General Anesthesia
advertisement
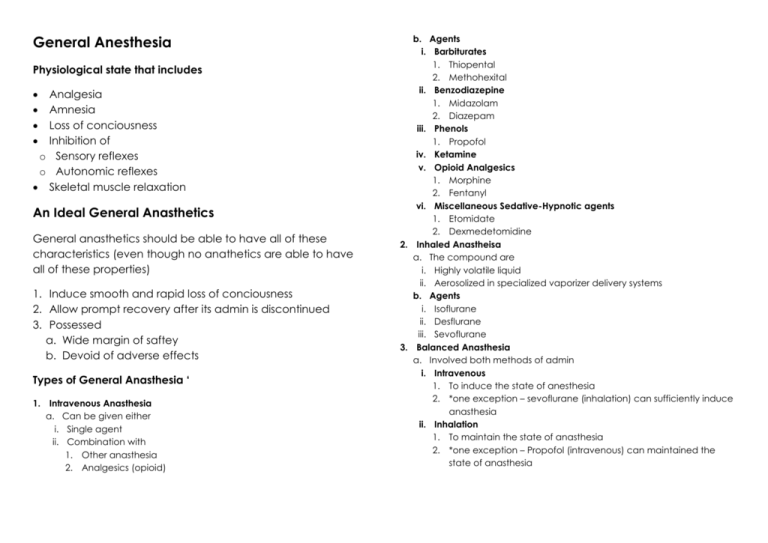
General Anesthesia Physiological state that includes Analgesia Amnesia Loss of conciousness Inhibition of o Sensory reflexes o Autonomic reflexes Skeletal muscle relaxation An Ideal General Anasthetics General anasthetics should be able to have all of these characteristics (even though no anathetics are able to have all of these properties) 1. Induce smooth and rapid loss of conciousness 2. Allow prompt recovery after its admin is discontinued 3. Possessed a. Wide margin of saftey b. Devoid of adverse effects Types of General Anasthesia ‘ 1. Intravenous Anasthesia a. Can be given either i. Single agent ii. Combination with 1. Other anasthesia 2. Analgesics (opioid) b. Agents i. Barbiturates 1. Thiopental 2. Methohexital ii. Benzodiazepine 1. Midazolam 2. Diazepam iii. Phenols 1. Propofol iv. Ketamine v. Opioid Analgesics 1. Morphine 2. Fentanyl vi. Miscellaneous Sedative-Hypnotic agents 1. Etomidate 2. Dexmedetomidine 2. Inhaled Anastheisa a. The compound are i. Highly volatile liquid ii. Aerosolized in specialized vaporizer delivery systems b. Agents i. Isoflurane ii. Desflurane iii. Sevoflurane 3. Balanced Anasthesia a. Involved both methods of admin i. Intravenous 1. To induce the state of anesthesia 2. *one exception – sevoflurane (inhalation) can sufficiently induce anasthesia ii. Inhalation 1. To maintain the state of anasthesia 2. *one exception – Propofol (intravenous) can maintained the state of anasthesia Stages of Anasthesia – Guedel signs Inhaled Anasthetics 1. Stage of Analgesia a. At first, patient at the state of analgesia without amnesia b. Later, amnesia comes about 2. Stage of Excitement a. Patients appear to be i. Vocalized delirium ii. Amnesia iii. Irregular respiration iv. Retching v. Vomiting b. This state can be avoided by giving high concentration of anasthesia c. The stage ends when respiration is normalized 3. Stage of Surgical Anasthesia a. Begins with recurrence of regular respiration b. Extends to a complete halt in respiration (apnea) c. Signs appear as changes in i. Ocular movement ii. Eye reflexes iii. Pupil size 4. Stage of Medullary Depression a. Deep stage of CNS depression b. Includes i. Vasomotor center ii. Respiratory center in the medulla c. Without respiratory support, death ensures within minutes Pharmacokinetics 1. Uptake and Distribution of Inhaled Anasthetics a. Concentration of an inhaled anasthetic is proportional to its partial pressure b. Adequate brain concentration is important in order to determine the depth of general anasthetics c. The rate of adequate concentration to be achieved in the brain depends on i. Solubility 1. Blood:gas partition coefficient is a useful index in determining the solubility of the inhaled anasthetics 2. Blood:gas partition coefficient a. Poorly blood soluble anasthetics i. Requires less amount of molecules to reach the arterial partial pressure ii. The levels rises rapidly in the blood iii. Onset of action in the brain is rapid iv. Eg. Nitric Oxide b. Highly blood soluble anasthetics i. Requires more amount of molecules to reach the arterial partial pressure ii. The level in the blood rises very slow iii. Slow onset of action in the brain iv. Eg. Halothane ii. Anasthetic Concentration in the Inhaled Air 1. ↑the conetration of anasthesia inhaled, ↑ the rate of transfer into the blood 2. Example a. Moderate blood soluble anasthesia i. Given in high doses in the induction phase to reach a rapid increase in blood level ii. Doss is reduced once the therapeutic level in the brain is achieved iii. It often be given with less soluble anasthesia (Nitric oxide) to ↓time required for 1. Loss of conciousness 2. Achievement the state to surgical anasthesia iii. Pulmonary Ventilation 1. ↑in rate and depth of ventilation, ↑arterial tension (level in the blood) of inhaled anasthetics 2. Variability a. ↑in rate and depth of ventialtion have variable effects depending on the solubillity of inhaled anasthetics i. Poorly soluble anasthetics (Nitric oxide) only has insignificant increase in arterial gas tension ii. Highly and moderately soluble anasthetics (Halothane) has a very significant increase in arterial gas tension up to fourfolds iv. Pulmonary Blood Flow 1. ↑in cardiac output will lead to a. ↑pulmonary perfusion b. Exposes larger volume of blood c. ↑blood carrying capacity d. ↓rate of rise in the anasthetic tension in the blood 2. ↓in cardiac output a. ↓pulmonary perfusion b. Exposes fewer volume of blood c. ↓blood carrying capacity d. ↑rate of rise in the anasthetic tension in the blood v. Arteriovenous Concentration Gradient 1. Distribution of inhaled anasthetics to the peripheral tissues depends on a. Solubility of the agent i. Lipid soluble more likely to accumulate in tissue b. Concentration gradient of drugs between blood and tissues i. ↑concentration gradient, ↑accumulation in peripheral tissues c. Tissue blood flow i. Highly perfused organs tend to accumulate the drugs 1. Brain 2. Heart 3. Liver 4. Kidneys 5. Splanchnic bed d. If the distribution of drugs in the peripheral tissues are high, less venous concentration of drugs i. Due to this, rate of achieving the arterial blood tension is slower due to less drugs remain in the blood to achieve the therapeutic effects 2. Elimination a. Recovery phase depends on the rate of elimination of anasthetics from the brain b. Two distinctive features of the recovery phase compared to that of induction phase i. Transfer of drugs from the blood back to the lung cannot be increased as drugs in the lungs cannot be reduced to zero level 1. While induction phase, transfer of drugs from the lung to the blood can be increased by ↑rate and depth of ventilation ii. Anasthetics gas tension in different tissues are variable in the recovery phase 1. While during induction phase, all tissues anasthetics gas tension remains at zero level c. Factors governing the rate of elimination are i. Blood:gas partition coefficient of anasthetics 1. ↑blood solubility, ↓rate of elimination ii. Duration of exposure 1. ↑duration of exposure, ↓rate of elimination as drugs have already accumulated in various tissues iii. Pulmonary clearence is the principal route of elimination. Somehow, liver also plays important role I elimination 1. Halothane is metabolized in toxic metabolite called the Chlorotriflouroethyl free radical a. May lead to Halothane-induced Hepatitis 2. The rank in susceptibility to hepatic metabolism a. Methoxyflurane Halothane Enflurane Sevoflurane Isoflurane Desflurane Nitric Oxide Systemic Effects of Inhaled Anasthetics 1. Cardiovascular Effects a. Blood pressure i. ↓BP proportionate to dose 1. Due to ↑ individual vascular beds (cerebral artery) with little change in systemic vascular resistance that leads to ↓cardiac output a. Halothane b. Enflurane 2. Due to ↑TPR with slightly ↓in cardiac output a. Isoflurane b. Desflurane c. Sevoflurane b. Heart rate i. Bradycardia 1. Due to direct vagal stimulation a. Halothane ii. Tachycardia 1. Due to transient stimulation of sympathetic outflow a. Desflurane c. ↓myocardial oxygen consumption 2. Respiratory Effects a. ↑ventilation rate b. ↓tidal volume c. ↑arterial PCO2 level d. ↓mucocilliary function 3. Brain Effects a. ↓metabolic activity of the brain b. ↑intracranial pressure secondary to ↑cerebral blood flow i. Nitirc oxide it the least likely to cause this c. CNS depression i. At higher dose ii. Myoclonic activity iii. Seizure like activity may also appear 4. Kidneys Effects a. Solely depends on the dose given b. ↓glomerular filtration rate c. ↓renal blood flow d. ↑filtration fraction Toxicity 1. Acute Toxicity a. Halothane-Induced Hepatitis i. Halothane b. Nephrotoxicity i. Formations of floride metabolites in 1. Methoxyflurane 2. Enflurane 3. Sevoflurane c. Malignant Hyperthermia i. If given together with muscle relaxant (Succinylcholine) ii. Treated with Dentrolene 2. Chronic Toxicity a. Mutagenicity b. Carcinogenicity c. Problems with reproductive system d. Heamatotoxicity i. Megaloblastic anemia Mechanism of Actions of General Anasthetics 1. Lipid Solubility-Anaesthetic Potency Correlation (the MeyerOverton correlation) a. May act by dissolving in the fatty fraction of brain cells and removing fatty constituents from them, i. Thus changing activity of brain cells and inducing anaesthesia b. The greater is the lipid solubility of the compound, the greater is its anaesthetic potency 2. Lipid Hypotheses of General Anaesthetic Action a. Hydrophobic anaesthetic molecules accumulate inside the hydrophobic (or lipophilic) regions of neuronal lipid membrane causing its distortion and expansion (thickening) due to volume displacement b. Accumulation of critical amounts of anaesthetic causes membrane thickening sufficient to reversibly alter function of membrane ion channels thus providing anaesthetic effect c. This hypotheses is now rejected 3. Modern Lipid Hypotheses a. Anaesthetic effect happens if solubilization of general anaesthetic in the bilayer causes redistribution of membrane lateral pressures b. According to modern lipid hypothesis change in membrane lateral pressure profile shifts the conformational equilibrium of certain membrane proteins known to be affected by clinical concentrations of anaesthetics such as ligand-gated ion channels 4. Membrane Protein Hypothesis of General Anaesthetic action a. According to this theory general anaesthetics are much more selective than in the frame of lipid hypothesis and they bind directly only to small number of targets in CNS mostly i. ligand(neurotransmitter)-gated ion channels in synapse ii. G-protein coupled receptors altering their ion flux b. Particularly Cys-loop receptors are plausible targets for general anaesthetics that bind at the interface between the subunits. c. The Cys-loop receptor superfamily includes i. Inhibitory receptors 1. GABAA receptors 2. GABAC receptors 3. Glycine receptors and ii. Excitatory receptors 1. Acetylcholine receptors 2. 5-HT3 serotonin receptors d. General anaesthetics can e. Inhibit the channel functions of excitatory receptors f. Potentiate functions of inhibitory receptors Intravenous General Anasthetics Differences of IV anasthetics compared to Inhalation Doesn’t need specialized vaporiser machine Rapid onset of action o Use during induction phase o Benzodiazepine is exception cause it has slow onset of action Rapid recovery o Enables use in short ambulatory surgical procedure Agents Barbiturates Thiopental Contraindication Severe hypotension Addison disease Liver disease Breathing disorder Pharmacokinetics Upon admin, rapidly crosses the BBB With sufficient dose, loss of conciousness ensures in a single cardiac cycle sufficient Highly lipid soluble o Plasma:brain equilibrium reaches very rapidly o High Vd, redistributed to almost all body compartment o Due to rapid redistribution (clearence from brain), duration of action is short Metabolized in the liver Excreted through urine Lacks of Antinoceptive activity Adjuvant Therapy Opioid o Combined with Fentanyl Morphine Sufentanyl o ↑cardiac stability o ↑respiratory depressive effects o ↑postoperative emesis Pharmacological Effects 1. CVS effects (dose dependent) o ↓BP o ↓Cardiac output o ↓stroke volume o ↑venous capacity (venodilation) 2. Respiratory effects o Potent respiratory depressor o Produces Transient apnea ↓sensitivity of respiratory center to changes in PCO2 3. CNS effects o ↓in cerebral Metabolism Oxygen consumption o ↓cerebral blow flow Can be given in pts with ↑ICP 4. Hepatic and Renal Effects o ↓hepatic and renal blood flow Adverse Effects 1. 2. 3. 4. 5. 6. Hypotension Apnea Airway obstruction Emergence delirium Prolonged somnolence Nausea Agents Benzodiazepines Pharmacokinetics 1. Diazepam 2. Lorazepam 3. Midazolam Clinical Uses Preanasthetic medications Adjuvant during surgical procedures performed under local anasthesia Contraindication Pregnancy Myasthenia gravis COPD Solubility o Non-water soluble Agents Diazepam Lorazepam Formulate in non-aquous vehicles which can lead to local irritation o Water soluble Agent Midazolam Prepared in aquous solution; the drug of choice to be given parenterally All drugs can become lipid soluble in the physiological pH Readily crosses the BBB The slowest onset among other IV general anasthetics o Reaches plateau CNS effects too early that it is inadequate for surgical anasthesia o Further ↑in dose will lead to Prolong postanasthetic recovery period High incidence of anterograde amnesia Midazolam has the most rapid onset among other Benzodiazepine Pharmacological Effects 1. CNS effects a. Sedative b. Anxiolytic c. Amnestic properties d. Ability to control acute agitation 2. Respiratory effects a. Respiratory depression Adverse Effects 1. Pradoxical Effects a. Aggression b. Violence, c. Impulsivity d. Irritability e. Suicidal behavior sometimes occur 2. Cognitive Effects a. Anterograde amnesia 3. May develop a. Tolerence b. Depedency c. Withdrawal syndrome Agents Propofol Pharmacokinetics Clinical Uses Induction phase of anasthesia Maintainance phase of anasthesia Can be either o Total IV procedure o Balanced procedure The most suitable for ambulatory surgical procedures Rapid onset Rapid recovery rate If given through prolong infusion o Cumulative effects may produce including Delayed recovery phase ↑serum lipid level (since propofol often formulated in lipid vehicles) Severe acidosis in children Respiratory infections may also presented Upon admin, half life is about 2-8 minutes o But after redistribution to peripheral tissues, half life elevated to 30-60 minutes Metabolize through Glucuronidation phase in the liver and other extrahepatic metabolic system o May be useful for pts with hepatic insufficiency Excreted via urine Pharmacological Effects CNS effects o Reduction in the postoperative Nausea Vomiting o Improve sense of wellbeing o Effective in producing prolonged sedation Respiratory Effects o Produces Transient apnea ↓sensitivity of respiratory center to changes in PCO2 CVS effects o Marked ↓in BP due to ↓TPR o Venodilation o Negative inotropic effects Adverse Effects 1. 2. 3. 4. 5. 6. Pain at the site of injection Hypotonus Tremor (rare) Hypotension Apnea Airway obstruction Agents Etomidate Clinical Use Induction phase of anasthesia Pharmacokinetics Ketamine Clinical Uses Due to its cardiostimulatory effects, useful in o Cardiogenic shock o Septic shock Given with propofol in ambulatory surgery Contraindication ↑ICP Rapid loss of conciousness o With minimal hypotension Rapid biphasic distribution to the peripheral tissues o Initial distribution Half life – 3 minutes o Intermediate distribution Half life – 29 minutes Rapid redistribution to peripheral tissues leads to rapid short duration of action Extensive hepatic metabolism Excreted via urine Highly lipophilic, distributed extensively in highlyperfused organs o Brain o Liver o Kidneys Fast induction phase Slow recovery Redistribution to other peripheral tissues happens after prolonged use Metabolized in the liver Excreted through o Bile o Urine Pharmacological Effects Adverse Effects Minimal CVS and Respiratory depression o Doesn’t change the heart rate o Apnea is very seldom No analgesic property 1. Prolonged infusion will lead to a. Hypotension b. Electrolyte imbalance c. Oliguria CNS effects o Dissociative Anasthetic State Catatonia Behavioral abnormalities Stupor Amnesia Analgesia With/out loss of conciousness o ↑cerebal blood flow CVS effects o ↑in sympathetic outflow leads to ↑TPR ↑heart rate ↑cardiac output ↑BP o This is due to Stimulation of central sympathetic nervous system Inhibition of reuptake of norepinephrine in the presynaptic terminal Respiratory Effects o Minimal respiratory depression 1. Postoperative psychic phenomena a. Disorientation b. Sensory and perceptual illusions c. Vivid dream d. Delirium e. Hallucination 2. Hypertension 3. ↑salivation