Negative Impacts of Blood Transfusions: Are they preventable?

Negative Impacts of Blood
Transfusions: Are they preventable?
Felice Felser, MSN, APRN-BC
In the wake of healthcare reform, hospitals find themselves amidst a culture of conservation.
That culture has seemingly taken root with some physicians and administrators. However, are healthcare professionals still missing the boat when it comes to blood management and its conservation during surgical procedures?
Are they doing everything possible to obtain proper and accurate data to prevent the soaring costs of blood transfusions from rising to astronomical proportion?
The Society for the Advancement of Blood
Management (SABM) and the Medical Society for Blood Management (MSBM) are two organizations dedicated to improving patient outcomes through the appropriate use of blood and blood products, and by developing strategies to reduce or avoid blood transfusions. Even with these medical groups in place, the annual cost of a blood transfusion is rising. A recent study published in the April
2010 issue of Transfusion, a peer review academic journal, states, “When all of the complex cost factors leading up to and after a red blood cell transfusion are considered, the actual cost of blood is substantially higher than previously estimated”. (1) The study calculated the annual expenditure of blood transfusions and related activities for surgical patients to be between $1.6 and $6.0 million per hospital surveyed. (2)
Clinical Implications
Besides the cost of transfusion, significant mortality rates and comorbidities are directly associated with the number of units transfused.
A research paper by Koch, etal., published in
1
Critical Care Medicine journal, describes an overall in-hospital mortality rate of 3.07% for those patients transfused with packed red blood cells (PRBC’s) as compared to 0.05% for those who did not receive transfusion. (3)
Additionally, Koch found there to be a “dosedependent relationship between each unit transfused” and mortality rates years later. (Fig
1)
Figure 1: Koch C. G. et al.; Ann Thorac Surg
2006;81:1650-1657
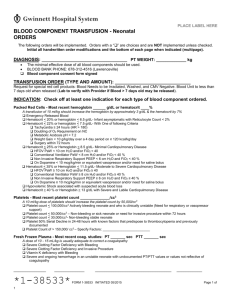
Further, PRBC transfusion is the single factor most reliably associated with increased risk of bypass related post-surgical outcomes (4). Post operative morbid events for those patients transfused compared to those who did not receive PRBC’s are best depicted in Figure 2.
Figure 2: Koch CG, et al. Crit Care Med
2006;34(6):1611
The decision to transfuse is generally based on numerous factors, ie: anemia, hemorrhage,
religious beliefs etc. However, the study concludes that women are more often transfused than men for no apparent reason despite having similar preoperative hemoglobin values and co-morbid conditions, whereas other health professionals have reported no clear indication at all for transfusion (4). So the question should be asked: Are we doing everything possible as healthcare providers to ensure quality patient care while keeping unnecessary procedures and costs low?
Point of Care: Measured Hematocrit or
Measured Hemoglobin in the CVOR?
The use of point-of-care instruments has greatly increased over the past decade. Specifically, point of care blood gas analyzers have been significantly used in cardiac surgery due to their rapid turnaround time, menu of measured analytes, and availability. Clinicians rely on the analyzer’s values to make timely decisions regarding patient care, namely the hemoglobin and hematocrit.
Currently there are two distinct methods of determining the need for transfusion, a measured hematocrit or measured total hemoglobin. A measured hematocrit is obtained through conductivity. Conductivity is the ability of a solution to transmit an electrical current. Conductivity-based hematocrit is accurate for most clinical situations. ”However, the accuracy of hematocrit using conductivity is affected by changes in sodium levels, changes in protein concentrations, the use of plasma expanders, and the amount and types of anticoagulants used during surgery”. (5)
Therefore, the ability to transmit current and receive an accurate hematocrit will be affected by the protein concentration within the plasma.
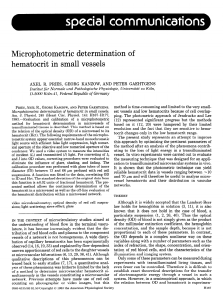
The alternative method, obtaining measured total hemoglobin, is driven by spectrophotometry and optical reflectance.
“Specific wavelengths and photodiodes are used to produce electric currents proportional to the light intensities”. (5) This will give
2 measured total hemoglobin without affects from hemodilution, protein concentrations, and anticoagulants used in cardiac bypass surgery.
Multiple studies have shown that using conductivity measurements during bypass surgery will give an erroneously low hematocrit thereby causing unnecessary transfusions. For example, a study conducted by Steinfelder-
Visscher concluded that of the 55 patients tested, 87% received erroneously low hematocrits and would have been unnecessarily transfused. (5)
Conclusion
With this knowledge in mind, why do medical professionals continue to disregard the data and use point of care equipment that utilizes conductive measurements? It seems to be a simple solution to a growing problem of unnecessary procedures driving healthcare costs higher. The studies have shown a superior method to conductivity. Clinicians who continue to use measured hematocrits are placing patients at increased risk for posttransfusion comorbidities and are linearly decreasing their lifespan per unit of PRBC transfused. I believe it is time to use the point of care alternatives on the market which provide measured total hemoglobin that is accurate.
References:
(1) Shander, A. ., Hoffman, A. Ozawa, S., theusinger, O., Gombotz, H., Spahn, D.
“Activity- based costs of blood transfusions in surgical patients at four hospitals”. Transfusion. April 2010,
Volume 50, Issue 4, Pages 753-765.
(2) “New published study finds the cost of blood transfusions is significantly under-estimated, establishes true cost at $522 to $1183 per unit”. PR
Newswire, retrieved July 2010 www.prnewswire.com.
3
(3) Koch CG, Li L, Duncan AI, Mihaljevic T,
Loop FD, Starr NJ, Blackstone EH.
“Transfusion in coronary artery bypass grafting is associated with reduced long-term survival”. Annals of Thoracic
Surgery. 2006;81:1650-1657.
(4) Koch CG, Li L, Duncan AI, et al.
“Morbidity and mortality risk associated with red blood cell and bloodcomponent transfusion in isolated coronary artery bypass grafting”.
Critical Care Med 2006;34:1608-1616.
(5) Myers, G., Browne, J. “Point of care hematocrit and hemoglobin in cardiac surgery: a review.” Perfusion 2007; 22:
179-183.