PREOPERATIVE DIAGNOSIS: Tetralogy of Fallot
advertisement
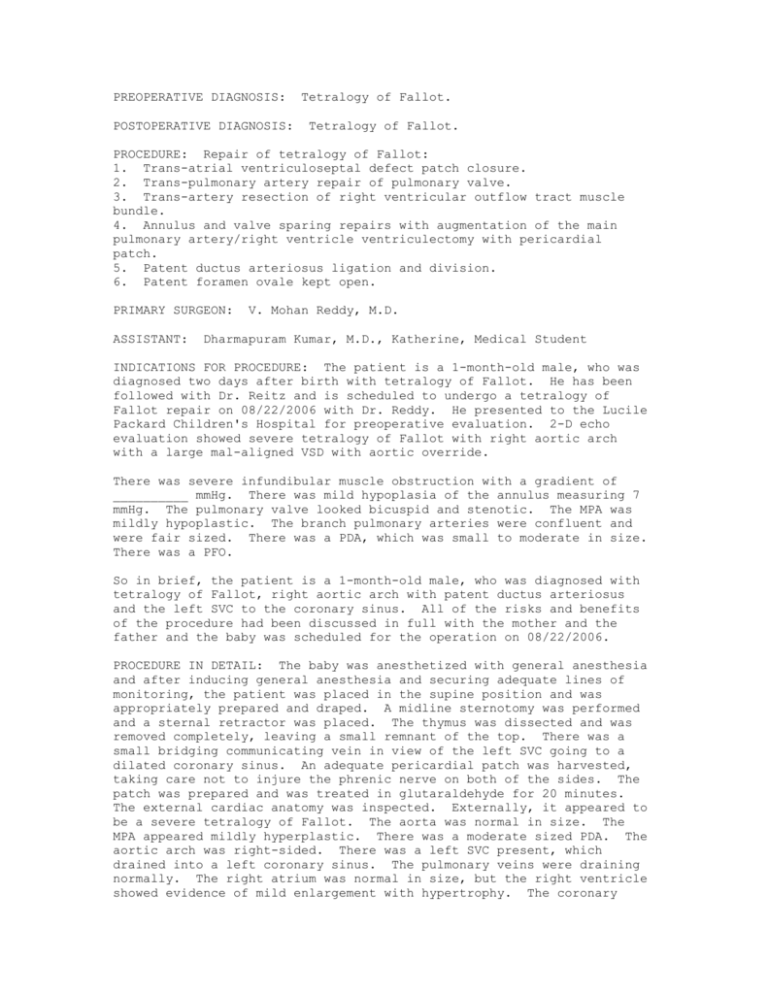
PREOPERATIVE DIAGNOSIS: POSTOPERATIVE DIAGNOSIS: Tetralogy of Fallot. Tetralogy of Fallot. PROCEDURE: Repair of tetralogy of Fallot: 1. Trans-atrial ventriculoseptal defect patch closure. 2. Trans-pulmonary artery repair of pulmonary valve. 3. Trans-artery resection of right ventricular outflow tract muscle bundle. 4. Annulus and valve sparing repairs with augmentation of the main pulmonary artery/right ventricle ventriculectomy with pericardial patch. 5. Patent ductus arteriosus ligation and division. 6. Patent foramen ovale kept open. PRIMARY SURGEON: ASSISTANT: V. Mohan Reddy, M.D. Dharmapuram Kumar, M.D., Katherine, Medical Student INDICATIONS FOR PROCEDURE: The patient is a 1-month-old male, who was diagnosed two days after birth with tetralogy of Fallot. He has been followed with Dr. Reitz and is scheduled to undergo a tetralogy of Fallot repair on 08/22/2006 with Dr. Reddy. He presented to the Lucile Packard Children's Hospital for preoperative evaluation. 2-D echo evaluation showed severe tetralogy of Fallot with right aortic arch with a large mal-aligned VSD with aortic override. There was severe infundibular muscle obstruction with a gradient of __________ mmHg. There was mild hypoplasia of the annulus measuring 7 mmHg. The pulmonary valve looked bicuspid and stenotic. The MPA was mildly hypoplastic. The branch pulmonary arteries were confluent and were fair sized. There was a PDA, which was small to moderate in size. There was a PFO. So in brief, the patient is a 1-month-old male, who was diagnosed with tetralogy of Fallot, right aortic arch with patent ductus arteriosus and the left SVC to the coronary sinus. All of the risks and benefits of the procedure had been discussed in full with the mother and the father and the baby was scheduled for the operation on 08/22/2006. PROCEDURE IN DETAIL: The baby was anesthetized with general anesthesia and after inducing general anesthesia and securing adequate lines of monitoring, the patient was placed in the supine position and was appropriately prepared and draped. A midline sternotomy was performed and a sternal retractor was placed. The thymus was dissected and was removed completely, leaving a small remnant of the top. There was a small bridging communicating vein in view of the left SVC going to a dilated coronary sinus. An adequate pericardial patch was harvested, taking care not to injure the phrenic nerve on both of the sides. The patch was prepared and was treated in glutaraldehyde for 20 minutes. The external cardiac anatomy was inspected. Externally, it appeared to be a severe tetralogy of Fallot. The aorta was normal in size. The MPA appeared mildly hyperplastic. There was a moderate sized PDA. The aortic arch was right-sided. There was a left SVC present, which drained into a left coronary sinus. The pulmonary veins were draining normally. The right atrium was normal in size, but the right ventricle showed evidence of mild enlargement with hypertrophy. The coronary artery anatomy appeared normal. Preparations were made for cardiopulmonary bypass. The aorta and the main pulmonary artery were dissected gently, very carefully and the PDA was looped with 5-0 Prolene and the PDA was resected. It was looped with 5-0 Prolene for transfixation to be done after establishing cardiopulmonary bypass. Pursestring sutures were placed on the aorta and both arteries, the SVC and the IVC. The heparin was administered. A #8 aortic cannula was placed in the aorta and both of the cavae were cannulated with #12 angled venous cannulae. Cardiopulmonary bypass was established and cooling started to achieve a core temperature of 28 degrees Centigrade. After establishing cardiopulmonary bypass, the PDA was immediately ligated with 5-0 Prolene transfixation suture. The PDA was ligated and divided in between two transfixation sutures of 5-0 Prolene and the aortic end was clipped with a medium size Hemoclip. Both of the cavae were looped in preparation for snugging. The main pulmonary artery was resected and the branch of the pulmonary artery was mobilized. The main pulmonary artery appeared mildly hypoplastic along with the mildly hypoplastic annulus, but the branch pulmonary arteries appeared confluent and were adequate in size. A #10 vent was placed into the left ventricle from the right superior pulmonary vein across the LA. After achieving the desired hypothermia, topical cooling of the heart was performed and at the aortic root a pursestring was placed for placing the cardioplegia needle. The aorta was crossclamped at a temperature of 28 degrees Centigrade and cold crystalloid cardioplegia was given. Both of the cavae were snugged and the right atrium was opened and the cardioplegia was let out. After achieving cardiac asystole, the main pulmonary artery was opened longitudinally in between two stay sutures, which were placed, one above the annulus and one below the bifurcation of the main pulmonary artery. The opening of the main pulmonary artery was longitudinal extending from just above the annulus to the level of the bifurcation. The pulmonary valve was inspected and was found to be bicuspid. The leaflets of the pulmonary valve appeared fairly thin without mitral thickening. They showed evidence of fusion of both the commissures. A commissurotomy was performed carefully by opening the commissural __________ and both of the commissures onto the annulus and after this, the valve and annulus were inspected and were found to be adequate from the pulmonary artery end. Following this, the right ventricle outflow was opened by an appropriately placed ventriculotomy in the region of the right ventricle below the level of the annulus of the pulmonary valve. In other words, the annulus was spared by not cutting across the annulus. After making the ventriculotomy, the infundibular muscle obstruction was examined and the muscle bundles were excised to open up the right ventricle outflow tract. The excision of the muscle bundle was done to the level of the annulus, but sparing the annulus and the pulmonary valve. A #8 Hegar dilator was placed through the ventriculotomy across the annulus into the main pulmonary artery and it was sized and found to be adequate. Hence, a decision was made to do an annulus-sparing repair by not cutting across the annulus and achieving the repair from both the pulmonary artery and the right ventriculotomy sites. Following this, the right atrium was inspected for evaluation of the VSD. The VSD was found to be large and mal-aligned with significant aortic override. The VSD was repaired with a pericardial patch that was already treated with glutaraldehyde. The patch was appropriately repaired to match the size of the VSD and the closure was done with 6-0 Prolene continuous suture. The suturing was started at the 3 o'clock position and continued superiorly towards the aortic valve, taking care not to injure the chordae of the tricuspid valve. At the superior end, the sutures were brought out through the septal leaflet of the tricuspid valve at the aortic mound. Inferiorly, the suturing of the VSD patch was continued posteroinferiorly in a continuous fashion away from VSD margin, taking care not to injure the __________. At the posterior inferior angle of the VSD, the suture was brought out the septal leaflet of the tricuspid valve into the right atrium. On the site of the septal leaflet of the tricuspid valve, the VSD was closed with a series of interrupted mattress sutures of 6-0 Prolene that were taken through a small pledget of pericardium. In other words, this margin was repaired with four interrupted mattress sutures of 6-0 Prolene. All of the sutures were tied down to the septal leaflet of the tricuspid valve. A continuous suture of 6-0 Prolene was tied at the superior end and the inferior end onto the nearest mattress suture of 6-0 Prolene to complete the VSD closure. Following this, cold slush cardioplegia was repeated from the aortic root, taking care that the aortic root was adequately de-aired by making a small arteriotomy at the root of the aorta. After repeating the cardioplegia, the VSD closure was completed on the side of the septal leaflet of the tricuspid valve. Following completion of the VSD closure, the atrial septum was inspected and was found to have a patent foramen ovale with the valve. This PFO was kept open. Following this, preparations were made to release the aortic crossclamp by stopping the left atrial vent and de-airing the aortic root adequately. The aortic crossclamp was released. After releasing the right aortic crossclamp, the heart started to regain its rhythm gradually. Rhythm was slowly established. On beating heart, the main pulmonary artery and the right ventricular infundibulum were augmented with a pericardial patch as follows: On the main pulmonary artery, the pericardial patch augmentation was performed with an oval-shaped pericardial patch that was sutured with 6-0 Prolene continuous suture all around and with interrupted sutures of 7-0 Prolene towards the annulus. After this, the RV ventriculotomy was augmented with another pericardial patch that was sutured to the ventriculotomy incision with 6-0 Prolene continuous suture all around, but with interrupted sutures of 6-0 Prolene towards the annulus. This technique of placing interrupted sutures at the level of the annulus for augmenting both the MP and the ventriculotomy was mainly to prevent a pursestring effect. After augmentation of the main pulmonary artery and the right ventriculotomy, the right atrium was closed with 6-0 Prolene continuous suture. The caval snuggers were released and rewarming was slowly completed. At this juncture, the left atrial vent was removed and the left atrial line was placed into the left atrium. At the end of the re-warming, preparations were made to wean the heart off CPB. Intraoperative TEE was done for evaluation of the repair. Moderate inotropic support was started with 5 mg of dopamine and 0.5 of milrinone and an infusion of calcium. This was done through the jugular vein. The heart was weaned off cardiopulmonary bypass with moderate inotropic support and with stable hemodynamics. The rhythm appeared to be in sinus rhythm and the myocardium showed good contraction. Intraoperatively showed a good repair with an intact VSD patch without any significant residual defects in the patch. There was no significant gradient in the RV outflow and the pulmonary valve showed good coaptation and without a significant gradient. There was no evidence of tricuspid regurgitation. The PFO was shunting left to right. The right ventricle and the left ventricle showed good contraction and no residual valve motion abnormality. There was evidence of good blood flow into the patched pulmonary arteries. After ascertaining an adequate repair by an intraoperative TEE, Protamine was administered and the patient subsequently underwent decannulation. The hemodynamics remained stable with good saturations and with acceptable left atrial pressures. Two atrial pacing wires and two ventricular pacing wires were placed. The left chest was opened widely and a #15 Blake was placed to drain fluid out. Decannulation was performed and hemostasis was checked at all of the cardiotomy sites including the ventriculotomy sites. After ascertaining adequate hemostasis, a #20 chest tube was placed in the mediastinum from the right side. The sternum was closed with steel wires and the subcutaneous tissue and the skin were closed in the usual fashion. The baby was transferred to the CVICU with stable hemodynamics and saturations and with acceptable LV pressures and without significant mediastinal bleeding.