Acute Respiratory Distress Syndrome (ARDS)
advertisement
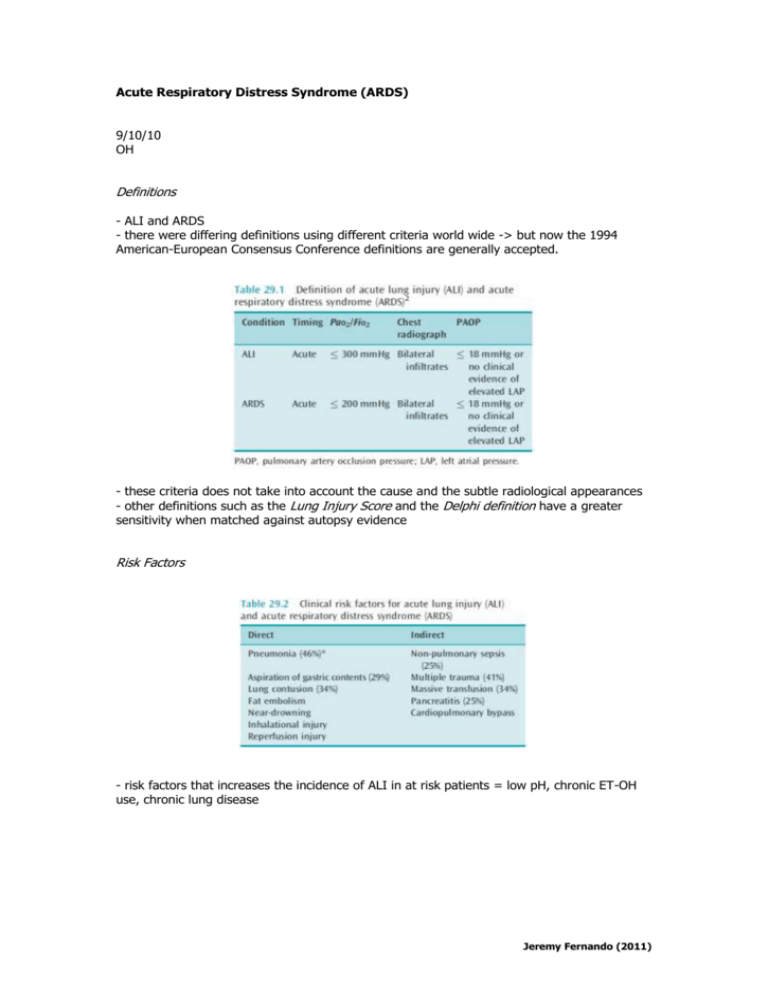
Acute Respiratory Distress Syndrome (ARDS) 9/10/10 OH Definitions - ALI and ARDS - there were differing definitions using different criteria world wide -> but now the 1994 American-European Consensus Conference definitions are generally accepted. - these criteria does not take into account the cause and the subtle radiological appearances - other definitions such as the Lung Injury Score and the Delphi definition have a greater sensitivity when matched against autopsy evidence Risk Factors - risk factors that increases the incidence of ALI in at risk patients = low pH, chronic ET-OH use, chronic lung disease Jeremy Fernando (2011) Pathogenesis PHASES = injury -> exudative -> proliferative -> fibrosing -> resolution - complex: (1) pulmonary oedema from damage to the alveolocapillary barrier (2) inflammatory infiltrates (3) surfactant dysfunction THE ALVEOLOCAPILLARY BARRIER - damage with bidirectional flow (proteins and fluid in to alveoli, surfactant and alveolar cytokines into plasma) - surfactant dysfunction - proliferation of type II cells -> the balance between repair and fibrosing alveolitis INFLAMMATORY INFILTRATES - migration of neutrophils into alveoli with activation -> release of oxygen species, cytokines, eicasanoids, proteases -> tissue damage - pulmonary endothelial cells, platelets, interstitial and alveolar macrophages also play important roles in alveolar inflammation. SURFACTANT DYSFUNCTION - decreased activity -> decrease in pulmonary compliance - caused by increased binding by plasma proteins and decreased production RESULTS - hypoxaemia (V/Q mismatch, impaired hypoxic pulmonary vasoconstriction) increase in dependent densities (surfactant dysfunction, alveolar instabilities) decreased compliance (surfactant dysfunction, decreased lung volume, fibrosis) collapse/consolidation (increased compression of dependent lung) increased minute ventilation (increased in alveolar dead space) increased WOB (increased elastance, increased minute volume requirement) pulmonary hypertension (vasoconstriction, microvascular thrombi, fibrosis, PEEP) Clinical Management GENERAL - diagnosis and appropriate treatment to minimise physiological impact of cause (drain collection, antibiotics, resuscitate, splint fractures) - feed - standard ICU prophylaxis MECHANICAL VENTILATION Jeremy Fernando (2011) - ARDS Network Study - controlled ventilation - TV 6mL/kg - avoid overstretch (volutrauma) and inadequate recruitment (atelectrauma) - Plateau pressure of <30cmH2O - PEEP titration is difficult and there many techniques that are acceptable: (1) titrating to the PF ratio – as in the ARDS protocol, (2) titration to PaO2 and aiming for a PEEP of 15, (3) measuring elastic mechanics at the bedside (PEEP was initially titrated to the lower inflection point of the PV loop -> this is now known to lead to overstretching and hyperinflation) - recruitment manoeuvres (PEEP 30-40cmH2O held for 30 seconds) -> can improve oxygenation but controversial - mode of ventilation: generally no difference (PCV tends to be used c/o plateau pressure approximates peak pressure, with VC plateau pressure needs to be measured), no role for inverse ratio ventilation (I:E ratio > 1) -> increased mean airway pressure + haemodynamic instability + regional hyperinflation - oxygenation target: SpO2 > 90%, PaO2 >60mmHg - carbon dioxide target: ARDSnet aimed for a normal CO2 -> but lung is exposed to repeated tidal stretch, ideally hypercapnia should be minimised but there isn’t compelling data to suggest it is harmful unless there is an obvious reason (raised ICP, pregnancy). OTHER TECHNIQUES TO IMPROVE OXYGENATION - prone posture: improves oxygenation but only trend towards decrease in mortality - inhaled iNO: optimisation of V/Q mis-match, 1-60ppm, on 40-70% will respond, monitor for metHb - inhaled prostacycline (PGI2): optimisation of V/Q mis-match, 1-50ng/kg/min, as effective as iNO PHARMACOLOGICAL THERAPY - surfactant replacement therapy: theoretically good, improves oxygenation but no improvement in mortality, problems with distribution to alveoli - glucocorticoids: improvement in ventilator free days and shock, no improvement in mortality and increase in weakness - ketoconazole: antifungal that inhibits thromboxane synthase and 5-lipooxygenase -> early data but not confirmed. - others: cytokine antagonism, NSAIDS, scavengers of O2 radicals, lisofylline -> no success, APC in sepsis Prognosis - pulmonary function returns to normal @ 6-12 months - occasionally patient have severe restrictive lung disease - although this is the case, many patient have a severe reduction and pulmonary QOL -> depression, anxiety and PTSD are common - patient often have cognitive impairment -> these correlate with the period and severity of hypoxia Jeremy Fernando (2011)