13: Skin - Gateshead
advertisement
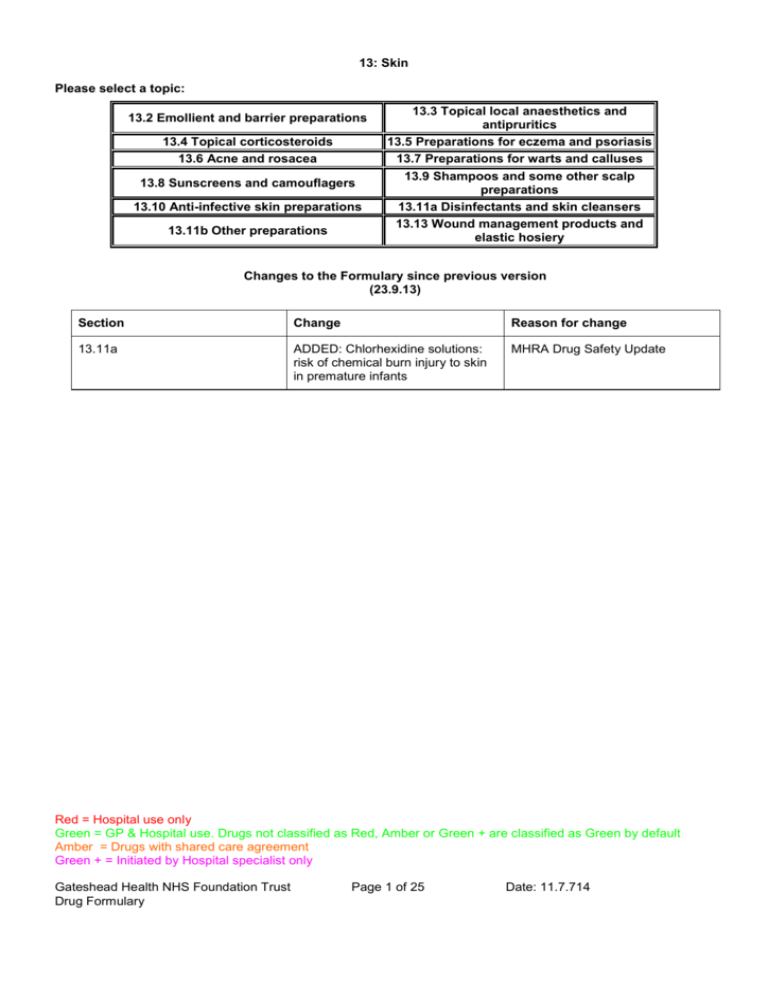
13: Skin Please select a topic: 13.2 Emollient and barrier preparations 13.4 Topical corticosteroids 13.6 Acne and rosacea 13.8 Sunscreens and camouflagers 13.10 Anti-infective skin preparations 13.11b Other preparations 13.3 Topical local anaesthetics and antipruritics 13.5 Preparations for eczema and psoriasis 13.7 Preparations for warts and calluses 13.9 Shampoos and some other scalp preparations 13.11a Disinfectants and skin cleansers 13.13 Wound management products and elastic hosiery Changes to the Formulary since previous version (23.9.13) Section Change Reason for change 13.11a ADDED: Chlorhexidine solutions: risk of chemical burn injury to skin in premature infants MHRA Drug Safety Update Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 1 of 25 Date: 11.7.714 13.1 Management of skin conditions The vehicle used in topical preparations influences skin hydration, has a mild antiinflammatory effect and facilitates penetration of the active component. Creams are more cosmetically acceptable than ointments. Gels are suitable for application to the face and scalp while lotions are used for moist conditions and hairy areas. Ointments are much less likely to sensitise and are suitable for chronic dry lesions. Possible contact sensitivity to preservatives or antiseptics is the reason for the range of topical agents. Body area Non-corticosteroid cream/ointment Face 15 to 30g (Qty based on twice daily application for 1 week in adults) Face and neck Corticosteroid cream/ointment (Qty based on single daily application for 2 weeks in adults) 15 to 30g Both hands 25 to 50g 15 to 30g Scalp 50 to 100g 15 to 30g Both arms 100 to 200g 30 to 60g Both legs 100 to 200g 100g Trunk 400g 100g Groins and genitalia 15 to 25g 15 to 30g Fire Hazard with Paraffin-based Emollients Emulsifying ointment or 50% liquid paraffin and 50% white soft paraffin ointment in contact with dressings and clothing is easily ignited by a naked flame. The risk will be greater when these preparations are applied to large areas of the body, and clothing or ointment become soaked with the ointment. Patients should be told to keep away from fire or flames and not to smoke when using these preparations. The risk of fire should be considered when using large quantities of any paraffin-based emollient. For further information refer to NPSA Rapid Response Report 4 dated 26.November 2007 The following products are known to be paraffin based: STEROIDS EMOLLIENTS Betnovate ointment Cetreban Cream & bath additive Betnovate RD ointment Dermol Cream, 500 lotion & 600 Bath Additive Diprobase and Diprobath Doublebase E45 Cream and Bath Oil Emulsifying Ointment Epaderm Hydromol Ointment and Bath additive Oilatum Cream and Bath additive Yellow soft paraffin Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 2 of 25 Date: 11.7.714 STEROIDS cont. EMOLLIENTS cont. ZeroCream Zerobase Zerolatum Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 3 of 25 Date: 11.7.714 13.2 Emollient and barrier preparations Emollients (moisturisers) Aqueous cream 100g & 500g OR ZeroAQS cream 100g & 500g Aveeno cream 100g Calmurid cream 100g Cetraben emollient cream 500g Dermol cream 500g – for short term use only Diprobase cream 500g OR Zerobase cream 500g Diprobase ointment 500g E45 cream 50g & 500g OR Zerocream 50g & 500g Emulsifying ointment 500g Eucerin Intensive 10%w/w Urea Treatment Lotion 250ml (Paeds only) Hand cream 50g (STAFF USE ONLY) Hydromol Ointment 125g & 500g Oilatum cream 150g (Paeds only) Oilatum Junior Cream 500ml & 1050ml (Paeds only) Yellow soft paraffin 15g Dose - Aqueous cream BP OR ZeroAQS (emulsifying ointment 30%, phenoxyethanol 1% in freshly boiled and cooled purified water) (100g): massage into skin 2-3 times daily; may be used as a soap substitute. - Aveeno® cream (colloidal oatmeal in emollient basis) (100mL): apply as often as required. - Calmurid cream (urea 10%, lactic acid 5%): apply twice a day. - Cetraben emollient cream (white soft paraffin 13.2%, light liquid paraffin 10.5%): apply twice a day. - Dermol cream (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride 0.1% w/w; Liquid Paraffin 105% w/w; Isopropyl Myristate 10% w/w): apply as often as required - Diprobase® cream OR Zerobase (cetomacrogol 2.25%, cetostearyl alcohol 7.2%, liquid paraffin 6%, white soft paraffin 15%) (50g tube, 500g dispenser): apply as often as required. - Diprobase® ointment (liquid paraffin 5%, white soft paraffin 95%) (50g tube, 500g dispenser): apply as often as required. - E45 Cream OR Zerocream (light liquid paraffin 12.6%, white soft paraffin 14.5%, hypoallergenic anhydrous wool fat 1% in self-emulsifying monostearin): apply as often as required. - Eucerin® Intensive cream (urea 10%): apply thinly and rub into area twice a day. - Hydromol® ointment (yellow soft paraffin 30%, emulsifying wax 30%): apply as often as required; may be used as a soap substitute. - Oilatum cream (light liquid paraffin 6%, white soft paraffin 15%): apply as often as required. - Oilatum Junior Cream (light liquid paraffin 6%, white soft paraffin 15%) Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 4 of 25 Date: 11.7.714 - Yellow soft paraffin (yellow petroleum jelly): apply as often as required. Prescribing notes Choice is guided by individual patient tolerance, preference and ease of use. It is dependent on previous use and adverse skin reactions (some may cause irritation or burning so advise testing on a small area of skin first and stop if a reaction occurs). Emollients soothe, smooth and hydrate the skin and are indicated for all dry scaling disorders. Emollients should be applied regularly to maintain improvement; most are best applied after a shower or bath. Use an oil-based emollient at night and during the day if skin is very dry/flaky. Use a cream which is easier to apply and less greasy throughout the day to aid compliance. These products, apart from white soft paraffin 50%/liquid paraffin 50%, may be used as soap substitutes by firstly wetting the skin, washing with the cream or ointment, then rinsing off. If emollients are being applied to the whole body twice daily, children may need 250g – 500g per week and adults 500g per week. It is most cost effective to prescribe emollients in very large quantities Hydromol contains less additives that Epaderm. Epaderm is now non-formulary Aqueous cream and emulsifying ointment should be used for washing only. Preparations that come in a pump dispenser presentation are good when product needed for use at school as more hygienic. Ointments should be used for dry skin and chronic eczema. Creams should be sued for acute inflammatory eczema. Aqueous cream and ZeroAQS cream can be considered the same. E45 cream and Zerocream can be considered the same. Diprobase cream and Zerobase cream can be considered the same. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 5 of 25 Date: 11.7.714 Emollient bath additives Aveeno bath oil 250ml (Paeds only) Balneum bath oil 200ml (Paeds only) Dermol 600 600ml – for short term use only E45 emollient bath oil 500ml (Paeds only) Hydromol emollient bath additive 500ml (Paeds only) Oilatum emollient bath additive 250ml OR Zerolatum 500ml Oilatum Plus bath additive 500ml (Paeds only) Cetraban emollient bath additive 500ml (Paeds only) Zerolatum bath additive Dose - Cetraban Emollient bath additive (light liquid paraffin 82.8%) (500mL): add 1-2 capfuls to bath (1/2 to 1 capful if child). - Oilatum® Emollient bath additive OR Zerolatum (acetylated wool alcohols 5%, liquid paraffin 63.4%) (250mL): add 5-15 mL/bath (2.5-10mL if an infant). - Balneum® bath oil (soya oil 84.75%) (200mL, 500mL, 1L): add 20mL/bath (5mL, if an infant). - Aveeno® bath oil (colloidal oatmeal, white oat fraction in emollient basis (250mL): up to 30mL/bath (child, up to 30mL). - Oilatum® Plus bath additive (benzalkonium chloride 6%, triclosan 2%, light liquid paraffin 52.5%) (500mL, 1L): 1-2 capfuls/bath (infant over 6 months, 1mL). - Dermol® 600 Bath Emollient (benzalkonium chloride 0.5%, liquid paraffin 25%, isopropyl myristate 25%) (600mL): up to 30mL/bath (infant up to 15mL). - Hydromol® Emollient Bath Additive (isopropyl myristate 13%, light liquid paraffin 37.8%) (500ml): up to 1-3 capfuls/bath. - E45® Emollient Bath Oil (cetyl dimeticone 5%, liquid paraffin 95%) (500ml): up to 15ml/bath. Prescribing notes Bath additives with antiseptic should be used in patients with infected eczema. Oilatum® Plus bath additive is not suitable for use in the shower. Preparations containing benzalkonium chloride can cause skin irritation with continued use. E45® Emollient Bath Oil contains no irritants or allergens. Oilatum and Zerolatum can be considered the same. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 6 of 25 Date: 11.7.714 Soap substitutes Aqueous cream 100g & 500g Emulsifying ointment 500g Hydromol ointment 500g Dermol 500 lotion 500ml (Paeds only. Not for longterm use) Dermol 200 shower emollient 200ml (Paeds only) Doublebase gel 100g, 500g (Paeds only) Oilatum shower emollient gel 150g(Paeds only) Dose - Emulsifying Ointment (emulsifying wax 30%, white soft paraffin 50%, liquid paraffin 20%) - Aqueous cream BP (emulsifying ointment 30%, phenoxyethanol 1% in freshly boiled and cooled purified water) (100g) - Hydromol® ointment (yellow soft paraffin 30%, emulsifying wax 30%) (500g) - Dermol 500 lotion (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride 0.1% w/w; Liquid Paraffin 2.5% w/w; Isopropyl Myristate 2.5% w/w): apply as often as required; may be used as a soap substitute. - Dermol 200 shower emollient (Benzalkonium Chloride 0.1% w/w; Chlorhexidine Hydrochloride 0.1% w/w; Liquid Paraffin 2.5% w/w; Isopropyl Myristate 2.5% w/w): apply as often as required; may be used as a soap substitute. - Doublebase gel (Liquid paraffin 15%; Isopropyl Myristate 15%): apply as often as required. - Oilatum shower emollient gel (light liquid paraffin 70%): apply as often as required. Prescribing notes Most emollients may be used as soap substitutes by firstly wetting the skin, washing with the cream or ointment, then rinsing off. White soft paraffin 50%/liquid paraffin 50% is not suitable as a soap substitute. Hydromol contains less additives than Epaderm® Preparations containing benzalkonium chloride can cause skin irritation with continued use. A convenient way to apply emulsifying ointment and Hydromol® ointment is as "soap balls", which are made by putting a scoop of the ointment into tubinette or stockinette. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 7 of 25 Date: 11.7.714 Barrier preparations Vasogen cream 50g Drapolene cream 100g Metanium ointment 30g Dose - Vasogen Cream (dimeticone 20%, calamine 1.5%, zinc oxide 7.5%)): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change. - Drapolene Cream (benzalkonium chloride 0.01%, cetrimide 0.2% in a basis containing white soft paraffin, cetyl alcohol and wool fat): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change. - Metanium Ointment (titanium dioxide 20%, titanium peroxide 5%, titanium salicylate 3% in basis containing dimeticone, light liquid paraffin, white soft paraffin, and benzoin tincture): for nappy and urinary rash and eczematous conditions, apply several times daily as necessary or after each nappy change. Prescribing notes Urinary (nappy) rash may clear if skin is left exposed to air; if associated with yeast (candida) infection, an antifungal cream such as clotrimazole cream is useful. For information on the use of Cavilon® please consult the separate Trust Wound Care Formulary. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 8 of 25 Date: 11.7.714 13.3 Topical local anaesthetics and antipruritics a) Topical antipruritics Calamine lotion 200ml (for inpatient use only) Dose - Calamine lotion: apply 2-3 times daily. Prescribing notes Emollient preparations may be useful for pruritus due to dry skin; sedating oral antihistamines may also be helpful for itch (b) Topical local anaesthetics LMX 4® cream Dose - LMX 4® cream (lidocaine 4%) (5g): for children & adults over 1 month, anaesthesia before e.g. venepuncture, apply a thick layer under an occlusive dressing 30 minutes before procedure Prescribing notes Topical local anaesthetics may be absorbed through mucosal surfaces. Local anaesthetics may occasionally cause sensitisation. For information on the use of Ethyl Chloride Spray please consult the Anaesthetics Chapter of the formulary. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 9 of 25 Date: 11.7.714 13.4 Topical corticosteroids Hydrocortisone 0.5% and 1% cream Hydrocortisone 0.5% and 1% ointment Hydrocortisone 1% plus clotrimazole 1% cream (Canesten HC) Hydrocortisone 0.5% plus nystatin and chlorhexidine cream (Nystaform HC) Hydrocortisone 0.5% plus nystatin and chlorhexidine ointment (Nystaform HC) Hydrocortisone 0.5% plus nystatin, benzalkonium and dimeticone (Timodine) Hydrocortisone 1% plus miconazole 2% cream (Daktacort) Betamethasone valerate 0.1% cream (Betnovate) 100g & 30g Betamethasone valerate 0.1% ointment (Betnovate) 100g & 30g Betamethasone valerate 0.1% scalp application (Betnovate) Betamethasone valerate 0.025% cream (Betnovate RD) 100g Betamethasone valerate 0.025% ointment (Betnovate RD) 100g Betamethasone valerate 0.1% plus clioquinol 3% ointment 30g Betamethasone valerate 0.1% plus neomycin 0.5% cream 30g Betamethasone valerate 0.1% plus neomycin 0.5% ointment30g Clobetasol propionate 0.05% cream (Dermovate) 30g Clobetasol propionate 0.05% ointment (Dermovate) 30g Clobetasone butyrate 0.05% cream (Eumovate) 30g & 100g Clobetasone butyrate 0.05% ointment (Eumovate) 30g & 100g Clobetasone butyrate 0.05%, oxytetracycline and nystatin 0.05% ointment (Trimovate) 30g Fluocinolone 0.025% ointment (Synalar) 30g Dose - Topical corticosteroids should be applied thinly as follows: Mild steroids = 1-2 times daily. Moderate, Potent & Very potent steroids = 1 x daily. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 10 of 25 Date: 11.7.714 Prescribing notes Topical corticosteroids are divided into four groups according to potency (see table) below). Mild or moderately potent corticosteroids should control most cases of eczema. Therapy should be stepped-down once control achieved. Potency Examples Trade Name Mild Hydrocortisone 0.5% and 1% Non-proprietary Hydrocortisone with antimicrobials Canesten HC, Timodene, Dakatacort, Vioform-HC Fluocinolone acetonide 0.0025% Synalar 1 in 10 Betamethasone 0.025% Betnovate RD Clobetasone butyrate 0.5% Eumovate Clobetasone with antimicrobials Trimovate Moderate Potent Very Potent Fluocinolone acetonide 0.00625% Synalar 1 in 4 Betamethasone 0.1% Betnovate Fluocinolone acetonide 0.025% Synalar Betamethasone 0.1% with antimicrobials Betnovate C, Betnovate N Clobetasol propionate 0.05% Dermovate Topical corticosteroids are not recommended in urticaria, rosacea, acne or undiagnosed, possibly infective, disorders. Topical corticosteroids must not be applied more than twice a day. To minimise the risk of side-effects, the smallest effective amount should be used, reducing strength and frequency of application as the condition settles. The risk of systemic sideeffects increases with prolonged use on thin, inflamed or raw skin surfaces, use in flexures, or use of more potent corticosteroids. Occlusion increases efficacy and side-effects. Only mild corticosteroids should be used on the face. Gloves should be worn during, or hands washed after, application of large quantities of steroid preparations. The occlusive effect of ointments increases penetration of the corticosteroid. Cream based preparations contain preservatives. Topical corticosteroids should not be used on infected skin unless the infection is being treated. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 11 of 25 Date: 11.7.714 Antibacterials and antifungals with corticosteroids may have a role if there is associated infection. Palms and soles may require potent or very potent steroids. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 12 of 25 Date: 11.7.714 13.5 Preparations for eczema and psoriasis Preparations for eczema PB7 Viscopaste bandages Prescribing notes Medicated bandages are flammable All patients with eczema should use an emollient and soap substitute and/or bath oil. Emollients with antiseptics should be used to in patients with infected eczema. Exacerbation of eczema may represent secondary bacterial or viral infection. Appropriate swabs should be taken, and topical antibacterials applied. Systemic antibiotics may be required in widespread infected eczema. Ciclosporin, azathioprine or systemic corticosteroids should be initiated on specialist advice only, with responsibility for monitoring agreed. Topical corticosteroids should be reduced and withdrawn as the condition settles. Sedating antihistamines may be used short-term for pruritus. Preparations for psoriasis Acitretin 10mg and 25mg capsules Exorex lotion 100ml (prepared coal tar 1% in an emollient basis) Calcipotriol 50microgram/gram cream 60g (Dovenex®) Prescribing notes Treatment choice depends on site, extent of psoriasis and patient preference and tolerance. Potent and very potent topical corticosteroids should be used on specialist advice only; they may precipitate unstable and pustular psoriasis after stopping. Phototherapy, methotrexate, ciclosporin, acitretin should be initiated on specialist advice only, with responsibility for monitoring agreed. Drugs affecting the immune response Ciclosporin 25mg, 50mg and 100mg capsules Methotrexate 2.5mg tablets Tacroliumus 0.03% ointment Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 13 of 25 Date: 11.7.714 13.6 Acne and rosacea Preparations for acne Isotretinoin 5mg and 20mg capsules (on advice on specialist only) Dianette tablets Prescribing notes Topical treatment takes at least 30 days to become effective. Benzoyl Peroxide is available to prescribe by GPs or for sale over the counter. Topical antibiotics are as effective as oral antibiotics but encourage resistance and are more expensive. Topical retinoids are recommended for comedonal acne; they may initially cause redness of the skin. Oxytetracycline may take up to 6 months of compliant use to achieve maximum benefit. Dianette® (cyproterone acetate with ethinylestradiol) is a treatment for severe acne and only in those patients may it also be used as an oral contraceptive. In those who do not require contraception, Dianette® should be withdrawn 3-4 cycles after the treated condition has completely resolved. If ongoing contraception is required, substitution with another COC is likely to maintain the improvement. Some drugs, including enzyme-inducers and antibiotics, may impair the efficacy of oral contraceptives; see BNF for details. Doxycycline can cause photosensitivity in some patients. Minocycline may be an alternative but prolonged use should be avoided due to the rare risk of liver damage; liver function tests should be monitored 3 monthly. Tetracyclines and retinoids (systemic or topical) must be avoided in pregnancy. Severe acne requires oral antibiotics and referral for consideration of isotretinoin for treatment failures. Oral isotretinoin (Roaccutane®) is a toxic and teratogenic drug that is only prescribable by a consultant dermatologist. There is no effective treatment for redness of the skin due to rosacea; camouflagers may be required. Mild rosacea is best treated with a topical agent. Pustular rosacea is best treated with systemic antibiotics. MHRA Drug Safety Update Cyproterone acetate with ethinyloestradiol (co-cyprindiol): balance of benefits and risks remain positive – updated prescribing advice Article date: June 2013 Summary Following a Europe-wide review of cyproterone acetate with ethinylestradiol (co-cyprindiol), the balance of benefits and risks of Dianette (brand leader) and its generics remains positive. To further improve the benefit-risk balance some important changes have been made to clarify the Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 14 of 25 Date: 11.7.714 indication—these are discussed below. Although the indications for co-cyprindiol relate to androgen-sensitive skin conditions and hirsuitism, the medicine also provides effective contraception for women who require it. Use of additional hormonal contraception with cocyprindiol is therefore contraindicated. The risk of venous thromboembolism is rare, but healthcare professionals and patients should remain vigilant for signs and symptoms of this important side effectine. Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON287002 MHRA Drug Safety Update Oral retinioids: pregnancy prevention – reminder of measures to minimise teratogenic risk Article date: June 2013 Summary The risk of foetal malformation with oral retinoids is extremely high, even when used at a low dose or for a short time during pregnancy. All oral retinoids have an associated Pregnancy Prevention Programme (PPP), which is supported by educational material for prescribers, pharmacists, and patients. Women of child-bearing potential should have pregnancy excluded before starting treatment. While taking these medicines, one—or preferably two—different forms of contraception must be consistently used. Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON287004 Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 15 of 25 Date: 11.7.714 13.7 Preparations for warts and calluses Cuplex gel 5g (salicylic acid 11%, lactic acid 4% in collodion basis) Silver nitrate caustic pencil 95% Salicyclic acid 10% in colloidion solution (chiropody) Imiquimod 5% cream 5g Prescribing notes These preparations are contra-indicated in facial or genital warts. The wart surface should be rubbed with a file or pumice stone, and the surrounding skin protected, before each application. If application becomes painful, treatment should be withheld for a few days then recommenced. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 16 of 25 Date: 11.7.714 13.8 Sunscreens and camouflagers Uvistat SPF 30 125g Uvistat SPF 50 125g Prescribing notes Sunscreens with SPF > 15 are prescribable for photosensitive skin disorders including genetic disorders, vitiligo, following radio-therapy, photo-aggravated rosacea, or recurrent herpes simplex labialis. Prescriptions should be endorsed "ACBS". The choice of sunscreens depends on individual patient need, tolerance and evidence of sensitivity to excipients. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 17 of 25 Date: 11.7.714 13.9 Shampoos and some other scalp preparations Polytar shampoo 250ml Ketoconazole 2% shampoo 120ml Cocois scalp ointment 40g OR Sebco ointment Oilatum shampoo Eucerin Dry Scalp Relief shampoo with 5% urea Dose - Ketoconazole 2% shampoo (120mL): for seborrhoeic dermatitis and dandruff apply twice weekly for 2-4 weeks; for pityriasis versicolor, once daily for up to 5 days. - Cocois® scalp ointment (coal tar solution 12%, salicylic acid 2%, precipitated sulphur 4% in a coconut oil emollient basis): for scaly scalp disorders including psoriasis, eczema, seborrhoeic dermatitis and dandruff, apply to scalp once weekly as necessary, shampoo off after 1 hour. - Polytar® liquid (arachis (peanut) oil extract of crude coal tar 0.3%, cade oil 0.3%, coal tar solution 0.1%, oleyl alcohol 1%, tar 0.3%) (250mL): scalp disorders, including psoriasis, seborrhoea, eczema, pruritus and dandruff, apply 1-2 times weekly. - Oilatum® shampoo: Wet the hair and massage OILATUM Scalp Treatment gently over the scalp to produce a lather. Leave on for 3-5 minutes. Rinse thoroughly, and repeat if necessary. Use twice weekly for two weeks to clear the scales and improve the condition of your scalp. Then just use once a week to maintain a clear scalp. Prescribing notes Shampoo formulations are preferred for moderate scaly slap conditions whereas more severe conditions may require an ointment. Ketoconazole shampoo is often helpful for seborrhoeic dermatitis of the scalp. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 18 of 25 Date: 11.7.714 13.10 Anti-infective skin preparations Antibacterial preparations Mupirocin 2% ointment 15g Silver sulfadiazine 1% cream 50g (Flamazine®) Fusidic acid 2% cream 15g Fucidin-H cream 15g Metronidazole 0.75% gel (Anabact) 15g Potassium permanganate solution tablets 400mg (Permitabs®) Octenisan Oilatum Plus (on advice of microbiology/infection control only) Dermol 600 – for short term use only Dose - Fusidic acid 2% cream, gel; sodium fusidate 2% ointment (15g, 30g): apply 3-4 times daily. - Metronidazole gel 0.75% : apply 1-2 times daily. - Silver sulfadiazine cream 1% (20g, 50g, 250g, 500g): burns, apply daily or more frequently if required; leg ulcers, apply every 1 to 2 days; fingertip injuries, apply every 2-3 days. - Potassium permanganate solution tablets 400mg (Permitabs®): 1 tablet dissolved in 4 litres of water provides a 0.01% (1 in 10,000) solution. - Mupirocin 2% ointment; cream (15g): apply up to 3 times daily for up to 3 days. - Fucidin H cream (hydrocortisone acetate 1%, fusidic acid 2%): apply 1-2 times daily. Prescribing notes Topical antibiotics should only be used short-term and for localised infections. If potassium permanganate tablets are prescribed, ensure tablets are dissolved in a jug prior to being poured into the bath as direct contact with the skin can cause burning. Antifungal preparations Clotrimazole 1% cream 20g Canesten-HC cream 30g Amorolfine 5% nail lacquer 5ml Nystatin 100 000 unit/g cream 30g Miconazole 2% cream 15g & 30g Dose - Clotrimazole cream 1% (20g): apply 2-3 times daily. - Terbinafine cream 1% (30g): apply 1-2 times daily. - Clotrimazole HC cream 1% (20g)(clotrimazole 1%, hydrocortisone 1%): apply 2-3 times daily. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 19 of 25 Date: 11.7.714 - Amorolfine nail lacquer 5% (5ml): apply 1-2 weekly. - Miconazole cream 2% (30g): apply 1-2 times daily. Antiviral preparations Aciclovir 200mg and 400mg tablets Parasiticidal preparations Malathion 0.5% in an aqueous basis (Derbac-M) 50ml Permethrin 5% dermal cream (Lyclear) 30g (a) Scabies Dose - Malathion 0.5% liquid in an aqueous basis (Derbac-M®) (50ml): apply over whole body and wash off after 24 hours; if hands are washed with soap within 24 hours they should be retreated. In young children, application may need to be extended to the face, neck, scalp and ears; this extended application may also be necessary for the elderly, immunocompromised and those who have experienced treatment failure. - Permethrin 5% dermal cream (Lyclear® Dermal Cream, 30g): apply over whole body and wash off after 8-12 hours. In young children, application may need to be extended to the face, neck, scalp and ears; this extended application may also be necessary for the elderly, immunocompromised and those who have experienced treatment failure. If hands are washed with soap within 8 hours of application, they should be treated again with cream. Prescribing notes Aqueous preparations are preferable to alcoholic lotions. All members of the household and close contacts should be treated. Clothes and bedlinen should be washed at normal temperatures at time of treatment. In pregnancy, malathion in an aqueous basis is preferred. (b) Head lice Dose - Malathion 0.5% liquid in an aqueous basis (Derbac-M®) (50ml): rub into dry hair and scalp, allow to dry naturally, remove by washing after 12 hours. Prescribing notes Head lice should be treated with lotion or liquid formulations; shampoos are diluted too much during use to be effective and should not be used. Products with short application times (e.g. cream rinse & mousse formulations) are not recommended. A second application 7 days after the first is needed. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 20 of 25 Date: 11.7.714 Aqueous formulations are preferred in severe eczema, asthmatic patients and small children. A rotational policy for insecticides is outmoded; a mosaic strategy is suggested whereby if a course of treatment fails then a different insecticide is used for the next course. Malathion should not be applied at intervals of less than 1 week or for more than 3 consecutive weeks since effectiveness is not increased. In pregnancy, dimeticone or wet combing are preferred. If malathion is required the liquid in aqueous basis should be used. Malathion should not be applied at intervals of less than 1 week or for more than 3 consecutive weeks since effectiveness is not increased. Permethrin is not recommended for the treatment of head lice since currently available formulations are diluted too much during use. (c) Crab lice Dose - Malathion 0.5% aqueous liquid (Derbac-M®) (50mL): apply over whole body, allow to dry naturally, wash off after 12 hours or overnight. Prescribing notes An aqueous preparation should be applied to all parts of the head and body for 12 hours or overnight; a second treatment is needed after 7 days to kill lice emerging from surviving eggs. Alcoholic lotions are not recommended due to irritation of excoriated skin and genitalia. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 21 of 25 Date: 11.7.714 Preparations for minor cuts and abrasions Proflavine cream BPC 100ml (Theatres only) Prescribing notes For information on the use of Cavilon® and Opsite® please consult the separate Trust Wound Care Formulary. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 22 of 25 Date: 11.7.714 13.11 Disinfectants and cleansers Alcohols and saline Methylated spirit external solution 70% Sodium chloride 0.9% sachets 100ml (Normasol) Isopropyl alcohol swabs Chlorhexidine salts Chlorhexidine gluconate 0.05% sachet (Unisept) 25ml & 100ml Chlorhexidine gluconate 0.5% solution (Hibisol and Hydrex) 500ml Chlorhexidine gluconate 4% surgical scrub (Hydrex) 500ml Chlorhexidine gluconate 1% obstetric cream 250g Chlorhexidine gluconate 0.015% and cetrimide 0.15% solution 1L (Travasept) Chlorine and iodine Povidone iodine 7.5% surgical scrub(Videne) 500ml Povidone iodine 2.5% dry powder spray (Betadine) 150g Povidone iodine 10% ointment (Betadine) 80g Povidone iodine 10% antiseptic solution (Videne) 500ml Povidone iodine 10% alcoholic antiseptic solution (Videne) 500ml Other Oilatum Plus 500ml (On advice of microbiology/infection control only) Octenisan 450ml Astringents, oxidisers and dyes Hydrogen peroxide 3% solution 200ml Prescribing notes Sodium chloride solution 0.9% is suitable for irrigation of skin and wounds. Povidone-iodine may produce systemic adverse effects, such as metabolic acidosis, hypernatraemia and renal impairment, if applied to large wounds or severe burns. Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 23 of 25 Date: 11.7.714 MHRA Drug Safety Update Chlorhexidine solutions: risk of chemical burn injury to skin in premature infants Article date: June 2014 Summary Advice for healthcare professionals: When using alcohol-based or water-based chlorhexidine solutions on preterm infants, bear in mind the risk of severe chemical injuries. Use the minimum amount of chlorhexidine solution required and do not allow the solution to pool. Remove any excess solution and any soaked materials, drapes, or gowns from the skin. Monitor patients frequently to detect and manage cutaneous side effects at an early stage. Link: http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON428307 Other preparations Infacare bath solution 500ml Iodine alcoholic solution BP 25ml Plaster remover solution 50ml Sterile water for irrigation 1L Sodium dichloroisoocyanurate external tablets (Haz-tabs) Sodium hypochlorite 2% solution 500ml (Milton) Sodium chloride 0.9% for irrigation 1L Aluminium chloride hexahydrate 20% roll-on 60ml Hirudoid cream 50g Lubricating jelly 42g & sachets Gigasept PA solution 5L Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 24 of 25 Date: 11.7.714 13.13 Wound management products and elastic hosiery See separate wound management formulary Red = Hospital use only Green = GP & Hospital use. Drugs not classified as Red, Amber or Green + are classified as Green by default Amber = Drugs with shared care agreement Green + = Initiated by Hospital specialist only Gateshead Health NHS Foundation Trust Drug Formulary Page 25 of 25 Date: 11.7.714