, Aje A, Ansa V, Ojji D, Danbauchi S, Hakim J, Matenga J, Yusuf S. Rationale and design of the Investigation of the Management of Pericarditis (IMPI) trial: a 2 × 2 factorial randomized double-blind Mycobacterium w multicenter immunotherapy in trial of adjunctive tuberculous prednisolone pericarditis. Am Heart and J. 2013;165:109-15.e3. 18 75. Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34:1186-97. 76. European Society of Cardiology; Committee for Education; Authors/Task Force Members:, Gillebert TC, Brooks N, Fontes-Carvalho R, Fras Z, Gueret P, LopezSendon J, Salvador MJ, van den Brink RB, Smiseth OA; Observer on behalf of the UEMS (Cardiology Section):, Griebenow R; Review Coordinators:, Kearney P, Vahanian A; Contributors and reviewers:, Bauersachs J, Bax J, Burri H, Caforio AL, Calvo F, Charron P, Ertl G, Flachskampf F, Giannuzzi P, Gibbs S, Gonçalves L, González-Juanatey JR, Hall J, Herpin D, Iaccarino G, Iung B, Kitsiou A, Lancellotti P, McDonough T, Monsuez JJ, Nuñez IJ, Plein S, Porta-Sánchez A, Priori S, Price S, Regitz-Zagrosek V, Reiner Z, Ruilope LM, Schmid JP, Sirnes PA, Sousa-Ouva M, Stepinska J, Szymanski C, Taggart D, Tendera M, Tokgözoglu L, Trindade P, Zeppenfeld K; ESC staff:, Joubert L, Carrera C. ESC Core Curriculum for the General Cardiologist (2013). Eur Heart J. 2013 Aug;34(30):2381-411. doi: 10.1093/eurheartj/eht234. Epub 2013 Jul 11. Online only material Feb 25 2014 version 19 Table 1s. Stages in the hemodynamic spectrum of cardiac tamponade. STAGE HEMODYNAMICS INCIPIENT or PRECLINICAL tamponade Pericardial pressure equals right atrial pressure but it is lower than left atrial pressure. INITIAL cardiac tamponade Pericardial pressure equals left atrial pressure. MODERATE tamponade Pericardial pressure is above 10-12 mmHg and an abnormal jugular pulse can be detected with signs of compression of right heart chambers. ADVANCED tamponade Sinus tachycardia with significant reduction of stroke volume, blood pressure, and evident pulsus paradoxus. 20 Table 2s Main echocardiographic signs for the diagnosis of cardiac tamponade with reported sensitivity and specificity (35-43). Sign Sensitivity Specificity Diastolic collapse of RA 50-100% 33-100% Diastolic collapse of RV 48-100% 72-100% Inferior IVC plethora 97% 40% RA= right atrium, RV= right ventricle, IVC= inferior vena cava. Online only material Feb 25 2014 version 21 Figure 1s. Electrocardiogram in a patient with cardiac tamponade. Please note low voltage and QRS-complex electrical alternans. 22 Figure 2s. Typical “water bottle” appearance with a large effusion and comcomitant left pleural effusion on chest x-ray. Online only material Feb 25 2014 version 23 Figure 3s. The role of echocardiography in selection of the approach for pericardiocentesis. A) Large pericardial effusion from the subxiphoid view: subxiphoid approach for pericardiocentesis should be applied. B) Large separation of pericardial layers from the apical view, but very small from the subxiphoid: pericardiocentesis using intercostal (apical) approach should be performed. C) loculated pericardial effusion with massive adhesions: surgical management is preferable option (subxiphoid pericardiotomy). 24 Figure 4s. Marked variations of mitral peak E velocities (>25%) during respiratory phases (panel A) and inferior vena cava plethora (panel B) are echocardiographic signs of cardiac tamponade (see text for explanation). Online only material Feb 25 2014 version 25 Figure 5s. Regional cardiac tamponade by a large hematoma after cardiac surgery. 26 Supplemental Video 1. Four chamber echocardiography view in a patient with cardiac taponade revealing swinging-heart and compression on the right-cardiac chambers. https://dl.dropboxusercontent.com/u/102100737/Echo%20-%20tamponade-4ch.avi Supplemental Video 2. Subcostal view in the same patient demonstrating large separation of pericardial layers and compression on the right atrium and the right ventricle. Pericardiocentesis would be possible both using subxiphoid and apical (intercostal) approach. https://dl.dropboxusercontent.com/u/102100737/Echo-tamponade-subcostal%20view.avi Supplemental Video 3. Bedside, echocardiography guided pericardiocentesis. https://dl.dropboxusercontent.com/u/6237405/Tamponade%20videos/Bedside%20pericard iocentesis.mp4 Supplemental Video 4. Combined echocardiography and fluoroscopy guided pericardiocentesis in the cardiac catheterization laboratory, utilizing epicardial halo phenomenon. https://dl.dropboxusercontent.com/u/6237405/Tamponade%20videos/Fluoroscopy%20gui ded%20pericardiocentesis.mp4 Online only material Feb 25 2014 version 27