It`s Due to Reflux – Or is it
advertisement

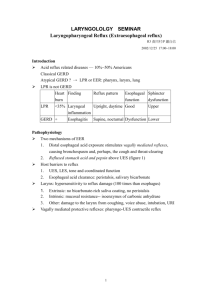
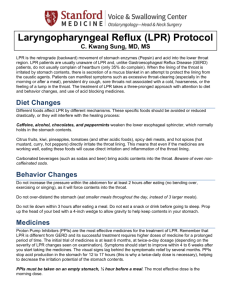
It’s Due to Reflux – Or is it? Reflux causes everything – or so it often seems when we read both scientific and lay journals and magazines on this subject. Reflux has been implicated in causing a great variety of maladies of the upper aerodigestive tract ranging from sinusitis to dysphagia to cancer. What is the truth? How can we accurately diagnose and treat reflux? In the last decade a large volume of scientific literature has been published on these topics, but many of the answers are anything but clear. In this short space I hope to summarize some of our current knowledge about laryngopharyngeal reflux and will also highlight some areas of uncertainty. What is reflux? First a few definitions. Laryngopharyngeal reflux (LPR) is the retrograde flow of gastric contents to the laryngopharynx. This is different than gastroesophageal reflux disease (GERD) where there are gastric contents refluxing back into the distal or mid esophagus. GERD has been studied longer than LPR and reasonably good data exists on how much acid exposure to the distal esophagus constitutes an abnormal amount. GERD is frequently associated with heartburn and can be diagnosed in a variety of ways including endoscopy and distal pH probe testing where a standardized scoring system exists. LPR is much more problematic. Though studies are continuing, there is no accepted standard for the measurement of the amount of gastric contents coming up through the upper esophageal sphincter. In GERD, repeated exposure of the distal esophagus to a pH below 4 is considered to be damaging. We all, however, have some distal reflux(which is considered normal) and our distal esophagus is generally able to tolerate some acid exposure without substantial negative impact. With LPR, exposures to pH values below 4 are certainly damaging, but many feel that pH values much higher than this could also be damaging as the epithelium lining the laryngopharynx is not adequately equipped to handle such exposures. Even relatively short exposures of the pharynx to gastric contents could be damaging. If every short episode of lower esophageal reflux also came all the way up into the pharynx this could be problematic. One could therefore see how LPR could occur in the absence of GERD. So even though it is understood that LPR is retrograde flow into the laryngopharynx, the exact definition of what constitutes an abnormal amount of flow or pH of the refluxate remains unknown. Diagnosis History. Multiple symptoms can occur with LPR. Some of the more common manifestations include throat irritation, chronic cough, lump in throat sensation, and hoarseness. Belafsky et al have developed a self-administered tool, the Reflux Symptom Index which can aid in determining the likelyhood of LPR. (Figure 1) Laryngeal Exam. With improvement in fiberoptic and digital technology, very detailed exams of the larynx are easily performed. Unfortunately exam findings are nonspecific and are those of chronic inflammation and irritation. Major findings include posterior commissure edema, subglottic edema, erythema, ventricular obliteration, diffuse edema, and granuloma.(Figure 2) While some studies have shown that these findings correlate well with documented LPR, others have shown poor correlation and have noted these changes in a good number of individuals without other evidence of reflux disease. Dental Exam. We tend to focus on laryngeal findings, but dentists have known for some time that gastric contents can damage the dentition. In those with bulimia or with severe LPR enamel erosion can be seen particularly on the lingual surface of the teeth. (Figure 3) pH Probe. 24-hour pH probe monitoring can be done to provide more information regarding the amount of laryngopharyngeal reflux occurring. It is important that this test not be done in the standard fashion where the probe is positioned 5cm above the lower esophageal sphincter. This will aid in diagnosing GERD but is not helpful with LPR. When performing a pH probe for LPR, the proximal pH sensor is typically placed just above the upper esophageal sphincter. This is another area of controversy as there is no well-established standardized placement technique or scoring system. Despite these shortcomings this is still likely the most accurate test that is widely available. More studies are coming out where a multichannel intraluminal impedance probe has been used to examine both acid and nonacid reflux events, but even less standardization exists at this point. Esophagoscopy. Esophagoscopy is often used for the diagnosis and monitoring of complications related to GERD. This approach is not nearly as helpful for LPR. Specific Disease Entities Though symptoms of LPR are often nonspecific, there are a variety of disease entities that may be caused by or made worse by LPR. The following is a list of these entities with a brief synopsis of current literature regarding their association with LPR. Sinusitis. Several studies have found that chronic rhinosinusitis occurs more frequently in those with LPR than in those without. Also medically refractory sinusitis has been associated with a higher likelihood of LPR. Though is an association, it is unclear if LPR is a coexistant disease processes or actually a cause of rhinosinusitis. Otitis media. Studies are inconsistent. Pepsin(apparently from the stomach) has been found in the middle ear of children with chronic otitis media, though a clear causative relationship has not been determined. Postnasal drainage. It appears that LPR is one potential cause. Postnasal drainage is extremely nonspecific and so common that other causes also always need to be considered. Cough/sore throat. In certain instances LPR may directly cause a cough and sore throat. Again, these symptoms are nonspecific and other causative factors are possible. Irritable larynx. This diagnosis can be a bit difficult in and of itself. At our Voice Center we do frequently see individual who fall into this category. Typical presentations include cough, tightness, and laryngospasm that can occur with exercise, changes in temperature or exposure to irritants. There is little scientific data to prove the LPR is a factor, though empiric treatment for LPR seems to help some individuals. Hoarseness. LPR can lead directly to hoarseness and can contribute to formation of laryngeal granulomas. Several studies have shown improvement in granulomas with treatment for reflux. Dysphagia/globus. Reflux can lead to dysphagia. A globus-type sensation in the throat is frequently associated with LPR though good studies are lacking. Airway stenosis. It is generally accepted that LPR can lead to or at least contribute to the development of subglottic and tracheal stenosis. Cancer. Studies are not terribly definitive. LPR does not appear to be a large risk factor for the development of laryngeal carcinoma. Treatment Behavioral changes. Patients should be educated on maintaining an appropriate weight, smoking cessation and an appropriate diet. Dietary changes would include restriction of caffeine, fats, tomato-based products, alcohol, and late-night meals. Medical management. Several categories of medications have been used to treat reflux: proton pump inhibitors(PPIs), H2 – receptor blockers, mucosal cytoprotectants, prokinetic agents, and antacids. PPIs are the mainstay of treatment. Typically a 3 month trial is needed to determine if the treatment is beneficial. It is important to take these medications approximately 30 minutes prior to eating and it should be noted that BID treatment may be necessary. Should no significant improvement occur within 3 months, more definitive testing such as pH monitoring should be considered. It is not infrequent that a patient feels improvement with treatment and yet laryngeal findings of reflux continue to persist. The significance of this is unknown. H2 blockers such as ranitidine may be of some benefit though are less effective than the PPIs. Mucosal cytoprotectants and antacids play a larger role in relief of GERD than in LPR. Prokinetic agents have largely fallen out of favor due to various adverse reactions. Surgery. Laparoscopic fundoplications are now fairly common and have been shown to improve the competency of the lower esophageal sphincter. It is not completely clear how well theses laparscopic procedures will hold up long-term. Conclusion LPR is an entity that has received much attention in recent years. While medications have improved and research has continued, accurate diagnosis often remains elusive as symptoms and exam findings are frequently nonspecific. We, as clinicians, should be aware of the potential symptoms that reflux may cause and at the same time should realize – reflux does not cause everything.