Here are the Readings for Manage and respond to allergy
advertisement

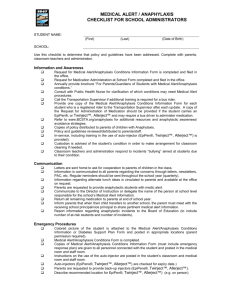
Manage and respond to allergy/anaphylaxis Identify and recognise signs, symptoms and key characteristics of allergy/anaphylaxis In this topic you will learn about food allergies and anaphylaxis. Anaphylaxis is a severe, life threatening allergic reaction. In most cases, anaphylactic reactions can be prevented with safety measures to avoid the known allergen, however, when anaphylactic reactions occur an emergency response is required. NSW Health indicates that it is likely that in NSW around 9 out of 10 child care centres may have at least one child with a food allergy enrolled, and around 2 out of 3 child care services may have at least one child with a peanut allergy. It is essential therefore that child care staff know not only how to prevent allergic reactions, but also how to act in an anaphylaxis emergency. The Australasian Society of clinical immunology and allergy (ascia) indicate that up to 40% of children in Australia and New Zealand are affected by allergic disorders some time during life, with 20% having current symptoms. Allergic diseases are on the increase, with some estimating they have just about doubled in western countries over the last 25 years. The most common allergic conditions in children are; food allergies eczema asthma and hay fever (allergic rhinitis). They are caused by immune system responses to otherwise harmless substances in our environment, such as pollen or house dust mites. When someone comes into contact with an allergen, their body has a reaction and they may display any of the following signs and symptoms: 1 © NSW DET 2007 cramps hives vomiting distress itchy ears/eyes loss of concentration swelling rash shock lethargy headache wheezing asthma cramps sneezing running nose itchy at site of contact shortness of breath rash anaphylaxis Reactions can be: Localised e.g. occurring at the site of contact with the allergen. An example of this might be where a child has brushed up against something in the garden that has affected them and so you may see swelling, redness or a rash at this site. Generalised –affecting parts of the body that have not been directly exposed to the allergen. An example of this is where the child has eaten something they are allergic to for instance peanut butter, and now has hives all over their body. Hives or welts (medically termed urticaria) are a red, itchy, raised skin rash, which can look like a group of mosquito bites an may be the first sign a person has an allergy. Although allergic reactions are common in young children, severe life threatening reactions like are uncommon and deaths are rare. Foods are the most common cause of allergies in infants and young children affecting around 5% of children under 3 years. While most children will outgrow their allergy, some will not. Many food allergies may become evident during the first 12 months when a child is given a food for the first time. This is why it is recommended that we introduce first foods slowly to the young child, one food at a time. This process makes it easier to identify the allergen and plan for the avoidance and treatment of the food allergy. Young child showing symptoms of allergic reaction: generalised hives on body and localised swelling of lips 2 © NSW DET 2007 Allergic reactions and anaphylaxis Anaphylaxis is a severe and sudden allergic reaction. It occurs when a susceptible person is exposed to a specific allergen (such as a food or insect sting). Reactions usually begin within minutes of exposure and can progress rapidly over a period of up to two hours or more. Anaphylaxis is potentially life threatening and always requires an emergency response. Anaphylaxis can occur at any age, but is most common in children and young adults. Allergy triggers Most commonly anaphylaxis may be triggered by foods such as peanuts, tree nuts, eggs, wheat, and cow’s milk. Less common food allergens are fish, shellfish, sesame and soy. Other substances that can trigger severe allergic reactions include medications (especially antibiotics), bee and other insect stings. Food allergy reactions almost always occur from eating the food or from touching the mouth with contaminated hands, utensils, toys or other objects. Signs of an allergic reaction Reactions can vary in severity but even mild symptoms can cause distress to the child. The signs and symptoms of a mild to moderate reaction may include: swelling of the face, lips and eyes rapid appearance of hives, itchy raised rash or welts on the skin abdominal pain and vomiting. The signs and symptoms of anaphylaxis may include one or more of the following: difficulty breathing; noisy breathing difficulty talking and/or hoarse voice swelling/tightness of the throat wheezing or persistent cough paleness and floppiness (in young children) collapse and/or unconsciousness. Although most food reactions are mild or moderate, a minority of reactions will require an emergency response. Peanuts, tree nuts, cow’s milk and eggs are the most common allergens responsible for triggering severe reactions in young children attending a children’s service. Most children grow out of cow’s milk and egg allergies before they reach school age or during the primary years, however, peanut, tree nut and seafood allergies tend to persist. 3 © NSW DET 2007 Activity 1 Apply organisation risk management strategies for children with allergy/ anaphylaxis As the most common allergies we will face in the child care service are related to food, our service approach to managing food allergies will centre on risk management strategies to prevent potentially serious reactions by avoiding exposure to the relevant allergen. The Australasian Society of Clinical Immunology and Allergy Inc (ASCIA) Guidelines note four steps in the prevention of food anaphylactic reactions for children’s services: 1. Obtaining medical information about children who may be at risk 2. Education of those responsible for the care of children concerning the risk of food anaphylaxis 3. Implementation of practical strategies to avoid exposure to known triggers, and 4. Age appropriate education of children with severe food allergies. Gathering medical information about anaphylaxis Activity 2 Action plans and medical kits Parents’ of a child with an allergic condition will need to provide the service with an Anaphylaxis Action Plan that has been developed with their doctor, prior to the child commencing in the service. Action plans provide instructions for staff on what to do if the child has an allergic reaction and must be updated regularly to ensure they are valid. Action plans include the child’s name and allergies, a photograph of the child and clear instructions on treating an anaphylactic episode. A standardised action plan that may be useful for children’s services is available from www.allergy.org.au 4 © NSW DET 2007 Depending on how serious the allergy is, the parent may also be required to provide a medical kit which will include the action plan and medication, including an adrenaline auto injector, EpiPen®. This needs to be brought to the service each day the child attends the child care centre. This medical kit must be stored out of direct sunlight and should be easily accessible in an emergency situation. Locking it in a cupboard or a room is not recommended as this will slow down any emergency response. Activity 3 The importance of education and training Managing anaphylaxis successfully in the centre will require all families’ staff and children to be informed about the seriousness of the condition and the steps the service is implementing to avoid a serious incident. Activity 4 Activity 5 Should all staff have anaphylaxis training? Services can consider whether all staff, or only certain identified staff, should have specific anaphylaxis training, so there is confidence about the service’s capacity to respond to an emergency situation. Anaphylaxis training should include: • • • • Awareness about those allergens that could cause a severe reaction Preventative measures to minimise the risk of an anaphylactic reaction Recognition of the signs and symptoms of anaphylaxis, and Emergency treatment, including practical training in the administration of an EpiPen®. Refresher training is advised every two years or when the needs of the service or the child/ren changes. This would include both the enrolment of a child at risk of anaphylaxis and when a child who is already attending the centre is diagnosed as at risk of anaphylaxis. In environments where food is provided for children at risk of anaphylaxis, cooks and other food providers should be fully informed about food allergy, risky food preparation procedures, cross contamination, and the options for nutritionally equivalent substitutes for potential allergens in recipes and food preparation. 5 © NSW DET 2007 Preventing anaphylaxis Should trigger foods be excluded from the centre? Many children’s services have developed policy to exclude foods such as peanut butter to prevent an identified child being accidentally exposed to a food contaminated with the allergen. Some have also excluded food products with ‘may contain traces of ...’ statements on the package. However, medical specialists agree that there is no risk from non-allergic children eating such foods in the vicinity of an identified child, unless there is direct sharing of the food. Any decision to exclude certain foods should be made in consultation with the identified child’s medical specialist. It should be made clear to parents and staff that, although allergen avoidance policies (sometimes called ‘nut free’ policies) are designed to reduce the risk of inadvertent exposure as far as possible, it is impossible to achieve a completely allergen-free environment in any service that is open to the general community. Strategies to prevent allergic reactions from occurring Where meals are provided by the child care service the following may be considered: • • • • for a severely allergic child, it may be preferable to have the parents provide meals prepared at home meals containing foods/ingredients that are labeled ‘may contain traces of nuts’, and similar, are not given to the identified child where the identified child is allergic to peanuts, tree nuts or shellfish, these foods may be readily excluded from the menu without compromising general dietary requirements sharing of food, containers and utensils should not be allowed. Where children are required to bring food from home for meals: • • sharing of food, containers and utensils should not be allowed eating areas and utensils should be thoroughly cleaned with warm soapy water, or put through a dishwasher cycle if appropriate, to remove traces of potential allergens. Special events The parents of a child with severe food allergy should be given advance notice of any special events. Events such as birthdays, excursions, cooking experiences all pose particular risks to the child with anaphylaxis and must be managed thoughtfully. 6 © NSW DET 2007 Child care services can reduce the likelihood of accidental exposure to food allergens by: Asking parents of all children not to send foods that contain the most common allergens for celebrations and occasions when food might be shared Asking parents of the child with severe food allergy to provide a treat box filled with a variety of items that the child or staff can choose from when a treat is required. They could also provide specially prepared cup cakes or muffins in a container with their child’s name clearly labelled on it to be frozen in readiness for any celebration that occurs in the child care service Making sure materials such as cow’s milk cartons, egg cartons or eggshells are clean and free of contamination before using for art and craft activities Being aware of the risk to an identified child of using allergenic foods in cooking activities (e.g. baking cakes, frying eggs) Keeping grassy areas mown, and reducing plants that attract stinging insects Working together with the parents of the identified child to gain a shared understanding of the level of risk in routine activities, such as cooking and craft, and the overall philosophy of inclusiveness for all children. Continuing education and awareness strategies. It will be vital for all staff, volunteers and students to be made aware of an individual child’s allergy condition and action plan. All staff should participate in anaphylaxis training and will need to know when and how to administer the adrenaline auto injector (EpiPen®) in the event of an emergency. Administer medication for anaphylaxis according to organisation policies and legislative requirements The importance of action plans in the management of anaphylaxis in the child care service has been mentioned previously. You will recall that action plans provide steps for staff to follow in an allergy emergency. Usually a child’s anaphylaxis action plan will indicate the need to administer a dose of adrenaline via an EpiPen®. EpiPen® is an emergency device which injects a dose of adrenaline into the thigh muscle in the thigh. It is used to treat severe allergic reactions (anaphylaxis). It contains one dose of 7 © NSW DET 2007 adrenaline. The drug adrenaline reverses the severe allergic reaction for example by reducing throat swelling, opening the airways, and maintaining blood pressure and can be lifesaving. EpiPen®. an example of an adrenaline auto-injector used to treat anaphylactic shock cli Training is required to administer the injection and should be given to all staff if a child, who may require this, attends the service. Giving this type of injection is a simple process but should be demonstrated and explained by a skilled staff member. Like Ventolin, Adrenaline requires a pre-arranged parental permission form to be signed. The anaphylaxis action plan tells you when you should give the EpiPen®. If your child develops an allergic reaction with any of the following symptoms you should use the EpiPen®; Difficulty/noisy breathing Swelling of tongue Swelling/tightness in throat Difficulty talking and/or hoarse voice Wheeze Persistent cough The EpiPen® should also be used if collapse or loss of consciousness develops in an allergic reaction. Be aware that young preschool age children may become pale and floppy without other symptoms and in this case the EpiPen® should be used. Remember: if you are in doubt it is better to use the EpiPen® unnecessarily rather than not treat a serious reaction. Staff may have concerns about administering this injection so services should consider purchasing a trainer EpiPen® so that staff can have regular practice with the device (purchase through Anaphylaxis Australia, http://www.allergyfacts.org.au/). Activity 6 8 © NSW DET 2007 Activity 7 Some final words about Epipen injectors Remember EpiPen®s can only be used once. Once the device has been used it needs to be replaced As with all emergencies the service response to the anaphylaxis incident needs to be reviewed along with service policies and procedure. Staff should reflect on whether the emergency could have been avoided? Summary An allergy is a sensitivity and an immune response to a usually harmless substance Anaphylaxis is a severe, life threatening form of allergic response. The growing incidence of allergies in our community means that it is vital that child care workers have a sound awareness of their roles and responsibilities with relation to not only the prevention of anaphylaxis but the identification of and emergency response to an anaphylaxis emergency. Additional resources The Australasian Society of Clinical Immunology and Allergy Inc (ASCIA) has developed an action plan for anaphylaxis available at: www.allergy.org.au Anaphylaxis Australia has produced a fact sheet “Starting Kinder or Preschool with Food Allergies” available at : http://www.allergyfacts.org.au/PDF/AAI%20Starting%20preschool.pdf Think F.A.S.T Poster A3 poster alerting people to the seriousness of anaphylaxis, the signs and symptoms that may appear available for purchase from Anaphylaxis Australia . Mailing address: PO Box 3182 Asquith NSW 2077. Web www.allergyfacts.org.au Email coordinator@allergyfacts.org.au Fax (02) 9482 4113 9 © NSW DET 2007 NSW Health Anaphylaxis guidelines for children's services: http://www.community.nsw.gov.au/docswr/_assets/main/documents/anaphylaxis_guidelines. pdf 10 © NSW DET 2007