INTRODUCTION: - British Renal Society
advertisement
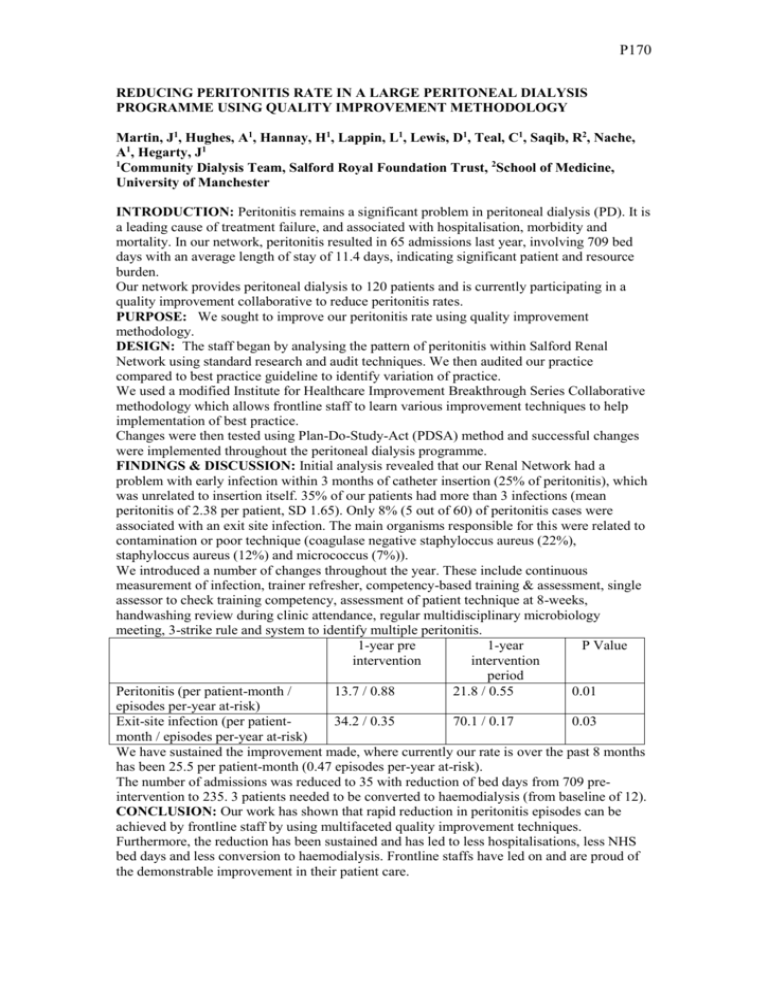
P170 REDUCING PERITONITIS RATE IN A LARGE PERITONEAL DIALYSIS PROGRAMME USING QUALITY IMPROVEMENT METHODOLOGY Martin, J1, Hughes, A1, Hannay, H1, Lappin, L1, Lewis, D1, Teal, C1, Saqib, R2, Nache, A1, Hegarty, J1 1 Community Dialysis Team, Salford Royal Foundation Trust, 2School of Medicine, University of Manchester INTRODUCTION: Peritonitis remains a significant problem in peritoneal dialysis (PD). It is a leading cause of treatment failure, and associated with hospitalisation, morbidity and mortality. In our network, peritonitis resulted in 65 admissions last year, involving 709 bed days with an average length of stay of 11.4 days, indicating significant patient and resource burden. Our network provides peritoneal dialysis to 120 patients and is currently participating in a quality improvement collaborative to reduce peritonitis rates. PURPOSE: We sought to improve our peritonitis rate using quality improvement methodology. DESIGN: The staff began by analysing the pattern of peritonitis within Salford Renal Network using standard research and audit techniques. We then audited our practice compared to best practice guideline to identify variation of practice. We used a modified Institute for Healthcare Improvement Breakthrough Series Collaborative methodology which allows frontline staff to learn various improvement techniques to help implementation of best practice. Changes were then tested using Plan-Do-Study-Act (PDSA) method and successful changes were implemented throughout the peritoneal dialysis programme. FINDINGS & DISCUSSION: Initial analysis revealed that our Renal Network had a problem with early infection within 3 months of catheter insertion (25% of peritonitis), which was unrelated to insertion itself. 35% of our patients had more than 3 infections (mean peritonitis of 2.38 per patient, SD 1.65). Only 8% (5 out of 60) of peritonitis cases were associated with an exit site infection. The main organisms responsible for this were related to contamination or poor technique (coagulase negative staphyloccus aureus (22%), staphyloccus aureus (12%) and micrococcus (7%)). We introduced a number of changes throughout the year. These include continuous measurement of infection, trainer refresher, competency-based training & assessment, single assessor to check training competency, assessment of patient technique at 8-weeks, handwashing review during clinic attendance, regular multidisciplinary microbiology meeting, 3-strike rule and system to identify multiple peritonitis. 1-year pre 1-year P Value intervention intervention period Peritonitis (per patient-month / 13.7 / 0.88 21.8 / 0.55 0.01 episodes per-year at-risk) Exit-site infection (per patient34.2 / 0.35 70.1 / 0.17 0.03 month / episodes per-year at-risk) We have sustained the improvement made, where currently our rate is over the past 8 months has been 25.5 per patient-month (0.47 episodes per-year at-risk). The number of admissions was reduced to 35 with reduction of bed days from 709 preintervention to 235. 3 patients needed to be converted to haemodialysis (from baseline of 12). CONCLUSION: Our work has shown that rapid reduction in peritonitis episodes can be achieved by frontline staff by using multifaceted quality improvement techniques. Furthermore, the reduction has been sustained and has led to less hospitalisations, less NHS bed days and less conversion to haemodialysis. Frontline staffs have led on and are proud of the demonstrable improvement in their patient care.