Lot 3 Emotional Wellbeing Service Spec
advertisement
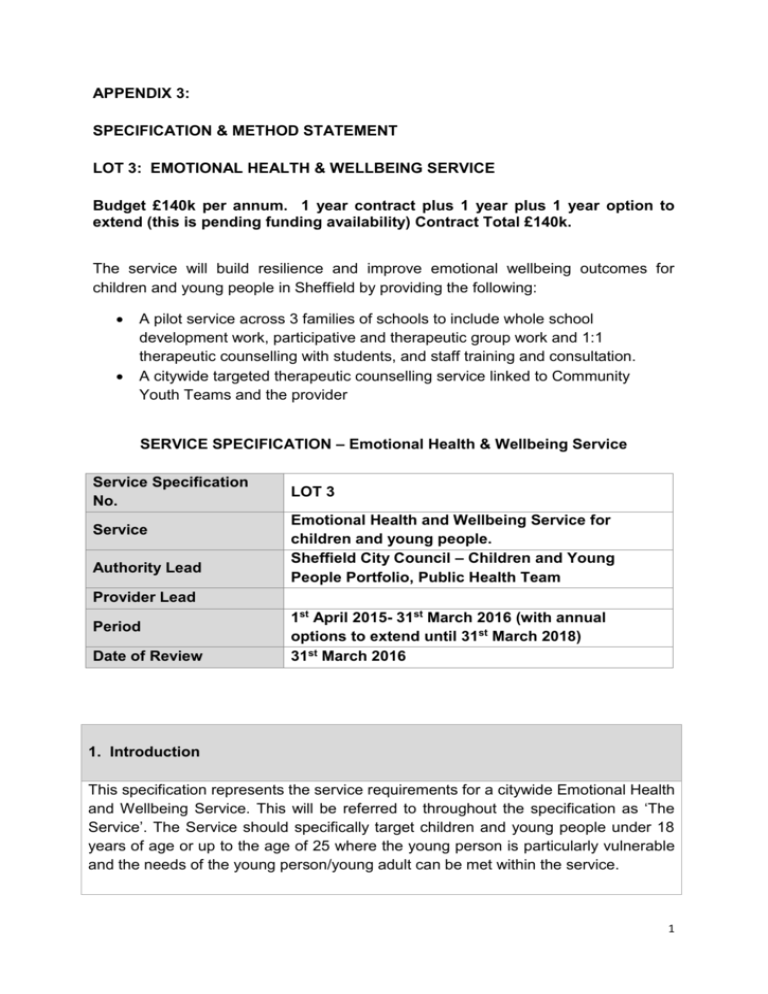
APPENDIX 3: SPECIFICATION & METHOD STATEMENT LOT 3: EMOTIONAL HEALTH & WELLBEING SERVICE Budget £140k per annum. 1 year contract plus 1 year plus 1 year option to extend (this is pending funding availability) Contract Total £140k. The service will build resilience and improve emotional wellbeing outcomes for children and young people in Sheffield by providing the following: A pilot service across 3 families of schools to include whole school development work, participative and therapeutic group work and 1:1 therapeutic counselling with students, and staff training and consultation. A citywide targeted therapeutic counselling service linked to Community Youth Teams and the provider SERVICE SPECIFICATION – Emotional Health & Wellbeing Service Service Specification No. Service Authority Lead LOT 3 Emotional Health and Wellbeing Service for children and young people. Sheffield City Council – Children and Young People Portfolio, Public Health Team Provider Lead Period Date of Review 1st April 2015- 31st March 2016 (with annual options to extend until 31st March 2018) 31st March 2016 1. Introduction This specification represents the service requirements for a citywide Emotional Health and Wellbeing Service. This will be referred to throughout the specification as ‘The Service’. The Service should specifically target children and young people under 18 years of age or up to the age of 25 where the young person is particularly vulnerable and the needs of the young person/young adult can be met within the service. 1 The Provider must deliver a programme of activity that is evidence based and complies with national policy, legislative frameworks and best practice models from across the UK. In addition the provider should also build on a range of local work which has been undertaken to understand and explore Children and Young people’s Emotional wellbeing and mental health needs in Sheffield and effective service response. In summary this work includes (with brief findings): Children’s Emotional Wellbeing and Mental Health Needs Assessment o 50% of lifetime mental illness (except dementia) arises by age 14 o There are inequalities in mental health need and access to services and these are related to deprivation and ‘at risk’ group e.g. Looked After Children, NEETs, SEN, substance misuse, LGBT and children of parents with a mental health disorder o Tier 1 and Tier 2 EWB&MH provision is not clearly articulated, can be limited in scope and disjointed, and the boundaries (and pathways) between the Tiers are not clear o Evidence of rising levels of need from Every Child Matters survey, increasing CAMHS referrals and increasing presentations of self-harm MAC UK (mental health charity specialising in working with gangs and youth violence) led a stakeholder review of the mental health system in Sheffield from the perspective of the most vulnerable children and young people and found: o A strong consensus for a team around the keyworker approach to support mental health, where the worker ‘bridges’ a relationship to another professional as opposed to referring them on Schools Emotional Wellbeing pilot in Sheffield Park Academy, Jan – July 2014 o Vulnerable children and young people present at school with high level needs for emotional wellbeing support, e.g. self-harm, depression, low self-esteem, sexual exploitation, bullying, bereavement, family breakdown, inappropriate relationships which are not responded to by a mental health service and do not meet the threshold for CAMHS o A whole school approach for Emotional wellbeing with targeted support wrapped around the school is effective in improving students mental wellbeing and behaviour o There are a number of recommendations for further development work, there would be benefits from an extended pilot to explore these The findings from the Right Here programme: a voluntary sector led partnership which worked with children and young people aged 16-25, with a focus on those more at risk of developing poor mental health and who may find it harder to access support (September 2009 – October 2013). The 2 programme recommended: o An integrative approach to young people’s mental health – based on young people’s needs and supported by the development of positive relationships o Young people’s involvement in mental health provision as a principle, including the design, delivery and evaluation of services o Creating opportunities for discussions around mental health o The importance of relationships and building social capital through group work opportunities o The effectiveness of therapeutic group work interventions Initial work from the Children’s Emotional Wellbeing and Mental Health Strategy Group has identified organisational and strategic priorities including promoting resilience and early intervention and improving support for 16-25 year olds in transition to adulthood Recent Child Death Overview Panel review of teenage suicides has recommended more accessible, flexible and creative emotional wellbeing and mental health responses to young people carrying complex vulnerabilities into their transition into independence and adulthood Consultations with Young Carers repeatedly highlight emotional wellbeing and mental health support as a key need for this group The Service design should be built from the learning and context above and rest on the following principles: That therapeutic intervention in this context is about supporting children and young people’s response to everyday life events and building resilience – it is not about treatment of mental health disorders. It is about universal prevention as well as early intervention for positive mental health. The Service actively bridges children and young people back into universal or targeted (non-mental health) provision as part of a robust step-down or stepacross process The Service is operating in a mental health system in which need and demand exceed capacity. The service will be required to work creatively with partners (e.g. Schools, MAST, CYTs, CAMHS and School Nursing Service), and to target activity carefully to make the best use of resources That a core commissioning and strategic outcome of the Service delivery in 2015/16 is about protecting existing emotional wellbeing support; exploring what works and where the gaps and strengths are within the system to be able to improve provision in subsequent years. Building relationships within this emotional wellbeing and mental health system is part of the process of this work. 3 There are two core components of the service specification: 1 Emotional Health and Wellbeing Service (schools – universal and targeted): Extended pilot of schools based emotional wellbeing service provision with up to 3 families of schools. This will run in tandem with the piloting of MAST Integrated Hubs (due to commence in April 2015) where MAST services are wrapped around families of schools. Whole-school staff training and development support around emotional wellbeing, developing the ‘in-house’ response, referral pathways and system relationships Participative and therapeutic group work targeted at vulnerable or ‘at-risk’ groups and transitions e.g. Y6 – Y7 1:1 therapeutic interventions, including bridging into other services as appropriate (e.g. to CYTs, CAMHS) Service weighting approx. 45% 2 Emotional Health and Wellbeing Service (Citywide targeted) 1:1 therapeutic counselling and group work emotional wellbeing provision linked to Community Youth Teams and Young Carers Support Service (8-19 year olds, up to age 25 if additional needs present and this is the most appropriate service) To include bridging back to schools, further education, training or employment and into other services as appropriate Service weighting approx. 55% This will be commissioned as one service for one year with the option of extending on a one year basis for up to 2 further years, dependent on outcomes. 2. Population Needs A Health Needs Assessment (HNA) has recently been completed for children and young people’s emotional wellbeing and mental health. The Executive Summary is included as an appendix and the full document can be accessed here: https://www.sheffield.gov.uk/caresupport/health/health-wellbeing-board/what-theboard-does/JSNA/positionstatement.html The HNA uses a range of local and national data, including stakeholder views to present a picture of the current emotional wellbeing and mental health needs of children and young people and the service provision to meet that need. It 4 demonstrates that there is some evidence for increase in need and definite evidence for an increase in demand on services. This service is being commissioned to sit across Tiers 1 and 2 of the mental health system in order to provide universal and targeted interventions for emotional wellbeing and mental health, particularly targeting adolescence. The widening gap between physical and sexual maturity and adult social and financial independence has been offered as an explanation for growing mental health and behavioural issues amongst young people. There is a surge of brain development in early adolescence, continuing into early 20s, and this brings with it a great potential for building lifelong wellbeing and resilience. The Service will respond to protective factors, risk factors and particular populations that are at risk of poor emotional wellbeing and mental health, further details are given in the HNA. Protective factors include school attendance, GCSE achievement and participation. Risk factors include deprivation, family breakdown, domestic violence, school factors such as absence, exclusions, bullying (behavioural indicators). At-risk populations include LAAC, SEN, Substance misuse, NEETS, young carers, LGBT, and young people at risk of offending or anti-social behaviour. There is an emerging discourse around positive mental health nationally and locally e.g. 5 ways to wellbeing; resilience; everyone has mental health (Right Here); which the Provider will build upon to reduce stigma and further develop informal support structures around mental health. 3. Key Service Outcomes 5 The Provider will deliver the outcomes required as demonstrated by the achievement of the key performance indicators listed in the table below: Outcome Demonstrated by The emotional wellbeing and resilience A flexible service offer which includes of vulnerable children and young people 1:1 therapeutic work, including is improved by being able to access counselling; therapeutic and therapeutic interventions appropriate to participative group work their needs Validated outcome monitoring scales tracking the progress of each client receiving an intervention. Individuals demonstrate improvement in personal wellbeing; family and close relationships; school and peer relationships. They demonstrate reduced risk and vulnerability, and improved behaviour. A specific referral pathway between participating schools and the Emotional Wellbeing service A specific referral pathway between Community Youth Teams and the Emotional Wellbeing Service A specific referral pathway between Young Carers Support Service and the Emotional Wellbeing Service A flexible support offer which provides short term, medium term and long term opportunities for service access and engagement The Service and it’s relationships with partners (e.g. Schools, MAST and Community Youth Teams) is underpinned by robust service level agreements, including safeguarding, confidentiality and data protection procedures The Service operates as part of the mental health system and pro-actively engages in strategic and development activity to add to the evidence base and improve the overall mental health support offer for children and young people in Sheffield 6 DNA rates for the service remain low because children and young people receive a high quality individualised service informed by their own views and feedback. Children and young people who are at The use of participation and therapeutic risk of poor emotional wellbeing are group work to support the building of supported to build their resilience relationships and social capital with children and young people who fall into at-risk populations for poor emotional wellbeing Children and young people at risk of The Service works pro-actively to poor emotional wellbeing are supported support the participating schools to at times of transition – into the service, bridge children and young people into between schools, services and into adult the service and to ensure resilience services strategies are taken back into the classroom The Service actively adopts a bridging model to support transition and engagement with other service providers, including CAMHS The Service designs, pilots and evaluates a support package for vulnerable children transitioning between primary and secondary school, specifically to support their wellbeing and resilience The Service designs, pilots and evaluates a support package for vulnerable young people transitioning between school and further education, employment or training, specifically to support their wellbeing and resilience Children and young people are involved Training to support young people’s in service design, delivery and involvement in service design delivery evaluation as the experts in their own and evaluation mental health The use of peer based group work approaches with full partnership working between the delivery practitioners and young people The use of participation models that are relevant to young people and to the organisation to create meaningful 7 Schools, community youth teams and the Young Carers Support Service are using evidence based approaches to improving their ‘in house’ support for children and young people’s mental health There is a reduction of stigma around mental health The service is able to be flexible and respond to changes in resource and demand opportunities School, Community Youth Team and Young Carers Support Service staff are trained and supported to develop their capacity to respond to children and young people’s mental health Working with participating schools and agencies to ensure that all children and young people have the opportunity to talk about and explore their own mental health A tailored support package for participating schools, community Youth Teams and Young Carers Service to meet need. Flexible and responsive service Ability to scale-up activity with corresponding resource if further schools wish to co-commission the service 3. Scope Service description The Provider is responsible for the overall delivery, implementation, monitoring and evaluation of the Emotional Wellbeing Service. The Provider will be responsible for ensuring the service requirements below are achieved. 1. Emotional Wellbeing service (3 families of Schools – universal and targeted) The exact model of provision will need to be negotiated by the provider with the schools concerned but should broadly include the following: Whole staff training and development to develop the ‘in house’ universal or first line response to students emotional wellbeing and mental health: o Key members of staff to be empowered to lead on emotional wellbeing and mental health; coaching and consultative support to develop this role o Whole staff introductory level training (in order to access further training, counselling support etc to ensure appropriate referrals) o Access for the whole staff team to good quality, flexible and responsive training and professional development 8 o Support to develop in- house referral pathways into targeted provision o A focus on developing peers and teachers response Participative and therapeutic group work provision – continue to build evidence base and explore different options, models or targeting in partnership with the school. o Explore prevention work with vulnerable groups; early intervention targeted work including self-referral; transitions y6 – y7; Y11- further education and work; any other key themes identified by the school (e.g. bereavement, healthy relationships, self-harm etc.) o Support school pastoral team to develop group work opportunities 1:1 therapeutic work with students o Therapeutic intervention in this context is about supporting children and young people’s response to everyday life events and building resilience. 2. Emotional Wellbeing Service (Citywide targeted) 1:1 therapeutic counselling; participative and therapeutic group work with children and young people identified by Community Youth Teams as having emotional wellbeing needs that cannot currently be met by core Community Youth Team provision 1:1 therapeutic counselling for Young Carers identified by the Young Carers Support Service and referred into the Emotional Wellbeing Service via an agreed robust pathway Work in partnership with CAMHS and Primary Mental Health Workers to ensure capacity building and development support to develop the ‘in house’ response of CYTs to young people’s emotional wellbeing and mental health needs. The Service will adapt a ‘Team Around the key Worker Approach’ to work with children and young people reluctant to engage or where there are a range of professionals already involved or where this will support transition and step down. Referral Pathway to the Emotional Wellbeing Service The Provider will develop a referral pathway and work collaboratively with participating schools and wider agencies (e.g. MAST, CYTS, School Nursing Service, Young Carers Support Service) to develop robust pathways. The Provider will actively adopt a ‘bridging’ model (as defined by MAC-UK) which helps build capacity in front line organisations and schools. Service evaluation The Service is being commissioned in the context of a developing mental health 9 system and wider health and social care re-organisations. As such the service will adopt a flexible delivery model which can respond to changing needs in the wider system. Learning from the first year of the Service will be fed into wider policy changes and will inform future commissioning. The Provider will ensure that there are robust monitoring and evaluation processes in place to learn from both the interventions and the process of delivery. This means that the evaluation will have a range of components: o Outcomes monitoring tools which are applicable across the service and enable comparison with other services in the future o Outcomes monitoring by participating schools, Community Youth Teams and Young Carers Service of the cohort of children and young people that receive interventions – to look at outcomes around behaviour, engagement, attendance, reduction of risk-taking behaviour etc. o Stakeholder feedback from across the partner agencies (e.g. Schools, MAST, CYTs, CAMHS) o Stakeholder feedback from children and young people, including universal feedback from schools o Outcomes from training o Whole school/Community Youth Teams/Young Carers Service impact of the Service o Demonstration of ongoing reflection on challenges and successes and Service response to these. Interdependencies with other services The diagram below demonstrates the inter-relationships of emotional wellbeing support with other provision. This service includes training and development to support universal capacity building in schools, 1:1 interventions and participative and therapeutic interventions for children and young people’s emotional wellbeing. As described above the Service is part of an emotional wellbeing and mental health system and the Provider is required to pro-actively work with partner agencies, this will be facilitated by SCC as Commissioner. 10 Service Mobilisation The Provider will be expected to produce a service mobilisation plan and will work closely with the Commissioner to ensure smooth implementation. Service Development The Service will provide the Commissioner with annual delivery plans which are based on direct consultation with children, young people and stakeholders and analysis of need utilising national, local and service user profile data. Within the first three months the Provider should develop an action/project plan which details how they intend to implement actions outlined in the service specification including the successful achievement of all key performance indicators. The plan should also include key milestones, target areas and how the process for evaluating the Service. This action/project plan should be developed and agreed in consultation with partners and signed-off by the Commissioner. Equality and Diversity The Provider must have a policy regarding Equality and Diversity. The provider must adhere to the policy to ensure that it does not discriminate against children and young people or adults on the basis of their gender, race, disability, sexual orientation, age 11 or religious belief. The provider must comply with the Disability Discrimination Act and monitor compliance. The Provider must contribute to carrying out, and it must monitor and act on the findings of Equality Impact Assessments on the provision of the Service. Quality Principles The Service will adopt and evidence the use of a Quality Framework and ensure that they provide annual case audits based on themes identified in partnership with the Commissioner. Contract Management Performance Monitoring The Provider will ensure all monitoring data that is submitted is accurate and complete and within the defined timescales of this contract. This will be based on a Performance Framework developed by the Commissioner and Provider and agreed prior to contract commencement. This will include a focus on outcomes and journey travelled whilst in the Service as well as output and finance management. This will be reviewed by the Commissioner and the Provider annually. Quarterly monitoring meetings will take place with the Provider and Commissioner at which the provider must provide a monitoring report. These meetings will provide a forum to discuss the on-going development of the service and resolve any difficulties or performance issues. The Provider will submit quarterly performance monitoring /activity data and Equality Impact Assessment monitoring data in the agreed format for the Service no later than 4 weeks following the end of the quarter. This contract will be reviewed annually in conjunction with the Provider and will include review of the service, scope and scale, local milestones, targets and context. Other Issues All children/young people should be contacted within 5 days of being made known to The Service. All personal identifiable data (client records/pledges) stored securely in line with the Data Protection requirements The Provider should note that the data they supply may be used by Sheffield City Council and other agencies for Data quality Reviews, Contract and Performance Management, Health Needs Assessment & Epidemiological studies, Resource Allocation, Audit, Clinical Audit, Research, Service Planning & Delivery, Strategy formulation. 12 The Provider will ensure that appropriate security & confidentiality measures are in place for the handling and transit of data at all times. The Provider will ensure that consent is obtained from children/young people/carer/parent by proxy to ensure that they understand the provider will hold their personal information and may contact them in the future to assess long term impact of the service. Tools such as Gillick should be used to ascertain capacity to consent. 4. Applicable Service Standards Applicable national standards. This list is not exclusive. Ensuring quality - All staff must be appropriately trained and qualified to deliver the appropriate part of the Service. Staff Training/Qualification/Experience Audits must be completed annually and shared with the Commissioner. - The Provider should adhere to adhere to National guidance and legislation to ensure the continuous improvement of the quality of their services, demonstrating this clearly utilising a validated Quality Standards framework underpinned by validated assessment and evaluation tools - The Provider will ensure at least 2 rounds of case audits are undertaken annually Safeguarding The Service must adhere to national and local safeguarding procedures and all staff must receive training on how to take action on any safeguarding concerns. This must be demonstrated annually to the Commissioner. In particular the Service will ensure that they work within the participating schools and agencies child protection and safeguarding polices (and others as appropriate) and draw up Service Level Agreements to reflect this. 5. Location of Provider Premises The location of service delivery will be flexible to meet the differing needs of service users. The service will be delivered in locations and venues, including community venues that are readily accessible and suitable for eligible service users. The Provider is expected to negotiate appropriate space for service provision within participating schools, Community Youth Team and Young Carers Service premises 13 as appropriate. The geographical location of the citywide service will be determined by the Provider. The Provider will be required to set out the planned geographical location of its service in its application to provide the service. Premises will need to be child/young person friendly and appropriate for delivery of 11 interventions and group work and provide an administrative base for the service. The Provider will demonstrate where appropriate a flexible approach to working in partnership with other services and organisations across a range of settings across the city to promote engagement and reduce barriers. 6. Inter-dependencies The Provider will develop and maintain good working relationships with other service Providers and local GP Practices, health professionals, local authorities and other statutory, voluntary and private groups. The service must ensure that policies and procedures relating to safeguarding are adhered to and managerial and administrative staff have undertaken safeguarding training appropriate for their professional role. It is vital that the Provider ensures that they have the necessary links with Children’s and Families Services in Sheffield so that access into these services is possible at appropriate times for appropriate children and young people. The Service will be an active Partner within the Emotional Wellbeing and Mental Health Strategy group and will ensure that they provide representation and influence strategy whilst supporting attendance and engagement of children and young people on the relevant Boards. The Service will provide evidence of the full range of services they actively engage with across children’s and adult services and will clearly demonstrate the value added in terms of outcomes. The service will demonstrate a step down approach to universal services across children’s, young people’s and adult services and will work with key strategic Boards and the Commissioner to develop robust pathways with other services. The Service will adapt a ‘Team Around the key Worker Approach’ to work with children and young people reluctant to engage or where there are a range of professionals already involved or where this will support transition and step down. Future proofing The Provider will be expected to work collaboratively with the broader agenda of improving healthy lifestyles and with public health colleagues in the NHS and in Local Authorities. This will include developing and maintaining strong partnership with: - Alcohol services Substance misuse services 14 - Mental Health Services Education Social Care Primary Care Preventative programmes – including participation and support in ad-hoc health promotion events organised within Sheffield. 15 Appendix I Service Consultation Date: 23/09/2014 12:30-14:00 This is a summary report capturing the output from a service consultation held on 23rd September 2014 between Sheffield City Council and the provider. The service is commissioned to provide targeted emotional health and wellbeing service to young people in Sheffield. The objective of this consultation was to understand the needs of young people in Sheffield in order to ensure that the service being commissioned is responsive and appropriate. In the interests of transparency and equality a summary of discussions during public consultations is to be included in the Invitation to Tender (ITT) documents. Why a competitive tender? A competitive tender process has been deemed necessary in the interest of being transparent and open. We will be measuring the specification uniquely to the needs highlighted as existing in Sheffield. Procurement milestones: ITT will go to market as a single stage process utilising Sheffield City Councils standing scoring matrix. The ITT will include the method statement. Top 3 scoring tenders will be taken through to the presentation stage. This will occur pre-award. The consultation discussions were organised around three key themes, to draw out expert knowledge and experience of working with particular groups of young people. Theme 1: Identification How do we identify Young People/Service Users? What are the barriers to identification? Which group remains hidden? Access/referral routes – consider time, venue and sources. Any gaps? Discussion points: A provider is commissioned by Sheffield City Council to provide targeted Emotional Wellbeing and Mental Health services in the form of counselling interventions. 16 Referrals are received from VOYCE (Views of Young Carers Explained), Community Youth Teams (CYTs), Youth Justice Service, and schools., Parent/carer and selfreferrals are limited due to funding restraints. Referrals are accepted depending on funding streams for different identified needs. Referrals from the following sources are not accepted under the current contract scope unless the provider purchases services via traded services: social care workers, MAST, Adult Mental Health (AMHS), Children & Adolescent Mental Health Services (CAMHs), Improving Access to Psychological Therapies (IAPT), Safeguarding, Special Educational Needs & Disabilities (SEND) or the voluntary sector. Appropriate referrals Some CYT where appropriate work closely with schools to decide how and when to refer a pupil to the service. Work is also undertaken to support school to understand individual need the services that are available to them i.e. Via PHSE lessons or assemblies Empowered young people are more likely to self-refer into the service. Evidence: Right Here programme this work included liaisons and informal consultations between referrers and the service. It 1) helped staff deliver 2) identify how and why to make an appropriate referral onto the service for counselling. Breaking down stigma is important, opening channels of communication and readiness to seek support amongst young people. The specification should consider how the provider works to breaking down stigma and facilitate access into the service. Hidden groups There are a number of hidden groups of young people who would benefit from a referral into these services, and although the service works with YP who are from these groups, there isn’t a direct referral route at present for some of the hidden groups, although clients may access the service via another funding route due to another specific presenting issue. These groups include: LGBT cohort – referrals from this group are increasing after 18 years of age however, referral rates remain low in younger years Sexually exploited young people can be referred via CYT if they are working with them Survivors of sexual abuse and incest, aged 18 and over. Young carers 17 Victims of crimes such as discrimination. Perpetrators of crime are referred from the Youth Justice Service however there is a gap for victims of crime. Young people from affluent areas - this cohort often feel isolated and feel unable to talk to those around them. This group are often affected by pressures to achieve. As they aren’t typically flagged in a high risk group e.g. risk of offending or under attainment, they often go unnoticed. Young people with special educational needs and disabilities, there is a need to adapt material and communicate at an appropriate level with this group. Asian young women. Eastern European young people. Children & young people from war torn parts of the world. o For some of the above groups there would be a need to consider the use of a translator where appropriate and consider the increased staffing cost to support this. Some of the identified vulnerable groups above maybe presenting via other routes and therefore, not coming to the attention as someone who could benefit from a referral into counselling. Better identification: how? Identification can be improved by breaking down stigma associated with accessing counselling services. For young people with special needs, generic SEND antistigma work is required. Mental Health ambassadors, STAMP (Support Think Act Motivate Participate) and participation groups can also contribute to having open discussions about the importance of emotional wellbeing amongst young people and wider society. Challenges to identification: access and referrals It is important for the service to be flexible and child / young person - centred when designing access and referral routes, and reflect need. Gaps and need of the service include: An increased demand for after-school counselling provision and a choice of venue (both closer to and from home). Self-referrals: how many are actual self-referrals and not directive prompts from others? Additional advertising material e.g. printing leaflets to raise awareness is not sustainable from a restrained budget in the long term One way to manage the waiting list for assessments is for the service to have some initial contact with the young person, to better understand demand and ensure that only appropriate referrals are advanced. “Meets and greets” or ‘triage’ with young person being referred in conjunction with CYT is useful to aid this. 18 Theme 2: Need What are the needs of this group? as a population as an individual in context How do these vary across demographics? Age, gender, ethnicity, parental factors, socio-economic and geographical factors Young person’s vulnerability Prioritise need/management demand As a population/individual/context, need varies for a number of factors. These include: a) Age of the young person; the service is accessible to 8-25 year olds. Needs vary accordingly with age and with developmental stages. For example, a 16 year old may have the developmental age of an 8 year old; young people at transitioning ages differ in their presenting need from both children and adults; the service must cater for this accordingly. b) Individual circumstances. A provider’s ability to be young person centred and adopt a flexible service delivery model is crucial to providing appropriate support to young people. Understanding a young person’s social environment is hugely beneficial. For example, seeing a young carer during school-time, as otherwise, a young carer would find it more difficult to engage with the service. Counselling should not be set and rigid but rather be an aid as part of a wider therapeutic process. This may require adapting the method of intervention delivery, such as allowing a young person to express themselves using art therapy if this cited as the preferred approach by the young person. It is important for the provider to be aware that the same therapy intervention will not suit or be appropriate to all. Practical needs Some young people do not have the means to attend the service without help. The most common way this is facilitated is through funding of bus-fare; this helps respond to the young person in their own context and aids engagement. Services need to be offered on premises suitable to the young person. Revolving door service? Unlike with adult services, young people’s choice to drop in and out of interventions is not necessarily a sign of disengagement or failure of the service. Often, young 19 people choose to engage at different times. Giving young people a choice of how and when to engage is paramount as it gives them control over their life, something which is not always possible in other aspects of their lives; where it happens re-entry into the service is often linked with key life events or changes. It is important for a provider of targeted emotional wellbeing for young people, to be in tune and reflect the needs of the presenting young person. If young people feel pressured that the intervention being offered is their only opportunity to get support, any disengagement with the service is likely to be long-lasting – this can be to the detriment of the young person’s emotional wellbeing. Another point for consideration is that short term time-limited interventions, whilst being easier to commission, may not necessarily be meeting the needs of young people. It is important to ensure that: - Access to services in the long term is possible and not to end this access prematurely There is realisation that some young people have complex needs and these require a considerable amount of engagement, trust-work and pre-therapy work from the referrer’s support before a targeted counselling intervention is possible. Theme 3: Response Access & Engagement across: Short term – Medium term – Long term Individual, group, peers, the family, wider system Exiting the service e.g. step down, follow up Social capital Social media/virtual service Clarification on what is meant by short term – medium term – long term response needs: Whilst appreciating that young people may have a long-term need for a counselling service, from the perspective of a commissioner there are budget restraints within which the provider will deliver a service. Therefore, we must consider how a young person is aided in stepping down and exiting the service with minimal disruption. The challenge is to bridge and support individuals over time, into service and onto other services and support functions, as most appropriate to reflect need. Social capital relates to having robust links with universal services and what is going on in a young person’s world. 20 Family context work - Statutory emotional wellbeing and mental health provision is family based (for the younger age group). This presents a gap for young person to be seen separately from that setting and focus specifically on their needs but without duplicating work of interventions offered elsewhere. - Parental attitudes to seeking outside help,/lack of awareness,/shame are a barrier to referrals - A young person can request a family member to be present during therapy but only with the young person’s consent. This is not always appropriate for many, as some young people do not want others to know they are receiving an emotional wellbeing intervention - Some “parents” may fall within scope for service - consideration for intergenerational work is required. It is important to relate this service to wider services: Creating a shared language to improve communication between agencies and which brings professionals together, as well as encouraging MH providers to co-create packages of support, thus enhancing care pathways. Some young people feel isolated from other mainstream mental health services on offer, i.e. difficulty in relating to generic literature and delivery modes as it is sometimes delivered in isolation of the specific circumstances of the presenting young person. The commissioned service must therefore, clearly respond to the needs of these young people. Building relationships (liaisons with universal and specialist services) and bridging young people and referrals/referrers. Commissioning for strategic influencing rather than just outcomes judged. A recommendation is to monitor and evaluate outcomes across services to identify need and styles (e.g. more collaborative working), that can be measured across services and ages ranges in a standardised way. Working alongside other agencies e.g. CYT and Educational Staff supports better engagement by the young person. Crisis management A provider of this service will manage young people presenting during a crisis. Some issues for consideration to ensure the service commissioned is effective in responding to presenting need of young people are: - It may not always be appropriate to refer a young person for another counselling intervention if the anxiety could be responded to and contained by the service workers who are familiar with the young person’s case. 21 - Consideration is needed on pathways into other services as the service is not funded to deliver 24/7 support; statutory services are set up to respond but may also be off-putting to young people. A young person with emotional wellbeing needs can frequently be moved around within the education and social care system. Maintaining a relationship with a therapist is key as it provides the young person with stability. The specification should consider how the commissioned service can continue a long-term relationship with a young person. What does long term support look like? - Consistency in branding of the provider service so young people are easily able to recognise it and associate with it. - Participation groups for young people to help maintain relationships and a support network - The provider offers various step down approaches to clients. This is recontracted with each individual client to ensure they are clear about the intervention they need to disengage from. - Remaining flexible and responsive to engaging with young person - Relationships may continue without a formal service provision - this long term support is achieved by young people choosing to build on friendships and support networks. - Acknowledging the straddling role this service plays i.e. between the children & adult worlds, health and social care, statutory and voluntary. - Tailor the service response to the expectations young people may have of the service. This has social capital implications which can be very severe if not managed well. - Recognising the unique nature of young people and their reality and responding to this Exiting the service: It is important to consider how a young person is supported to step-down and exit from the service. Primarily, making a young person aware of where additional support can be accessed and what form the support takes will facilitate their exit. Some points to consider are: - - The role of voluntary sector, which can provide specialist services on particular issues or generalist e.g. housing advice. Signposting a young person to these services can help contribute to a holistic support package to meet the needs of a young person. Training and raising awareness within schools of young people with emotional wellbeing needs can benefit the young person returning to a universal setting. A focus on how GP’s can help provide alternative support. 22 - There are gaps in other service support provision at certain ages. For example, Youth Justice input ends at 21 and young people who are also exiting a targeted emotional needs service may need additional considerations. Similarly, school leavers aged 16-18yrs exiting targeted services may need specific support to step-down without requiring another rereferral. Sometimes, a young person may require a more intensive intervention. The provider should therefore be aware that a young person engaging with the service will always move through it and exit. Young people can be actively engaged in helping to remove stigma amongst their peers and providing input on what a helpful intervention looks like. The provider currently facilitates volunteering opportunities for young people to help and engage other young people to raise awareness of the service. Considering social media/virtual services into service specification: Any social media involvement by the provider should be decided in conjunction with young people’s preferences. Although many young people are accustomed to using social media/virtual services to socialise and access information, it has not been a priority area for development as young people have not raised it as an issue. - - A telephone service for 16years + did not have a good impact or uptake. Skype technologies not favourable amongst service users Appointments for counselling sessions can be sent via text message, email or phone (all protected by safeguarding procedures). The service uses one consistent phone number which young people learn to associate with the provider. Finding a “private space” can be difficult for some young people and the organisations within which they are situated, for example, in a school setting Young people find building relationships, in person, very important; this enables building of communication skills and trust in relationships. Any additional considerations: [none raised] Appendix II Service Consultation Date: 23/09/2014 10:00-11:00 This is a summary report capturing the output from a service consultation held on 23rd September 2014 between Sheffield City Council and provider staff who are 23 commissioned to deliver TaMHS. The service is commissioned to provide capacity building training for staff in primary and secondary schools. The objective of this consultation was to understand the needs of young people in Sheffield in order to ensure that the service being commissioned is responsive and appropriate. In the interests of transparency and equality a summary of discussions during public consultations is to be included in the Invitation to Tender (ITT) documents. Why a competitive tender? A competitive tender process has been deemed necessary in the interest of being transparent and open. We will be measuring the specification uniquely to the needs highlighted as existing in Sheffield. Procurement milestones: ITT will go to market as a single stage process utilising Sheffield City Councils standing scoring matrix. The ITT will include the method statement. Top 3 scoring tenders will be taken through to the presentation stage. This will occur pre-award. The consultation discussions were organised around three key themes, to draw out expert knowledge and experience of working with particular groups of young people. Theme 1: Identification How do we identify Young People/Service Users? What are the barriers to identification? Which group remains hidden? Access/referral routes – consider time, venue and sources. Any gaps? Discussion points: TaMHS service is commissioned by Sheffield City Council to deliver universal emotional health and wellbeing training to school staff, in order to help meet the emotional wellbeing needs of children. Provision is in place for primary and secondary schools. There are two types of training courses on offer: 1. General core training- this training is entry level and aimed at staff to get a better understanding of the types of emotional wellbeing needs children may present with. It is not tailored to cover specific needs in depth. 24 2. Specialised training: more specific material tailored to inform school staff around particular emotional wellbeing needs that children may present e.g. ADHD The principles underlying both types of training courses remain the same however the delivery is tailored to reflect the presenting need at a particular school/school group i.e. amending for age-appropriateness of children that staff are working with. The manner in which capacity building training is delivered often differs in primary and secondary schools. In primary schools, it is more commonplace for schools to take a holistic whole-school approach and train the whole staff group including administration staff, support staff, teachers and senior management teams. This is made possible given the smaller size of primary schools compared with secondary schools. In secondary schools, a filter-down approach is often deployed by the school. This involves training being delivered to a specific staff group who are in particular need for the training, and later disseminated as deemed necessary. Location and duration of training courses - The location of the training delivered is negotiated with individual schools. Increasingly, it is being offered on school premises, although external venues are sometimes also sourced. Delivering training on school premises is practical (reduce commuting time of staff) and it can increase attendance. - Training sessions can be tailored to fit around school teaching time through the use of inset days or twilight sessions at the end of a school working day. - Often, training courses are delivered on a one-off basis though some schools do request refresher or additional capacity training to cover additional staff groups and/or receive specialised training for particular presenting needs of children. Currently, around half of the 180 schools in Sheffield have received at least one type of training, from TaMHS. Organising training: Proactive or Reactive? Schools approach TaMHS for capacity training – the commissioned provision is not compulsory to take-up by schools. In terms of managing demand, TaMHS will assess the request for training as it is received and providing a particular school is not requesting numerous sessions in a very short period of time, training is often scheduled in as requested; it is not uncommon for schools to plan in staff training into the school year, in advance. A more targeted approach by the service has been considered, however, a question of how to do this appropriately needs further exploration. Schools identified as having higher levels of need have been targeted however some have not taken up 25 the offer of training. There are several reasons for and often schools have a range of competing needs to address and a limited available timeframe to do so. Another possible form of proactive targeting is by geographical areas and type of youngster with presenting emotional wellbeing needs. For example, Looked After children are more clustered in particular parts of Sheffield and therefore, delivering capacity training to help school staff to react to presenting need of this group could be considered. Although there is potential benefit of having a structured approach to universal training delivery, providers need to be aware of the extent to which this kind of approach is best use of resources. Identifying Emotional Wellbeing Needs The main challenge for school staff is to see beyond the displayed behaviour and consider the emotional wellbeing needs from the perspective of the child. There are groups of children whose emotional well-being needs are often “hidden” and less apparent than those whose needs result in more demonstrative behaviours. Capacity training received by school staff seeks to address this through highlighting the range of needs and behaviours impacted by emotional wellbeing and mental health. These groups are difficult for school staff to engage with though it is important to recognise and become more aware of presenting needs of these children and young people in a universal approach. Hidden group: quiet and withdrawn children. The more disruptive children are often seen as more problematic in classrooms and capacity training requested by staff is often as a result of to help respond to this effectively. The quiet and withdrawn children will also have emotional wellbeing needs but can be overlooked due to the attention detracted away from them. Hidden group: children not engaging with schools (hospital and home tuition). Children and young people disengaged from mainstream schooling will have emotional well-being needs that school staff are not fully aware of and therefore, it is difficult to train staff on presenting need (as it is not always known). There are trends in the prevalence of emotional wellbeing needs in specialist schools compared to mainstream schools. Some of the main areas of need include Looked After Children, ADHD, Autism and PDA. The specification should reflect that this service being commissioned is for universal training provision; too much of a targeted approach will restrict the universality of the service on offer. Theme 2: Need 26 What are the needs of this group? as a population as an individual in context How do these vary across demographics? Age, gender, ethnicity, parental factors, socio-economic and geographical factors Young person’s vulnerability Prioritise need/management demand It is important for the training provider to be receptive to the needs identified by schools where the training is being provided. High level of engagement determines the usefulness of the training in the specific school areas/tailored to presenting need. One of the main needs for capacity training for school staff is to raise awareness of what and common specific emotional wellbeing needs are and how they affect children. This will help staff to become more knowledgeable of issues they may face when interacting with children and young people in schools. In recent times, specialist courses have been developed to reflect presenting need in schools. For example, Pathological Demand Avoidance syndrome (PDA) which is a subset of Autism Disorder. Culture in schools Schools have cultures and targeting school staff as early as possible with emotional wellbeing capacity training will undoubtedly influence a change in a school’s culture to one of a greater understanding and more appropriate response to presenting emotional wellbeing needs of children. Responsive capacity training helps develop a better working atmosphere amongst school staff, and enables staff to respond to and where necessary, “hold” the emotional wellbeing needs of children and young people whilst they are referred to specialist CAMHS services. This concept of bridging is important and should be included in the specification, as it shows that capacity training has far reaching beneficial implications. Can parents/carers of children with emotional wellbeing needs, benefit from training? Parents/carers of children with emotional wellbeing needs often face similar challenges at home as school when the child is at school. This is especially prominent in the cases of children with additional needs. How can training that staff receive, be filtered through to parents/carers, especially to adoptive/foster placement homes to prevent breakdown in relationships and placements? Kinship carers also currently miss out on this support. One suggestion made was that schools could possibly host sessions for parents to access input around young people’s emotional wellbeing and mental health. 27 Assessing need: outcome measures A follow up with schools to assess the extent to which staff found the capacity training helps their understanding and/or interaction with children with emotional wellbeing needs, is important. There are many ways of measuring outcome, and for the purpose of the specification, it is not in the interest of the commissioner to be very prescriptive in how this is managed. Some useful measures discussed which may be good indicators for assessing the usefulness and impact of the training delivered are: - - Measuring how confident staff who received the training feel in terms of understanding the presenting emotional needs of children and young people in their care Standardising evaluation method could allow for comparison and benchmarking against schools in Sheffield Availability of a toolkit to aid school staff in deciding how to approach presenting emotional wellbeing needs and also helping to signpost to the most appropriate referral route. This toolkit is publically available to schools and was commissioned by Sheffield city council in an attempt to have a directory of all services available in Sheffield for Emotional Wellbeing and Mental Health needs. Theme 3: Response Access & Engagement across: Short term – Medium term – Long term Individual, group, peers, the family, wider system Exiting the service e.g. step down, follow up Social capital Social media/virtual service Clarification on what is meant by short term – medium term – long term response needs: Whilst appreciating that emotional wellbeing need of children and young people in schools appears on a continuum and varies in duration and intensity, from the perspective of a commissioner there are budget restraints within which the provider will deliver a service. One of the main challenges facing universal capacity training in schools for emotional wellbeing of children is how to bridge and support individuals over time, into other services and support functions that may become more appropriate. 28 The remit of this commissioned service is to provide initial capacity training sessions on a universal level. Sometimes, a more targeted service may be necessary, in which case how and if a universal service signposts onto these should be considered in the specification. Considering social media/virtual services into service specification: Although the staff consulted felt online access to the services toolkit and other resources would be useful to easily obtain information, extending training sessions to a virtual environment was not recommended. Face to face training allows for staff to interact and engage fully with the material, other members of staff and the training provider all during protected time. The opportunity to have real-time input and a holistic view of presenting need is very important for capacity training to be effective and for this reason, the staff consulted strongly felt that this element of delivering training should remain unchanged. General point of clarification As the provision of universal and targeted Emotional Wellbeing and Mental Health services are joined into one tender, partnership working amongst multiple providers and/or across universal and targeted care provision are welcomed. Any additional considerations: [none raised] 29 Appendix III Children and Young People’s Mental Health Needs Assessment Executive Summary The purpose of this summary is to outline the findings from a Health Needs Assessment exploring the emotional wellbeing and mental health needs of children in Sheffield. The HNA will be used to inform the direction of the Emotional Wellbeing and Mental Health Strategy and future design and commissioning of services. Content is derived from national and local indicators, informed by the evidence base of protective and risk factors for emotional health and wellbeing. The report also considers service level data and self-reported measures from local surveys and consultations. 30 Population The scope of the HNA is 0-25 year olds, with a particular focus on Early Years and Adolescence as important periods of physical and emotional development. Preschool years involve children undertaking a number of important developmental tasks relating to their physical development, social and emotional development and language and cognitive development which all have an impact on later childhood. In regards to adolescence, the widening gap between physical and sexual maturity and adult social and financial independence has been offered as an explanation for growing mental health, and behavioural issues amongst young people. There is a surge of brain development in early adolescence, continuing into early 20s, and this brings with it a great potential for building lifelong wellbeing and resilience. The table below profiles the Sheffield population of Children and Young People as relates to usual divisions in service provision i.e. Early Years, 5-15s, 16 & 17 year olds, and 18-25 year olds. Prevalence of mental disorder and illness Mental disorders arise early in the life course and impact on a young person’s development and can stop them realising their potential. Furthermore mental disorders often last for a long period of time. It is recognised that 50% of lifetime mental illness (except dementia) arises by age 14 and 40% of young people experience at least one mental disorder by age 16. It is estimated that approximately 7000 5-15 year olds in Sheffield have a clinically recognisable mental health disorder. Prevalence data for Early Years is less clear but it estimated that approximately 10% of 0-3 year olds could have a mental health problems. It should be noted that local estimates of prevalence are based on extrapolated national data, some of which is 10 years old. We have good 31 local data around risk factors and protective factors, and access to services which can be used to complement prevalence estimates. Protective and Risk Factors, including at-risk populations Sheffield generally benchmarks around the national average for protective and risk factors, however this masks the wide inequalities experienced across the city – which reflect broader inequalities in health. The Relative Index of Multiple Deprivation can give an indication of cumulative risk factors for poor emotional wellbeing and mental illnesses. In Sheffield the population is clustered towards higher levels of deprivation, with a total of 34.2% of the Sheffield population living within the most deprived fifth of areas in England. This equates to 38,991 0- 17 year olds. Certain populations are at greater risk of poor emotional wellbeing and mental illnesses, for example LAAC, SEN, Substance misuse, NEETS (data relates to range of age ranges). An estimated 19 000 CYP fall into these categories. In Sheffield an estimated 15 000 CYP live with a parent with mental health disorder. 40% children experience insecure attachment which is also a risk factor for poor mental health. There are a number of factors which point to increased risk in early years compared to our statistical neighbours and England: there has been a recent decline in access to Free Early Learning, achievement of the Personal Social Emotional Development element of EYFS (also reflected in the Best Start Sheffield study) is low and the % inequality gap for EYFS – while similar to Y&H is low in comparison to England and our statistical neighbours. Service provision Emotional Wellbeing and Mental Health System Support for children and young people’s emotional wellbeing and mental health is articulated within the local policy context, both in terms of population mental health and commitment to commissioning intentions for service delivery at all Tiers. However, there is no whole system model of emotional wellbeing and mental health provision and this is recognised as a concern by stakeholders. The system is broader than that which is commissioned by NHSS CCG and SCC and there is potential for further investigation and quantification of the mental health impact of wider services. Tier 1 and Tier 2 provision is broad and disjointed, and the boundaries (and pathways) between the Tiers are not clear. The young person centred model of Mental Health services created by Right Here presents a view of the mental health system which is needs led and contrasts with the ‘service-led’ Tiers model. Presenting the Mental Health 32 system in this way would help articulate the CYP journey through the Mental Health system and may help identify gaps. The diagram below shows current services at each tier and estimated relative need (where the figures are available). Further discussion of provision at each tier follows. Becton(5-18y old) 15 day places 40 intensive outreach NEED 30 inpatient Clinically diagnosable mental disorder: (at any one time) Aldine House secure unit Est. 7000 5-15 year olds Est 16 000 16-24yr olds anxiety disorder CAMHS 1273 5-16 yr olds p.a. (comm, forensic,MAPS) Est 4500 16-24 year olds PTSD AMHS 1916 15-25 year olds p.a.(457 15-17yrs); Transitions Group; CD team MST (11-17y olds) caseload = 45 SYEDA = 47 CYP pa; Perinatal MH 200 women pa At risk populations e.g. LAAC, SEN, Substance misuse, NEETS (data relates to range of age ranges) Primary Mental health workers - 898 Est. 19 000 CYP approx MAST consultations Est .15 000 CYP with a parent with MH disorder 40% children experience insecure attachment Key risk factor: Deprivation (IMD deciles 1&2): 34% equivalent to Est. 40 000 0-17 year olds IAPT - 729 15-17 year olds; 4216 18-25 yr olds MAST - 500 parents parenting programmes BSF - Family support Interchange Sheffield CIC - counselling support to CYP (8-25) referred through CYTs, YJS, SHeffield Futures, VOYCe young carers, 18 secondary schools. 300 CYP pa CYTs ; YJS MIND; Samaritans Whole population: Est. 114 000 0-17 year olds Educational Psychology CAMHS core skills -211 introductory + 291 development session Schools & colleges, school nurses; police parents; clubs; VCF participation; culture, arts, leisure. Peers. 89 000 18-25 year olds CYP IAPT Epic Friends, Find Get GIve support groups e.g. young carers; sibling support for disabled children nurture groups - 108 children GPs health visitors, midwives, children centres. Family Action TAMHS 696 staff trained plus support and consultation Mental Health First Aid Sector led improvement – PSHE, anti-bullying. ESCAL. EdPsych Tier 1 There is a broad service offer at Tier 1 but support for Mental Health is not always articulated well (or quantified) within it. There is an emerging discourse around positive mental health nationally and locally e.g. 5 ways to wellbeing; resilience; everyone has mental health (Right Here); which could be co-ordinated better and built upon to reduce stigma and further develop informal support structures around mental health: families, peers etc. 33 Tier 2 Most mental health support for CYP is embedded (but not always quantified) within broader Tier 2 support services e.g. MAST and CYTs. In the case of MAST there is a clear route into Tier 3 support via Primary Mental Health workers. There is a small targeted counselling resource at Tier 2, this does not currently have formal links with CAMHS or AMHS. Although there are a range of pathways between Tier 2 and 3, (eg social workers, paediatricians and educational psychologists and via primary mental health workers based within MAST) this could be further developed to facilitate wider access by other universal and targeted services (including schools) to consultation advice and specialist services. Support for CYP stepping up and down into Tier 3 services has been identified as a gap by stakeholders. Tier 3 Capacity for service delivery at Tier 3 is much less than the expected prevalence of mental illness and disorders and there is evidence of a significant increase in demand over recent years which is reflected in increased referrals and waiting lists. There is variation in age ranges for different service delivery e.g. up to 16, up to 18, up to 25. There are changes planned around commissioning of Tier 3 services which will mean that CAMHS provision will go up to age 17 from 1 st October 2014. The Community CAMHS teams accept approximately 70% of referrals – the remaining 30% are signposted back to the referrer and into tier 2 or universal support. More investigation of the referral process and referrals would be helpful to see if there is scope to reduce the number of inappropriate referrals. CAMHS referral rates and DNAs show a correlation with deprivation – there are proportionally more referrals and more DNAs from more deprived areas. There are some areas with a high level of deprivation that seem to have a low rate of referral to CAMHS. There are wards with over 25% missed appointments (DNAs and cancellations combined) – this suggests a potential for some geographically targeted work to bridge access to CAMHS. There is under-representation of BME patients in CAMHS and AMHS. There is under-recording of ethnicity in AMHS and IAPT – this is less so in CAMHS. There is a difference in gender demographics in terms of access to CAMHS and AMHS – 63% of CAMHS patients are male compared to 51.3% of AMHS patients. 66.5% of IAPT clients are female which reflects the gender demographic of the prevalence of neurotic disorders which is the focus of IAPT provision. 34 Tier 4 Late 2013, NHS England Specialised Commissioning Oversight Group (SCOG) commissioned a review which was designed to map current CAMHS Tier 4 service provision, to consider issues that had arisen since April 2013 when commissioning arrangements transferred from local CCGs to NHS England. The main issue reported by providers was a lack of bed capacity. There was an increase in referrals into T4 CAMHS in 2013/14 compared to the previous year – it is felt this is more likely to be due to the changes in commissioning rather than in increase in need or demand in the population. The report makes a series of recommendations for development work – these are outlined in the HNA. Training and capacity building support There are a number of training and development support providers but this is not currently joined up and can result in duplication. An option would be to link at least SCC and NHSS CCG commissioned provision, for example a training and professional consultation support system which is underpinned by CAMHS but not always delivered by CAMHS Increase in need/increase in demand on services There is some evidence that there is an increase in prevalence of mental disorders and illnesses. A national longitudinal study showed increases in emotional problems and conduct problems; locally the ECM survey shows an increase in self-reported negative emotions such as sadness, anger, stress etc. National data shows an increase in seeking support for self-harm and locally there has been a marked increase in the number of children attending A&E following a deliberate self-harm (86 in 2004; 165 in 2013). There is a recent significant increase in demand for specialist CAMHs with a 30.7% increase in referrals in 2013/14 compared to 2012/13. The increase is mainly located in Community CAMHS where referrals have increased from 1461 in 2012/13 to 1975 in 2013/14 (35.2%). A similar proportion of referrals across the 2 years (approx. 70%) are being accepted – meaning that community CAMHS accepted 394 more cases in 2013/14 than 2012/13. Referrals into the Deliberate Self-Harm team have increased from 32 in 2012/13 to 62 in 2013/14. Siobhan Horsley: Sheffield City Council, Children Young People and Families Portfolio, Public Health team E: Siobhan.horsley@sheffield.gcsx.gov.uk 35 Appendix IV Sheffield Park Academy Emotional Wellbeing Pilot Summary of findings 1. Background In Autumn 2013 SCC CYPF Public health submitted a successful business case to NHSS CCG Innovations fund for £25k to pilot an Emotional Wellbeing Service in one secondary school in Sheffield. The proposed service model was a framework of commissioned activity wrapped around that school. Sheffield Park Academy was selected via a bidding process managed through the Citywide Learning Body based on levels of need, willingness to participate and ability to benefit from the package of interventions. The school was to be supported to develop its in-house response to emotional wellbeing and mental health issues and in addition have access to a range of evidence based externally provided interventions. The pilot lifespan was from November 2013 (work in school began early 2014) – July 2014. The pilot service model took into account the early findings from needs assessments and local stakeholder consultations around the provision of emotional wellbeing services: the need for consultative support for staff; step up, step down and wraparound support for CAMHS, to support earlier discharge; the need to equip staff with intervention skills rather than solely awareness raising; and the role of the school in supporting a child’s emotional wellbeing and mental health. 2. Delivery The pilot was delivered by the providers via an extension to current contracts. The service offer included whole school development work (e.g. via assemblies and PSHE), participative and therapeutic groupwork, 1:1 therapeutic counselling, and staff training and consultation. The provider organisations worked in partnership with the school, facilitated by SCC to develop an offer to meet the schools needs. 3. Learning from the pilot 3.1 Successes Open communication, flexibility and willingness to work together towards solutions by all partners The therapeutic interventions delivered by the providers and were evaluated to show success with the young people supported. Interventions have facilitated better engagement with CAMHS by one client. Students also benefitted from links and joint working with other external agencies e.g. Sexual Exploitation Service, Sheffield Young Carers 36 Providers and the school report that interventions have ‘held’ students at a lower Tier and avoided referral onto other agencies o Students wouldn’t need to go to CAMHS now perhaps. I’ve gone from seeing the counselling as a ‘holding bay – something positive and worthwhile til they see the proper people to maybe she doesn’t need to go (to CAMHS) now’. Even when still is a ‘holding bay’ it is holding from exclusion/ hospitalisation (self-harm)/risky situations (member of SPA staff) Provider staff being visible in school and being part of the school team The school have benefitted from on-site therapeutic response to 2 crisis incidents within school A simple, single point of referral pathways for receiving referrals from the school, which was part of the school’s existing structures. This maintained the unified ‘school-facing’ aspect of the service and prevented confusion or duplication of work for the school. This could have been developed further (see below) A range of provision within the one service (including access to different providers as appropriate) allows for the combination of skills, knowledge and quality of both services to be applied to the needs present within the school. Staff training & development can reinforce student interventions through raising the levels of knowledge, awareness and confidence amongst school staff which in turn increases the consistency of response toward young people with emotional wellbeing needs as well as in increasing the appropriateness of intervention in school and in referrals made for additional support Students have been well engaged with the pilot – there have been no DNAs Development of key pastoral staff developed the schools ‘in house’ response to emotional wellbeing and mental health. 3.2 Challenges A major challenge recognised by all partners was that of timescales – this then manifested itself in multiple ways throughout the project e.g. timetabling of staff training, referrals and generating a joint understanding of group work and how best to implement The knock-on effect of late delivery of staff training was that referrals were for students with much higher needs than anticipated. Training and development could have supported more appropriate referrals, and a range of referral to be able to explore the impact of a range of provision on different levels of need. The limitations on staff training delivery also meant that staff received a limited offer. Staff indicated a clear desire for more and extended training (the original proposal). Other areas of challenge included the initial process of receiving referrals from the school and the associated time-delay. 37 Difficulties in establishing group work meant that this was not possible for some referred young people who would have benefitted from this and the reluctance to allow non-referred young people to attend groups meant that the scope for certain forms of intervention were greatly reduced. 3.3 If we could do it again what would be different More development time around staff training, referral pathways Fuller staff training delivery – need to negotiate this further to meet both school needs and service needs (better planned further in advance) Staff training before referrals open for counselling Clearer offer around group work; more group work included targeted to vulnerable groups Providers to be involved at the point of referral allocation, rather than this being a separate conversation afterwards (speed up the process) Build in consultation element to the Safer Academy Partnership meetings (to support referral allocation and promote in house offer) Options for students once counselling is full up Self-referral system in place More universal work, also develop teachers to lead on universal element (link to training) e.g. follow on from assemblies, corridor workshops; involvement in PSHE; tutorial time Better promotion within school of consultation offer Transition group work with feeder school y6s Transition group work with Y11s 4 Recommendations for future service development In light of the outcomes of this pilot investment is recommended in a co-ordinated range of support and interventions, wrapped around a school (or family of schools) specifically for children and young people’s emotional wellbeing and mental health. Linking these outcomes with the recent Health Needs Assessment for Children’s Emotional Wellbeing and Mental Health, priority areas should include schools located in areas of deprivation – where circumstances contribute to a higher mental health need and lower resilience. The exact model of provision will need to be negotiated with the schools concerned but should broadly include the following: Whole staff training and development to develop the ‘in house’ universal or first line response to students emotional wellbeing and mental health: o Key members of staff to be empowered to lead on emotional wellbeing and mental health; coaching and consultative support to develop this role o Mandatory whole staff introductory level training (in order to access further training, counselling support etc to ensure appropriate referrals) 38 o Access for the whole staff team to good quality, flexible and responsive training and professional development o Support to develop in- house referral pathways into targeted provision o A focus on developing peers and teachers response Participative and therapeutic group work provision – continue to build evidence base and explore different options, models or targeting in partnership with the school. o Explore prevention work with vulnerable groups; early intervention targeted work including self-referral; transitions y6 – y7; Y11- further education and work; any other key themes identified by the school (e.g. bereavement, healthy relationships, self-harm etc) o Support school pastoral team to develop group work opportunities 1:1 therapeutic work with students o Therapeutic intervention in this context is about supporting children and young people’s response to everyday life events and building resilience. o 1:1 therapeutic work has had demonstrable positive outcomes for students emotional wellbeing, development of resilience skills and improved behaviour o It is valued by the school as evidenced by their support in implementation, and by the students evidenced by zero DNAs. A communication and monitoring system which has a range of components: o An agreed Service Level Agreements with named leads; clear links with school safeguarding and child protection policies; agreed confidentiality protocols o Regular face to face communication between school and providers o Outcomes monitoring tools which are applicable across the service and enable comparison with other services in the future o Outcomes monitoring by the school of the cohort of children and young people that receive interventions – to look at school outcomes around behaviour, attendance etc o Quarterly reporting on the above, more frequent contact during programme initiation A model which is part of a system approach o The pilot has demonstrated how school based counselling can ‘hold’ students at a lower Tier o The pilot has explored and generated evidence as to how it can relate to and add value to interventions provided by other agencies e.g. CAMHS; sexual exploitation service and Young Carers support. This 39 should be built on in future service design and a model is suggested in the diagram below. o NB A system approach to EWB & MH should also include a CYT route to accessing T2 counselling provision, for older young people or those not engaged with school – this has not been part of this pilot as further evidence for the CYT approach is already available through existing practice. 40 Appendix V MAC UK Consultation on Mapping and Understanding Accessibility of Mental Health Services for Excluded Young People in Sheffield July 2014 41 1. Background: 1.1 In early 2014, the Sheffield City Council Children, Young People and Families Portfolio (CYPF),Portfolio Leadership Team (PLT) and the Emotional Wellbeing and Mental Health Strategy group (under the auspices of the Children’s Health and Wellbeing Partnership Board) discussed and agreed to build on Sheffield’s current systems and understanding regarding the mental health of its most excluded young people. This included mapping systems and pathways from the perspective of vulnerable Children and Young People including those involved in criminality/gang violence as those experiencing more general social exclusion. This was discussed at PLT and the Strategy Group. 1.2 Sheffield Children Young People Public Health Team commissioned a consultation from Dr. Charlie Howard, Founding Director of MAC-UK and Clinical Psychologist. The commission was to interview strategic and front-line services across Sheffield to map and understand the above process to provide the group valuable additional insight into Sheffield’s mental health service provision for excluded young people. 1.3 The outcome of the interviews, conducted over 2 days, is this report which gives an overview of the findings including a clear set of key recommendations. 2. Acknowledgements: 2.1 A special thanks to Janine Dalley, Siobhan Horsley and Kalvinder Smith for all their help and coordination before and during the consultation and hosting the visit. Thank you also to everyone who took part in the interviews and engaged in such an open and constructive dialogue around children, young people and mental health. 3. Existing practice which should be commended and celebrated: 3.1 There was a genuine willingness across all interviewees to embrace mental health as a top priority for children and young people strategically and operationally. 3.2 Real commitment to good care and timely access to the right pathways for mental health care for young people. 3.3 Young people’s voice was evident in the strategic planning and service delivery with an agreed iterative manifesto in place, created by the local STAMP group. 3.4 A clear desire to build on the join up of strategic planning and service delivery in a climate of change and economic challenge. 3.5 A very good understanding of mental health and some excellent innovative ideas about ways in which strategic planning, commissioning and front-line delivery could be done differently to further build on the good practice currently in place. 3.6 A good understanding of the wider determinants of mental health e.g. housing, education. 42 3.7 Clear commitment to on-going and frequent specialist training on mental health, open to all across the city. 4. Key findings: 4.1 From analysis of all the interviews, it was found that the majority of discussion focussed strategically and operationally on 3 clear messages: i) That in these austere economic times with no additional resources, partners all recognised the need to work differently and demonstrated a clear commitment to do so; ii) It was also clear that while much good practice was evidenced on children, young people and mental health that there is a recognised gap around transitional arrangements between child and adult mental health services; and iii) The third strand of the interviews focussed on ‘referring on’ or ‘signposting’ with the majority of interviewees saying they were very receptive to the MAC-UK concept of ‘Bridging’ i.e. the majority of interviewees’ strong preference for developing a trusted relationship with a young person over time and being supported to do that work using a team around the keyworker approach. This approach would avoid the need to refer that young person on and thus the subsequent potential for them to ‘fall through the gap’ between referrals. This alternative was also seen as an opportunity to capacity build frontline staff, whilst maximising more specialist expertise. 4.2 In analysing and reflecting the above key messages, there was an overarching theme which emerged which related to ‘Longer-Term Systems Change’ which fell into two, inter-related parts: ‘longer-term change’ and more ‘immediate change’. These are discussed, below, along with key recommendations. 4.3 By way of context regarding ‘Longer-Term Systems Change’, the thinking reflected a bold aspiration to want to work together in new ways, to better meet the mental health needs of excluded young people. This was reflected at both the strategic and operational levels and suggested the need for a longer-term systems review. There was a particular aspiration to create services which focused on young people in transition between child and adult services; namely young people aged 1625 years. It was felt that this group was currently ‘falling through the gap’ of existing provision. 4.4 It was recognised that longer-term systems change was a longer-term piece of work, requiring changes to commissioning and outcomes. It would also require signup across all agencies and budgets. In most interviews, however, there was an energy and commitment to make it happen, albeit in the context of recognising that it could be a challenge. 43 4.5 It was evident that the various high-level strategic boards across children’s services not only recognised the importance of mental health but also saw it as a priority. In this context, it was felt that prioritising young people aged 16-25 years, could perhaps be embedded as a strategic priority. 4.6 More generally, it was felt that agreeing the age range of ‘young people’ for all partners would be beneficial i.e. 0-25 year olds or 0-16s. Communicating this to frontline services would then enable a clearer understanding of ‘transition’ arrangements both strategically and operationally. 4.7 Operationally, transitional arrangements were discussed throughout the interviews. There is some promising work being led by adult mental health in the form of a ‘transitions group’ but this needs to be built upon so that it can reach larger numbers and not be seen as the solution in itself. It was also recognised that mental health is just one issue effecting this age-group and that groups delivered in partnership with housing, education etc would enhance this offering. This would be a useful discussion for partners – what does this look like, entail, who owns it strategically etc. 5. Longer-Term Systems Change: 5.1 Co-located Hub Model (longer term vision) 5.1.2 Throughout the interviews, the idea of a co-located hub model emerged as a way of achieving longer-term systems change including the discussion on transition, and to meet the needs of 16-25 year olds who might not otherwise seek support for their mental health. The hub would target peer groups in general and would attract young people by co-producing activities in which they were interested e.g. music, football, job opportunities etc. Mental health trained staff would be co-located in the hub along with youth workers, employment advisors, housing advisors etc. and the mental health elements would wrap around these staff and activities. This work would take place both in the hub and around the city, recognising that not all young people are comfortable accessing support in one location. 5.1.3 By way of example, a young person might be excluded from school and known to Community Youth Teams (CYTs) as being involved in low level offending. They have been referred to Child and Adolescent Mental Health Services (CAMHS) in the past but have failed to attend. One of their friends has been doing music sessions at the hub and invites them along. They get to know the youth worker at the hub and develop a trusting relationship. One day they tell the youth worker that the only way they can feel calm is to go out looking for fights and this is why they keep getting into trouble. The mental health worker in the hub is told about this need and starts to support the youth worker to begin to explore the young person’s issues around fighting to keep calm. In so doing, the youth worker learns new skills and the young person is able to have deeper conversations with their trusted member of staff; in this case their youth worker. Sometimes the conversations are for 10 minutes at a time – it’s led by them. 44 Key recommendation: Strategic Leaders and Commissioners to consider piloting a hub way of working. There are models of good practice from elsewhere which could support the scoping, costing and operating model. 5.2 Current service provision and resources (more immediate change) 5.2.1 Whilst the hub model is an all-encompassing, longer term solution, a number of shorter-term thoughts also emerged from the interviews and would be an early step towards the wider hub ambition. These fell into three general areas in the context of existing service provision: i) Issues with young people getting ‘lost’ between referrals; ii) The need for further training of frontline staff around mental health and low level therapeutic conversations; and iii) Clinical supervision and/or tailored support of identified frontline staff. Key recommendation: These three areas could be broadly addressed by a ‘team around the keyworker’ approach, which wraps interventions and support around the key professional who works with the young person as opposed to the young person themselves. It also builds on MAC- UK’s concept of ‘bridging’ where a worker ‘bridges’ a relationship to another professional as opposed to referring on. Clearly, the detail of how this would work specifically in Sheffield needs full multi-agency discussion/time-limited working group. 5.2.2 The school nurse CYT pilot was described in the interviews. This exciting pilot involves embedding a school nurse into a CYT session(s) to enable relationship building with young people. If higher level needs emerged around mental health, then the young person would be referred on by the nurse. Key recommendation: An alternative way forward, would be for a mental health trained worker to support the nurse(s) via group clinical supervision. This could take place on a monthly basis and would capacity build the nurse(s) to do more low level mental health work. It would also nurture the relationship which has been built and prevent the young person from ‘getting lost’ between services and/or not wanting to start again with a new worker. This would reflect a ‘team around the keyworker’ model. 5.2.3 The CYTs have mental health champions, which is an excellent idea and opportunity. Key recommendation: Similar to the school nurse(s), they could attend group clinical supervision. This would maximise their potential to ‘champion’ mental health in the CYTs and to receive the necessary support. 5.2.4 There was a strong feeling that there was unmet mental health need in young people attending the CYTs but that a) young people were reluctant to access mainstream mental health services and b) they often had sub-clinical mental health needs which did not reach the criteria for these services. 6 45 Key recommendation: A solution might be to pilot embedding a mental health worker in a CYT. This would enable on-going ‘informal training’ and consultation with staff and could also allow some joint youth work and mental health work with young people in most need. 5.2.5 In terms of training, there was a strong sense that professionals across agencies would benefit from training from each other in what each other does with regards to excluded young people. Key recommendation: There could perhaps be a day where CAMHS, CYTs, Adult Mental Health (AMH), Youth Offending Service (YOS) and Police are brought together and each presents on their role and approach to excluded young people. 5.2.6 There was a strong feeling that mental health services lacked an understanding of criminal justice system in relation to gangs in Sheffield and vice versa. Key recommendation: There could, for example, be training for GPs/mental health on gangs in Sheffield and training for justice agencies on what mental health does and how they can contribute to supporting the young person. The idea of a ‘professional buddy’ system across agencies was also discussed and has been successfully piloted elsewhere. 5.2.7 There is on-going CAMHS training which was felt to be a useful resource as well as Mental Health First Aid (MHFA) training which is open to anyone on a sign-up basis. Key recommendation: The CAMHS training syllabus could expand to include training on the links between mental health and gangs/Police/YOS criminal justice and perhaps a couple of slides on this issue could be added to the MHFA training. 5.2.8 Training on attachment, anxiety, gangs as a public mental health issue was also highlighted as a useful addition to the current training programme. Key recommendation: This training could also be enhanced by covering low level mental health needs and a key message that mental health is everyone's responsibility. 5.2.9 In analysing what the interviewees meant by ‘training’, it was clear that this needed to happen on several levels. Whilst awareness training is important, it was felt that this the training also needed to focus on practical skills development. This would help the training to be embedded and to make a difference on the frontline to the service delivered to young people. Key recommendation: Training needs to be multi-agency; at a minimum level this is awareness raising but needs to be linked to a second level of training on skills and development, a third level of how to intervene and hold a 46 workload, and ongoing reflective supervision and support. This then needs to link with the real commitment to building on good pathways for young people. 47 6. Economic benefits of the above: 6.1 It was clear throughout the interviews that cuts to funding was, on one level, forcing partners to think and work differently. On another level, this was seen as an opportunity to refresh how mental health and young people was resourced strategically and operationally. There was a confidence amongst partners that the skills, knowledge and commitment was strong in the City included understanding the current levels of DNAs and just how much this was costing the system and outcomes for young people. This led on to how embracing ‘Bridging’, development of a hub and skill sharing was a sound way of addressing this significant resource cost, improving the economic cost of providing services and building on the outcomes for young people. 7. Summary: 7.1 There is a strong commitment in Sheffield to recognise and prioritise the mental health needs of excluded young people. This commitment is evident at both the operational and strategic levels. This report has given rise to some immediate recommendations which would support Sheffield’s mental health ambitions in the context of existing resources and structures. These recommendations have the potential to reduce mental health delivery costs, using high level mental health expertise in new ways. The report also points to a longer-term, systems goal, which aspires to evolve the way in which services work together. This would require a commitment from all services to use budgets in new ways and would require changes to the way in which services are commissioned more generally. There are examples elsewhere in the country where the latter has been done and Sheffield could draw on these to help it achieve its longer term ambitions. 8. Next Steps: 8.1 Dr. Charlie Howard will support Sheffield to: recommendations can be implemented/developed into an action plan; rovide support for Sheffield partners to embed the action plan; and 48 Appendix VI Right Here Sheffield’s ‘big asks’ for future service design of 16-25 year olds. Extracted from Right Here Sheffield – Supporting the Mental Health and Wellbeing ‘On the Edge’ If we are going to provide a service which successfully engages young people from many backgrounds and with different types and levels of need, we believe an Integrative approach to meeting young people’s mental health which considers the following elements is essential. The work of Right Here Sheffield has shown that we are at the edge of lots of new ways of working Sheffield needs to: • Listen and respond to young people’s experiences, views and opinions, and take these into account when making decisions that affect them. • Involve young people at a range of levels in the commissioning, development, design, delivery and evaluation of mental health services. • Combine a youth work and therapeutic approach to bring together the skills and methods of both professions. • Offer support early-on through interventions such as mental health awareness raising, resilience building activities, counselling and therapeutic group work before problems become entrenched. • Understand and recognise the importance of relationships for young people with workers and peers. Peer support is proven to reduce isolation, develop a sense of belonging and build social capital. • Offer therapeutic group work in addition to one-to-one counselling and therapeutic support, as this is a form of intervention which many young people benefit from and tell us they highly value. • Offer flexibility and choice through a wide range of interventions drawing on different approaches such as mindfulness, CBT and positive psychology to tailor what is delivered to the individual needs of young people. • Reach out to young people at the places they already go to, or are comfortable in attending, to provide ‘non-stigmatising’ support, which those, who are unlikely to engage with more traditional mental health services may be more likely to access. The work of Right Here Sheffield has shown that we are at the edge of lots of new ways of working with young people, supporting them to improve their own mental health and the mental health of those around them. We need a mental health and wellbeing service for 16-25 year olds that offers young people hope for their future and the help they need to grow and change at a critical period of their life and development. We feel that the work of Right Here Sheffield has laid some of the groundwork for this transformation. We believe the 49 recommendations and messages in this report offer some of the solutions to achieving this transformation in mental health service design and delivery for Sheffield’s young people. http://interchangesheffield.org.uk/right-here 50 Appendix VII 51 TUPE information: TUPE Emotional Wellbeing List 1 of 2.docx TUPE Emotional Wellbeing List 2 of 2.docx 52 METHOD STATEMENT Please answer each question, referring to the specification. Please ensure you refer to the allocated word count and keep within this. Boxes can be enlarged accordingly. LOT 3: Universal and Targeted Emotional Health & Wellbeing Service For each statement (excluding 3.3), please demonstrate how this will be measured. This will form part of the contract if awarded Weight 10% 1. Identification Word How will your organisation identify and engage children and Count young people at risk of or experiencing poor emotional health and wellbeing? 800 Please refer to Supporting documents. 53 2. 2. Define Your Service Model 15% 2.1 Describe and illustrate your service model taking into account the continuum of need identified in the specification. Include the range of interventions offered, prioritisation, stepup/step-down, where the service will be located and the workforce required to deliver this. Also demonstrate a needsled approach to service access and hours of operation, and ability to scale- up if required. 1200 54 10% 2.2 Describe how your service will work with schools to develop their ‘in-house’ support for children and young people’s emotional wellbeing and mental health. 800 55 10% 2.3 How will your service interact with the health, social care and education systems to maximise outcomes for these children and young people? Include referral pathways, ‘bridging’ and capacity building. 800 56 10% 3 Added Value 3.1 Describe the added value your organisation will bring to the Emotional Health and Wellbeing Service. 800 57 15% 3.2 Give examples of innovative ways your organisation will deliver key elements of the specification (please refer to the Outcomes section of the Specification and the Consultation reports). 1200 58 10% 3.3 Please provide a mobilisation plan which ensures that the service is ready to commence 1st April 2015. 800 Include reference to continuity of care for service users, staff/TUPE, stakeholder management, premises and IT. 20% 4 Presentation The top 3 scoring bids following evaluation of responses to the above 3 questions will be invited to deliver a presentation to the Young Commissioners on 22nd December 2014. This will cover young carers’ influence and participation in service delivery. Details will be circulated to shortlisted organisations nearer the date. Please note that those organisations not invited to deliver presentations will be given a quality score out of 80%. Those invited to presentation stage will be given the opportunity to score a further 20%. 59 PRICING SCHEDULE – 10% Weighting Please state how the service would be provided within the budget (Budget £140k per annum. 1 year contract plus 1 year plus 1 year option to extend - this is pending funding availability Contract Total £140k) by demonstrating a breakdown of costs. The TUPE information provided will assist with this. See Section 4.1.4 of the main ITT document for Scoring information. Description Cost Total 60