Assessment of the Neonate

1
RSPT 2353 – Neonatal/Pediatric Cardiopulmonary Care
Assessment of the Neonatal & Pediatric Patient
Lecture Notes
Reference & Reading: Whitaker, Ch 4 & 5
I.
Assessment of the neonate begins when the baby transitions from uterine life to survival outside the uterus. Assessment skills must be keen in determining how the patient is adapting to its new environment. There are several systems in place to gauge how well the baby is transitioning
II.
Assessment begins with: Obstetric, pregnancy and L&D history
III.
Assessment in Labor & Delivery (pg. 100) - Immediately after delivery
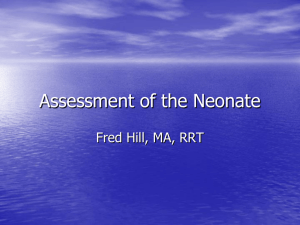
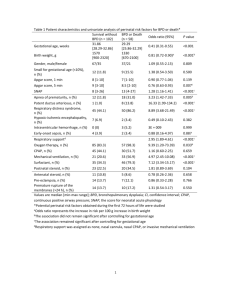
APGAR scores will be assigned
Objectively evaluates the condition of a neonate
Areas examines are: HR, respiratory effort, muscle tone, reflex irritability and color
Each area gets a score of 0, 1, or 2; assessed at 1 and 5 minutes and if necessary then every 5 minutes up to 20 minutes
A
Score
Appearance
0
Pale or blue
1
Body pink, extremities blue
2
Pink
P
G
Absent
None
>100
Cry
A
R
Pulse
Grimace
Activity
Respiratory Effort
Limp
Absent
<100
Some
Some flexion
Irregular
Well flexed
Regular/Crying
IV.
Assessing Gestational Age a.
Dubowitz: Several criteria when examined determine gestational age
Accurate within first 2 weeks of life, consistent results in first 5 days
Uses 11 physical signs and 10 neurologic signs
Each sign is assigned a score from 1 to 5
The score will add up to gestational age b.
Ballard:
Modified the Dubowitz to shorten time for assessment
Looks at 6 physical and neurologic signs
Can assess from 22 to 44 weeks, between 30 and 42 hours of life c.
Using physical exam to determine gestational age
Very quick , easily and relatively reliable, especially during resuscitation
Can be determined in < 1minute if skilled
1.
V
ERNIX
– white, cream-cheese material that covers fetus a.
Appears around 20-24 weeks b.
Very thick until 36 weeks c.
Disappears at 41-42 weeks
2
2.
3.
4.
5.
6.
7.
8.
S
KIN
M
ATURITY a.
25 -26 weeks or less skin is very gelatinous , transparent, & vessels are clearly seen b.
As gestation advances, skin is more pink and vessels are less visible c.
Term neonates will have adult like skin, vessels not visible d.
Post-term neonates, skin will be very wrinkled and sometimes peeling
Lanugo
a.
Fine, downy hair covers fetal body b.
Appears around 26 weeks and covers thorax, head and extremities c.
At 28 weeks it begins to thin d.
It should begin to disappear at 32 weeks
E
AR
R
ECOIL a.
25 – 26 weeks or less will have flat pinna b.
Cartilage is not present until 34 weeks
B
REAST
T
ISSUE a.
25 to 26 weeks or less – not recognizable b.
27 weeks – red circle; no tissue c.
Week 30 – breast bud present
G
ENITALIA a.
25 to 26 weeks or less; Male - scrotum not recognizable, testes have not descended; Female – labia minora & clitoris protrude
S OLE C REASES a.
26 weeks – faint red lines b.
30 weeks – anterior portion of foot c.
34 weeks – 2/3 of the sole d.
Term – covered
E YES
– The baby is considered extremely premature if the eyes remain fused.
V.
Classifying the Neonate – based on weight and exam using a intrauterine growth chart
AGA – appropriate for gestational age
LGA – large for gestational age
SGA – small for gestational age
IUGR – Intrauterine growth retardation
( http://www.aafp.org/afp/980800ap/peleg.html
)
VI.
Examining the Neonate a.
Quiet Exam
Color
Muscle tone
RR – normal 30-60 bpm; tachypnea >60 bpm
Signs that a patient is in respiratory distress
1.
Nasal flaring
2.
Grunting
3.
Retractions
Silverman score can gauge how much distress a patient is in
1.
Scores 0 – 10
2.
High score = distress, low score = none or less distress b.
Physical Exam
Presence of clefts
Chest exam – tactile fremitus
Normal HR 120 – 160bpm ; <100bpm bradycardia
Pulses – abnormal femoral pulses = indication of CHD
BP – see table 5-1;
1.
Mean Blood Pressure
2.
MBP = Gestational age + 5
Abdomen – scaphoid abdomen, enlarged abd
VII.
Examining the Pediatric Patient a.
History b.
RR – evaluating respiratory distress
>1 year: > 40 bpm
> 5 years > 35 bpm
Nasal flaring still possible
Head-bobbing c.
HR & BP is dependent on age or baseline d.
ABGs should be normal or baseline
3