Prof. Marc Miserez Prof. R.J. Fitzgibbons Prof. Volker Schumpelick
advertisement
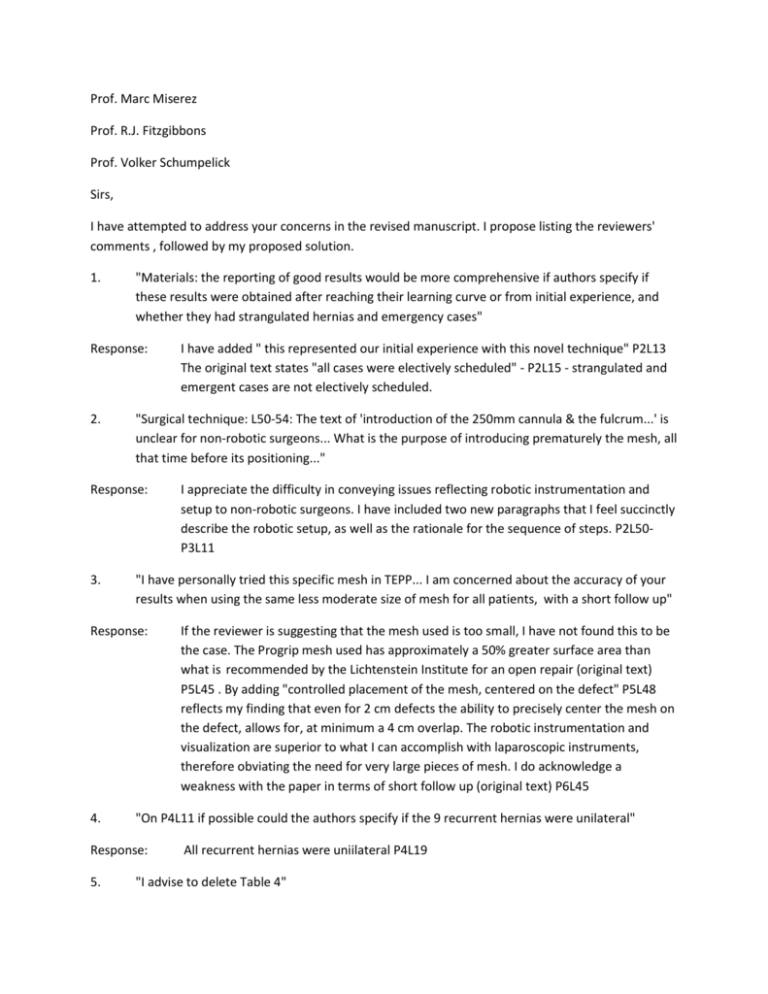
Prof. Marc Miserez Prof. R.J. Fitzgibbons Prof. Volker Schumpelick Sirs, I have attempted to address your concerns in the revised manuscript. I propose listing the reviewers' comments , followed by my proposed solution. 1. "Materials: the reporting of good results would be more comprehensive if authors specify if these results were obtained after reaching their learning curve or from initial experience, and whether they had strangulated hernias and emergency cases" Response: 2. "Surgical technique: L50-54: The text of 'introduction of the 250mm cannula & the fulcrum...' is unclear for non-robotic surgeons... What is the purpose of introducing prematurely the mesh, all that time before its positioning..." Response: 3. If the reviewer is suggesting that the mesh used is too small, I have not found this to be the case. The Progrip mesh used has approximately a 50% greater surface area than what is recommended by the Lichtenstein Institute for an open repair (original text) P5L45 . By adding "controlled placement of the mesh, centered on the defect" P5L48 reflects my finding that even for 2 cm defects the ability to precisely center the mesh on the defect, allows for, at minimum a 4 cm overlap. The robotic instrumentation and visualization are superior to what I can accomplish with laparoscopic instruments, therefore obviating the need for very large pieces of mesh. I do acknowledge a weakness with the paper in terms of short follow up (original text) P6L45 "On P4L11 if possible could the authors specify if the 9 recurrent hernias were unilateral" Response: 5. I appreciate the difficulty in conveying issues reflecting robotic instrumentation and setup to non-robotic surgeons. I have included two new paragraphs that I feel succinctly describe the robotic setup, as well as the rationale for the sequence of steps. P2L50P3L11 "I have personally tried this specific mesh in TEPP... I am concerned about the accuracy of your results when using the same less moderate size of mesh for all patients, with a short follow up" Response: 4. I have added " this represented our initial experience with this novel technique" P2L13 The original text states "all cases were electively scheduled" - P2L15 - strangulated and emergent cases are not electively scheduled. All recurrent hernias were uniilateral P4L19 "I advise to delete Table 4" Response: 6. "P4L29 delete the "i" in the word was. L36: it would be better to add the percentage into brackets" Response: 7. I agree with the concern over port site herniation. Why exchange one hernia for another? From the beginning I spent time carefully closing the fascia to mitigate the risk. I have been aware of the small bite - short stitch concept and have employed this, even though it added to the overall length of the procedure. I have added description P3L52 to emphasize the importance of meticulous closure technique. As a side note, I have had one port site hernia that developed in a cholecystectomy patient, in nearly 100 combined single site cases that I have performed. "Why not inserting the port site transumbilically, ensuring better cosmetic outcomes, and probably less incisional port hernia compared to lateral placement compared to lateral placement of the single port" Response: 9. Changes made P4L35 and P4L42 "No port site hernias?? Be precautious... authors had only 15% obese patients: could it be of the reason?" Response: 8. Table 4 has been deleted I have clarified the location of the fascial incision based on "in order to efficiently complete the proximal peritoneal flap dissection" P2L59-P3L6. There was never any mention made of a lateral port placement. I am unsure of what the reviewer is questioning. " Discussion: Despite the improvement of the promissing challenging robotic single port surgery, the cost effectiveness has not been assessed, compared to the higher price of the mesh, cost of the single port, cost of the robotic accessory, longer operative time to the low-cost of conventional laparoscopic surgery. Authors did not include in this article an assessment of cost but I hope it would be done in the near future" Response: First, this is a descriptive paper showing that a novel technique is safe and effective. Second, cost is highlighted as an important consideration, and in the original text time equivalence to laparoscopic TEP and TAPP was shown, P6L24, as it is clear that operative time is a substantial contributor to overall procedural costs. This is not a "longer operative time" procedure as suggested by the reviewer. I agree that cost issues need to be evaluated. I encourage the reviewers to look at data emerging from several institutions - Green Bay, Minneapolis among others showing that when you compare robotic single site cholecystectomy to laparoscopic cholecystectomy, the robotic technique represents a higher contribution margin to the hospital and is less costly for the patient. There are efficient systems that can bend the cost curve down, making robotics the more financially attractive modality. 10. "Two long in my opinion, and could be limited to 2 major messages" Response: I tried to increase the description and precision of the text, but was not successful in making it substantially shorter. I clarified the important message that RASS-TAPP is safe and should be evaluated further, as well as highlighting a potential advantage of this technique over all other modalities of inguinal hernia repair, less risk of chronic pain. Summary: This was not mentioned by the reviewers, but I have reorganized the structure of the Discussion, that I now feel is more cogently presented and easier to follow. I appreciate the opportunity to revise the manuscript, and the time the reviewers spent on the paper. Since I submitted this, there appears to be an increasing level of awareness and enthusiasm for RASS-TAPP and I hope that you will allow this to reach a much larger audience in Hernia.