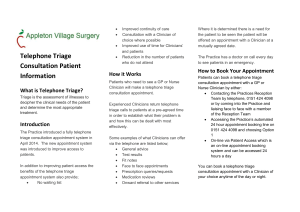
Patient Participation Action 3
advertisement

Patient Participation Action 3 Action 3 - Review of Ability to Speak to GP or Nurse on the Phone. Internal review followed by detailed discussion with the Patient Participation Group. To include review of how patient requests to speak to a clinician are managed and how those call backs to patients are made. Could call back times be more specifically managed? Review to include publication of how and when patients can access clinicians by telephone work, published on website and in practice leaflet. The practice has looked at patient telephone consultations with both the GPs and the nurses. Patients call the surgery and ask to speak to a GP. They are put down for a call back and this is done usually at the end of the GPs clinical session. Often patients don’t answer their call back. It is noted that whilst telephone consultations can save patients being seen by a clinician they present two major which need to be addressed. The first of these is capacity. The second is clinical safety. Telephone capacity. A typical telephone consultation with a patient takes about 7 minutes. Add to this the time required to update the patients clinical record and the total time for each telephone consultation is not significantly less that if the GP had actually seen the patient. The big problem with capacity is the relevance of those requests to speak to a GP. Often, it is to pass on information about an outpatient appointment that they have been to. Not necessary as we get letters from outpatients detailing the consultation. The problem is it is often very difficult to separate the important calls from the less important calls and prioritising calls becomes nigh impossible. It is up to the clinician to educate the patient. The other problem is just how many calls it is reasonable to expect a GP to manage in a day without compromising their other clinical requirements. We have seen GPs with up to 15 telephone calls in a day and the GP is still making those calls early evening. To address capacity issues we have put the following in place. GP telephone consultations are capped to 7 per day per clinician. This is to allow the GP the time to manage their calls more efficiently. Patients are directed to their usual GP for call back. Patients are discouraged from booking telephone call backs days in advance. With nurses capacity is not a problem as there is a low volume of patient telephone work, and so no cap is in place. Clinical Safety. Telephone medicine can be problematic as the clinician is unable to see the patient and unable to take any observations (BP, pulse, etc). Telephone medicine is high risk and will lead to more significant events. Often patients who are called by the GP are then asked to make an appointment with the duty doctor. This means that care to them can be delayed for as much as half a day or more. For example, a patient calls the surgery at 8.30 and asks for a call back from the GP. The GP calls them at 11.30 and asks them to see the duty GP. The next duty GP appointment is at 16.10. Had the patient been given a duty appointment when they first called they would have been seen at 9.50. A delay of 6 hours. If this plays out with the patient being called after the surgery has closed, then the patient is transferred to the care of the ambulance service or asked to make a duty appointment the next day. Not ideal. Timed call backs We have reviewed the use of making call backs to patients at specific times. This might work if all GPs ran their clinics to time (ie. no patient took over ten minutes to see). It has been decided that clinicians should first see those patients in the waiting room, except in the case of life threatening emergency. In summary Patients can request a call back from a clinician by calling reception and asking for this. They will be asked to give some detail so that clinicians can prioritise. Patients will usually be called back at the end of the clinician’s clinical session. This might mean that patients are called back early evening. Patients will be educated by the clinician if the clinician feels that the reason for their call is inappropriate.