Humana health insurer rules on preauthorization for genetic testing
advertisement

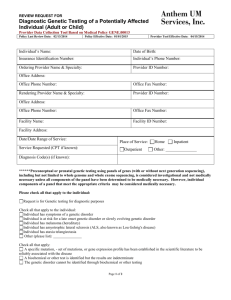
Humana health insurer rules on preauthorization for genetic testing Humana website 12.18.15 Molecular Diagnostic and Genetic Testing (MD/GT) Preauthorization of MD/GT is required for commercial, Medicaid and Medicare Advantage (MA) health maintenance organization (HMO) and preferred provider organization (PPO) members. In Puerto Rico, preauthorization is required for all MI Salud (i.e., Medicaid) and commercial products. Preauthorization is not required for: MA private fee-for-service (PFFS) plans Risk groups CarePlus members HumanaOne members MA members in HMO groups in Florida, Illinois, Nevada, Arizona and California Humana's Genetic Guidance Program The Genetic Guidance Program is a utilization management initiative designed to share information with physicians and members about the use and appropriateness of MD/GT. Board-certified genetic counselors are available to discuss genetic testing services, and preauthorizations. To initiate a request, you may call 1-800-523-0023. Representatives are available from 8 a.m. to 8 p.m. Eastern time, Monday through Friday. Submitting Preauthorization Requests Physicians and local labs (Puerto Rico only) have several options when submitting their preauthorization requests: Submit requests online Physicians may log into Humana's secure provider portal at Humana.com/providers to initiate a preauthorization request. Providers who are registered with Availity, may initiate preauthorization requests through Availity and the requests will be directed to our genetic counselors. Submit requests by phone Physicians may initiate preauthorization request by calling Humana's Interactive Voice Response system (IVR) at 1-800-523-0023. If needed, representatives are available from 8 a.m. to 8 p.m. Eastern time, Monday through Friday. A board-certified genetic counselor may ask the physician questions about the patient's condition and past medical/family history. Genetic counselors can also answer questions related to the test(s) the physician is ordering and applicable Humana clinical policies. Requestor will receive notification of the outcome of the request. Submit requests by fax Physicians/local labs may also request preauthorization via fax. To do so, download the preauthorization request form below, fill it out in its entirety and fax it to us at 1-855-227-0677. A board-certified genetic counselor will review the request and contact the physician/local lab if additional information is required. Approvals of requests are returned via phone or fax; nonapprovals are sent via mail. United States Request Form (265 KB) Download PDFEnglish Puerto Rico Request Form (556 KB) Download PDFEnglish Texas authorization request form Physicians and other clinicians in Texas may use this form to submit authorization requests for their Humana-covered patients. Instructions are available here. Once complete, please fax it to Humana at 1-800-266-3022. Include supporting clinical documentation (e.g., medical records, progress notes, lab reports, radiology studies, etc.) with your fax form. Indiana authorization request form Physicians and other clinicians in Indiana may use this form to submit authorization requests for their Humana-covered patients. Instructions are included on the form. Once complete, please fax it to Humana at 1-800-266-3022. Include supporting clinical documentation (e.g., medical records, progress notes, lab reports, radiology studies, etc.) with your fax form. Information Needed When Requesting Preauthorization The physician should have relevant clinical information available in the patient's chart when requesting preauthorization, including: Member name and Humana member ID number Ordering physician name and provider ID or tax ID number Telephone and fax numbers of the ordering physician Name, telephone number and fax number of lab/facility performing the test Patient diagnosis or clinical indication (ICD code) Test being ordered (CPT code or test name) Indication/reason for test Signs, symptoms and duration Prior related diagnostic and/or genetic tests and their results Laboratory studies and results Family medical/genetic history Medications and duration (if related) Prior treatments or other clinical findings (when relevant) How the test results will be utilized in the member's care Local laboratory name, provider ID or tax ID (i.e., Puerto Rico lab or facility that will collect the sample— Puerto Rico only) Exclusions to Preauthorization While most genetic tests and molecular diagnostics require prior authorization, the following categories are excluded: Routine prenatal screening — Non-invasive prenatal testing does require preauthorization Routine inpatient newborn screenings Human leukocyte antigen (HLA) testing for transplant Chromosomal analysis for leukemia and lymphoma Infectious disease testing considered to be the standard of care For all other tests, the health care provider should contact Humana to request preauthorization. Additional Resources