Assessment of the Respiratory Patient 1. The respiratory therapist is
advertisement
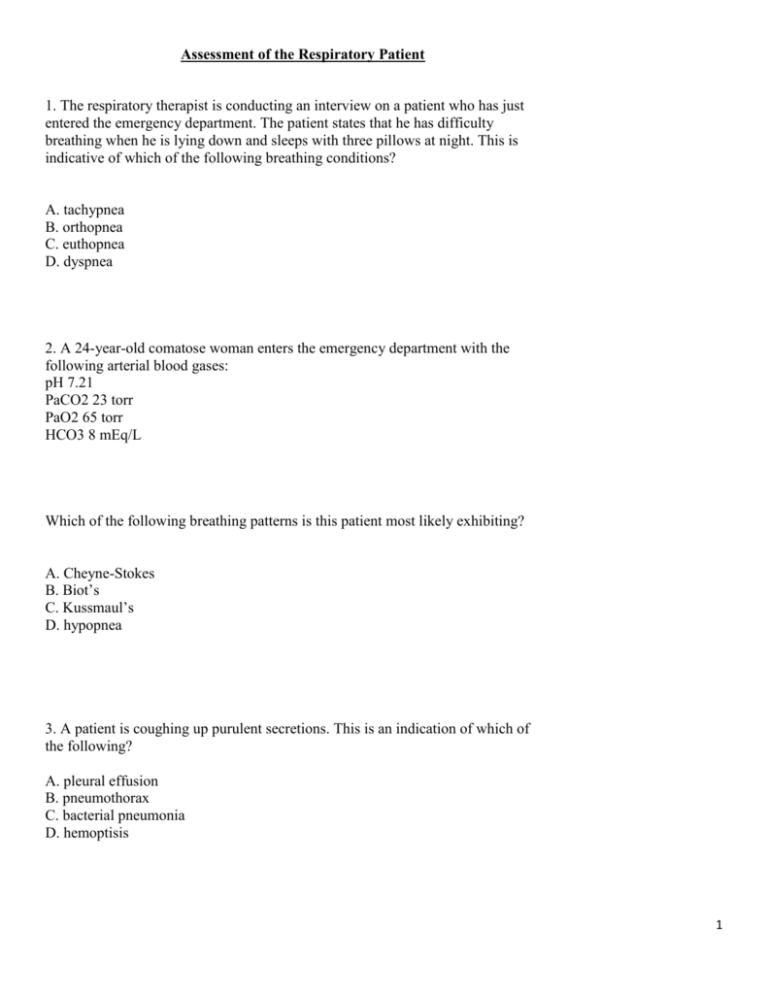
Assessment of the Respiratory Patient 1. The respiratory therapist is conducting an interview on a patient who has just entered the emergency department. The patient states that he has difficulty breathing when he is lying down and sleeps with three pillows at night. This is indicative of which of the following breathing conditions? A. tachypnea B. orthopnea C. euthopnea D. dyspnea 2. A 24-year-old comatose woman enters the emergency department with the following arterial blood gases: pH 7.21 PaCO2 23 torr PaO2 65 torr HCO3 8 mEq/L Which of the following breathing patterns is this patient most likely exhibiting? A. Cheyne-Stokes B. Biot’s C. Kussmaul’s D. hypopnea 3. A patient is coughing up purulent secretions. This is an indication of which of the following? A. pleural effusion B. pneumothorax C. bacterial pneumonia D. hemoptisis 1 4. A hyperresonant lung sound is heard while the respiratory therapist is percussing over the patient’s lower left lung field. This is indicative of which of the following pulmonary conditions? A. left lower lobe atelectasis B. left-sided pneumothorax C. pleural effusion D. lobar pneumonia 5. While auscultating the chest of a patient in ICU you hear crackles in both lung bases. This is most likely the result of which of the following? A. pulmonary edema B. tracheal stenosis C. bronchoconstriction D. glottic edema 6. A ventilator patient suddenly becomes restless and agitated and the high pressure alarm begins sounding. The respiratory therapist auscultates diminished breath sounds in the left lung and palpates the trachea right of midline. Which of the following has most likely occurred? A. right-sided pneumothorax B. massive atelectasis of the left lung C. ET tube slipped into right mainstem bronchus D. left-sided tension pneumothorax 7. A patient states that she has been coughing up thick, green, foul-smelling secretions. The respiratory care practitioner would conclude this patient has A. pulmonary edema. B. a Pseudomonas infection. C. hemoptysis. D. bronchial asthma. 2 8. A patient who seems unconscious but will awaken when stimulated is said to be A. lethargic. B. comatose. C. obtunded. D. disoriented. 9. The respiratory therapist is evaluating a patient and observes a six second capillary refill time. This indicates the patient A. has pulmonary edema. B. has inadequate perfusion to the extremities. C. has adequate pulmonary perfusion. D. has an increased cardiac output. 10. While conducting a pulmonary evaluation on a patient, the respiratory therapist auscultates diminished breath sounds on the right side and palpates the trachea being shifted toward the right side. The therapist should suspect which of the following? A. right-sided tension pneumothorax B. massive atelectasis of the right lung C. left-sided pneumothorax D. pleural effusion of the left lung 11. Which of the following muscles are utilized during normal breathing? I. scalenes II. diaphragm III. sternomastoid IV. external intercostals A. II only B. I and III only C. I and IV only D. II and IV only 3 12. A 38-year-old woman presents in ER complaining of shortness of breath. A CBC reveals a hemoglobin level of 6 gm%. The respiratory therapist determines her SpO2 is 99%. Which of the following statements are true regarding this patient’s condition? I. The patient is hypoxic. II. The patient is most likely cyanotic. III. Oxygen is not indicated at this time. A. I only B. III only C. I and II only D. I and III only 13. A patient in the cardiac care unit is hemodynamically unstable with fluctuating arterial blood pressures. Which of the following should the respiratory therapist recommend to best monitor this patient’s hemodynamic status? A. pulse oximeter B. radial artery catheter C. radial artery puncture for ABGs D. echocardiogram daily 14. The respiratory therapist is reviewing the chart of a patient in ICU who has a Swan-Ganz catheter in place. Which hemodynamic value would best determine the extent of the patient’s left heart failure? A. central venous pressure (CVP) B. pulmonary artery pressure (PAP) C. pulmonary capillary wedge pressure (PCWP) D. mean arterial pressure 15. To most effectively monitor the hemodynamic status of a patient with ARDS who is being mechanically ventilated, the respiratory therapist should recommend which of the following? A. Swan-Ganz catheter B. EKG monitor C. peripheral arterial line D. pulse oximeter 4 16. A 28-week-old neonate is suspected of having a pneumothorax. Which of the following should the respiratory therapist recommend to help diagnose if this condition is present? I. transillumination of the chest II. transcutaneous PO2 monitoring III. chest x-ray IV. arterial blood gases A. I and III only B. I, II and III only C. II, III and IV only D. I, III and IV only 17. While assessing a patient’s cardiac status, the respiratory therapist observes the following EKG tracing on the cardiac monitor. This would be interpreted as A. sinus bradycardia. B. ventricular fibrillation. C. sinus rhythm with occasional PVCs. D. sinus tachycardia. 18. The respiratory therapist is assessing a patient with emphysema and observes pedal edema and jugular venous distention. The therapist should note in the patient’s chart these signs are most likely the result of A. systemic hypertension. B. hypercapnia C. pulmonary infection D. right ventricular hypertrophy 19. The respiratory therapist is administering PEP therapy to a patient with atelectasis. Which of the following would indicate the atelectasis is improving? A. decreased late inspiratory crackles B. decreased inspiratory wheezes C. reduced inspiratory stridor D. coarse crackles that clear with coughing 5 20. The following arterial blood gas results are recorded for a COPD patient who is breathing spontaneously. It is not noted what FIO2 the patient is on. pH 7.23 PaCO2 82 torr PaO2 76 torr HCO3 36 mEq/L BE +12 The respiratory therapist should conclude from this information which of the following? A. The patient has acute respiratory acidemia and is breathing room air. B. The patient is not a chronic CO2 retainer. C. The patient is breathing supplemental oxygen. D. The blood gas sample is most likely venous blood. 21. A patient with ARDS is receiving mechanical ventilation with PEEP. The respiratory therapist has just increased the PEEP level from 8 cm H2O to 12 cm H2O. Which of the following should the therapist assess to determine the patient’s response to this change? I. blood pressure II. Dynamic lung compliance III. Heart rate IV. Fluid intake and output A. I and II only B. I, II and III only C. I, III and IV only D. I, II, III and IV 22. The respiratory therapist palpates a “thready” and irregular pulse on a patient with a history of atrial fibrillation. To further assess the patient’s condition, the therapist should recommend which of the following? A. chest radiograph B. ECG C. arterial blood gases D. pulse oximetry 6 23. A patient is experiencing cardiac arrhythmias, muscle weakness and an arterial blood gas determines the patient is in metabolic alkalosis. Which of the following is the most appropriate laboratory value to assess at this time? A. WBC B. Hb and Hct C. plasma protein D. potassium 24. A 2-year-old patient presents in the emergency department coughing with acute shortness of breath. A chest x-ray reveals a radiopaque density at the level of the 5th thoracic vertebrae in the right lung field. The right lung is also hyperinflated. Based on this information, the respiratory therapist should suspect this x-ray is most likely the result of which of the following? A. atelectasis of the right lower lobe B. a foreign body lodged in the right mainstem bronchus C. pneumothorax of the right lung D. right lower lobe pneumonia 25. The respiratory therapist has just intubated a patient in respiratory failure. To initially assess the position of the endotracheal tube, the therapist should recommend which of the following? A. measurement of PETCO2 B. arterial blood gas analysis C. measurement of spontaneous tidal volume D. measurement of SpO2 26. A severe COPD patient is admitted to the hospital with dyspnea. The patient is unresponsive with a blood pressure of 170/110 mm Hg and a respiratory rate of 38/min. The respiratory therapist should assess which of the following next? A. Hb and Hct B. PaCO2 C. SpO2 D. chest x-ray 7 27. The respiratory therapist is performing a chest examination on a mechanical ventilator patient and observes a dull percussion note over the right lower lobe with decreased expansion of the right lung. The therapist’s assessment may indicate the presence of A. a right mainstem intubation. B. a right-sided pneumothorax. C. a left-sided tension pneumothorax. D. atelectasis of the right lower lobe. 28. The respiratory therapist is assessing a patient who suffered smoke inhalation as the result of a house fire. The patient is on a nonrebreathing mask at 15 L/min and his ABG results are below. pH 7.23 PaCO2 21 torr PaO2 174 torr HCO3 12 mEq/L BE -13 SaO2 68% From this data, which of the following is true regarding this patient’s condition? I. The patient is hypoxic. II. The FIO2 should be decreased. III. The patient is hypoventilating. IV. The blood gases reveal a partially compensated metabolic acidemia. A. I and III only B. I and IV only C. II and III only D. I, III and IV only 29. The respiratory therapist is assessing a patient prior to initiation of bronchodilator therapy followed by CPT. The patient states “ I don’t feel short of breath, but I seem to breathe fast and I raise my shoulders with each breath. I sleep well at night using only one pillow.” The therapist can conclude from this interview that the patient most likely has A. orthopnea. B. dyspnea. C. increased work of breathing. D. bradypnea. 8 30. The respiratory therapist percusses an area of hyperresonance on a patient on mechanical ventilation. This percussion note is most likely the result of which of the following? A. pneumothorax B. atelectasis C. consolidation D. pulmonary edema 31. The respiratory therapist is conducting a bedside assessment on a patient with Guillain-Barre syndrome. Which of the following bedside pulmonary function results indicates the need for ventilatory assistance? A. maximum inspiratory pressure (MIP) of –28 cm H2O B. decreased peak expiratory flow C. vital capacity of 8 ml/kg of body weight D. decreased FEV1 32. The respiratory therapist is assessing a patient in the cardiac ICU. Over the past 36 hours, the patient has been complaining of increasing dyspnea. A chest x-ray reveals diffuse infiltrates. The therapist notes inspiratory crackles while auscultating the chest and observes jugular venous distension. Based on this assessment, which of the following values would most likely be increased? I. central venous pressure II. pulmonary capillary wedge pressure III. cardiac output A. I only B. III only C. I and II only D. I, II and III 33. A patient enters the emergency department following a motor vehicle accident. The respiratory therapist conducts a chest assessment and notes the trachea is shifted to the left of midline and breath sounds are absent on the right side. The patient’s respiratory rate is 38/min and has a SpO2 of 85%. The therapist should recommend which of the following at this time? A. Obtain a chest radiograph. B. Obtain stat ABGs. C. Intubate and initiate mechanical ventilation. D. Insert a chest tube on the right side. 9 34. The respiratory therapist is assessing a patient in the ICU with acute pulmonary edema. Which of the following would best determine if this is cardiogenic pulmonary edema? A. pulmonary capillary wedge pressure B. central venous pressure C. pulmonary artery pressure D. right atrial pressure 35. A physician has ordered hand-held nebulizer therapy q2h with 0.5 ml of albuterol (Ventolin). The patient has a history of congestive heart failure and currently has 3+ pitting edema. The patient has no history of asthma, smoking or pneumonia. There is moderate respiratory distress with expiratory wheezes. The respiratory therapist should recommend which of the following? I. furosemide (Lasix) II. intubation III. monitoring input/output IV. discontinuing the hand-held nebulizer treatment V. q4h nasal suctioning A. I, II, and III only B. I, III and IV only C. I, III, IV and V only D. II, III, and IV only 36. A patient is coughing up green, odorous secretions. This most likely indicates which type of organism present in the secretions? A. aerobic B. anaerobic C. viral D. acid-fast 37. The respiratory therapist palpates subcutaneous emphysema over the lower right lung segment. This is indicative of which of the following? A. right lower lobe pneumonia B. right pleural effusion C. right pneumothorax D. right lower lobe atelectasis 10 38. You observe digital clubbing while performing a pulmonary assessment on a patient. This is a sign the patient most likely has which of the following? A. asthma B. emphysema C. pneumonia D. atelectasis 39. While assessing a patient’s lab report you note the patient has a potassium level of 2.0 mEq/L. This patient is said to be A. hypokalemic. B. hypernatremic. C. hypoxemic. D. acidemic. 40. While assessing a patient’s chest radiograph you notice reduced vascular markings and a flattened diaphragm. This indicates the patient most likely has which of the following? A. pneumothorax B. pleural effusion C. pulmonary edema D. emphysema 41. Which of the following would be observed on a patient with cor pulmonale? I. pedal edema II. jugular venous distension III. decreased CVP level A. I only B. I and II only C. II and III only D. I, II and III 11 42. While assessing the lab work on a patient in the ICU you notice a white blood cell count of 6000. This indicates the patient has A. a normal WBC count B. an infection. C. a pleural effusion D. pneumonia. 43. While assessing the lab work on a patient in the ICU you notice a white blood cell count of 22,000. This indicates the patient has A. a decreased WBC count B. an infection. C. a pleural effusion D. atelectasis. 44. While assessing a patient’s chest radiograph you observe an area of hyperlucency. This may be the result of which of the following? I. hyperinflation II. atelectasis III. emphysema IV. pneumothorax A. I and III only B. II and III only C. I, III and IV only D. II, III and IV only 45. While performing a physical assessment on a patient in the ICU the respiratory therapist notes paradoxical respirations. This is indicative of which of the following conditions? A. emphysema B. pneumonia C. atelectasis D. flail chest 12 46. A patient experiencing deep, rapid breathing followed by apnea is exhibiting which type of breathing pattern? A. Kussmaul’s B. Biot’s C. bradypnea D. Cheyne-Stokes 47. Which of the following represents the normal value for potassium? A. 1.5 – 3.0 mEq/L B. 3.5 – 5.0 mEq/L C. 5.5 – 7.0 mEq/L D. 7.0 – 8.5 mEq/L 48. While assessing the patient’s chart you observe a hemoglobin level of 7.5 gm/dL. This indicates the patient A. has a decreased oxygen carrying capacity. B. has a normal hemoglobin level. C. has chronic lung disease. D. has a normal red blood cell count. 49. A patient has a respiratory rate of 12/min. This indicates the patient is A. tachypneic. B. eupneic. C. bradypneic. D. dyspneic. 50. Which of the following is true regarding a patient is experiencing Kussmaul’s respirations? A. The patient’s PaCO2 would be increased. B. The patient’s HCO3 would be increased. C. The patient’s pH would be decreased. D. The patient’s HCO3 would be normal. 13 Oxygen Therapy 1. A patient enters the emergency department complaining of shortness of breath with a respiratory rate of 30 breaths/min and a tidal volume that fluctuates between 300 ml and 450 ml. The physician orders the patient to be placed on a moderate level oxygen. Which of the following devices should the respiratory therapist recommend to deliver the oxygen? A. nasal cannula at 4 L/min B. 40% air entrainment mask C. simple oxygen mask at 8 L/min D. nonrebreathing mask at 15 L/min 2. The physician orders a 40% aerosol mask for a patient that has a total inspiratory flow of 42 L/min. In order to meet this patient’s inspiratory flow demands, what is the minimum flow the oxygen flowmeter must be set on? A. 8 L/min B. 10 L/min C. 12 L/min D. 14 L/min 3. While making oxygen rounds the respiratory therapist notices bubbling in a humidifier that is attached to an oxygen flowmeter that is turned completely off. The cause of this problem is most likely which of the following? A. There is a leak in the humidifier jar. B. The flowmeter is uncompensated for pressure. C. The flowmeter has a faulty valve seat. D. Water has entered the flowmeter. 4. The respiratory therapist is evaluating the oxygen set-up on a patient in the ICU. The patient is on a non-rebreathing mask with an O2 flow of 10 L/min. The therapist notices that the reservoir bag on a patient’s mask almost totally collapses during the patient’s inspiration. Which of the following should be done to correct this problem? A. Change to a partial rebreathing mask. B. Recommend placing the patient on a CPAP mask. C. Instruct the patient to breathe more shallow. D. Increase the flow to the mask. 14 5. Which of the following oxygen delivery devices are considered high-flow devices? I. venturi mask II. partial rebreathing mask III. simple oxygen mask IV. aerosol mask A. I only B. I and II only C. I and IV only D. II and III only 6. You are preparing to transport a patient on a 5 L/min nasal cannula from ICU to the Radiology Department for a CT scan. In order to ensure the E cylinder has enough gas to run for at least one hour, what is the minimum pressure the cylinder must contain? A. 900 psig B. 1200 psig C. 1400 psig D. 1700 psig 7. While making oxygen rounds the respiratory therapist notices that the bed sheet is pulled up over the entrainment port of a patient’s venturi mask. What effect will this have on the device? A. The delivered oxygen percentage will remain the same, but the total flow will decrease. B. Less air entrainment will occur resulting in a decrease in the delivered oxygen percentage. C. The delivered oxygen percentage will increase as the total flow decreases. D. The total flow from the device will increase with an increase in oxygen percentage. 8. A patient arrives in the emergency department after being pulled from a burning house. The respiratory therapist should recommend which of the following to best determine the severity of the patient’s smoke inhalation? A. Hb B. COHb C. PaO2 D. SpO2 15 9. The following data has been obtained from a 36-year-old patient in ICU with pneumonia on a 50% venturi mask. Arterial blood gases: pH 7.46 PaCO2 33 torr PaO2 54 torr HCO3 25 mEq/L respiratory rate - 26 breaths/min pulse - 110/min Based on this data, the respiratory therapist should recommend which of the following? A. Place on a 70% aerosol mask. B. Institute mechanical ventilation. C. Place on a 100% nonrebreathing mask. D. Place on CPAP. 10. The respiratory therapist is ask to set up 35% oxygen on an active 4-year-old patient. The most appropriate oxygen delivery device to use in this situation is which of the following? A. oxygen tent B. oxygen hood C. nasal cannula D. simple oxygen mask 11. The respiratory therapist notices that when a patient on a 40% aerosol masks inhales, there is no mist exiting the exhalation ports of the mask. Which of the following should be done to correct this problem? A. No action is necessary. This is a normal occurrence. B. Add a heater to the nebulizer. C. Increase the oxygen percentage to 50%. D. Increase the flowrate to the nebulizer. 12. A severe COPD patient enters the emergency department in respiratory distress. Arterial blood gases are drawn on room air. Thirty minutes later ABGs are drawn on 5 L/min nasal cannula. The data is recorded below. ABGs on room air: pH 7.34 ABGs on 5 L/min NC: pH 7.27 PaCO2 59 torr PaCO2 70 torr PaO2 42 torr PaO2 53 torr HCO3 36 mEq/L HCO3 36 mEq/L Which of the following should be recommended at this time? A. Decrease the oxygen to 2 L/min. B. Place on a nonrebreathing mask. C. Institute mechanical ventilation. D. Place on CPAP. 16 13. A patient on a 35% venturi mask running at 6 L/min is receiving how much total flow from the device? A. 24 L/min B. 30 L/min C. 36 L/min D. 42 L/min 14. The physician has ordered oxygen to be set up on a patient with a spontaneous tidal volume of 600 ml and an inspiratory time of one second. Which of the following oxygen delivery devices will deliver a flow that meets or exceeds this patient’s inspiratory flow? A. 35% air entrainment mask at 6 L/min B. 40% aerosol mask at 8 L/min C. nasal cannula at 5 L/min D. simple oxygen mask at 10 L/min 15. Room air WILL NOT be entrained through the exhalation ports of an aerosol mask during inspiration if A. inspiratory flow from the delivery device is inadequate. B. the patient’s inspiratory flow exceeds the total flow from the device. C. the patient’s inspiratory flow is 45 L/min and the total flow from the device is 40 L/min. D. the total flow from the device exceeds the patient’s inspiratory flow. 16. The following data is recorded on a patient who is on a 50% air entrainment mask. pH 7.38 PaCO2 43 torr PaO2 90 torr SaO2 95% Hb 14 vol% Heart rate - 76/min Respiratory rate - 14/min Based on this data, which of the following represents the patient’s total oxygen content? A. 12.3 vol% B. 15.6 vol% C. 18.1 vol% D. 20.3 vol% 17 17. A patient on a 100% nonrebreathing mask at 15 L/min has a PaO2 of 600 torr. Which of the following should the respiratory therapist recommend at this time? A. Place on a 40% air entrainment mask. B. Decrease the flow to 10 L/min. C. Place on a 4 L/min nasal cannula. D. Discontinue oxygen therapy. 18. A 32-year-old female patient with pneumonia has a PaO2 of 57 torr and a PaCO2 of 30 torr on a 50% air entrainment mask. Which of the following statements is FALSE regarding this situation? A. The patient has a decreased P(A-a)O2. B. The patient is hypocapnic. C. The patient’s arterial pH is most likely alkalotic. D. The patient is hyperventilating in response to hypoxemia. 19. The respiratory therapy practitioner is preparing to monitor a neonate’s TCPO2. With a barometric pressure of 747 torr, the monitor should be calibrated to room air at which of the following values? A. 0 torr B. 100 torr C. 147 torr D. 157 torr 20. The following data has been collected on a patient in ICU on a 60% aerosol mask. pH 7.44 PaCO2 42 torr PaO2 160 torr PB 747 torr Based on this information, which of the following represents this patient’s P(A-a)O2? A. 208 torr B. 276 torr C. 368 torr D. 404 torr 18 21. A patient is on a 60% aerosol mask with the flow running at 8 L/min. The patient is dyspneic with an SpO2 of 88%. Which of the following would be most appropriate at this time? A. Recommend administering a bronchodilator. B. Increase the O2 to 70%. C. Increase the flow to 15 L/min. D. Place the patient on CPAP of 4 cm H2O and 60% O2. 22. The maximum liter flow to be used to deliver oxygen to a patient on a nasal cannula is A. 4 L/min. B. 6 L/min. C. 8 L/min. D. 10 L/min. 23. Which one of the following oxygen delivery devices is not a low flow device? A. nasal cannula B. air entrainment mask C. partial rebreathing mask D. simple oxygen mask 24. When delivering oxygen using a simple oxygen mask, what is the minimum flow required? A. 3 L/min B. 5 L/min C. 7 L/min D. 10 L/min 25. Provided the patient has a normal respiratory rate and tidal volume, the oxygen percentage available with a simple oxygen mask is A. 22-35%. B. 30-40%. C. 35-55%. D. 55-70%. 19 26. When using an air entrainment mask with various jet sizes, the smaller the diameter of the jet A. the less room air entrainment. B. the more room air entrainment. C. the higher the delivered FIO2. D. the less total flow delivered. 27. The air/O2 entrainment ratio for 30% is which of the following? A. 25:1 B. 10:1 C. 8:1 D. 5:1 28. The respiratory therapist has received a verbal order from the physician to set up a high percentage of oxygen on a patient. Which device has the capability of delivering the highest oxygen percentage? A. simple oxygen mask B. air entrainment mask C. partial rebreathing mask D. nonrebreathing mask 29. Which of the following O2 delivery devices will meet the inspiratory flow demands of a patient with an inspiratory flow rate of 40 L/min? I. 40% aerosol mask at 8 L/min II. 30% air entrainment mask at 5 L/min III. 40% air entrainment mask at 12 L/min IV. 35% aerosol mask at 6 L/min A. I and III only B. II and III only C. III and IV only D. I, II and IV only 30. Assuming a patient has an ideal breathing pattern, what is the approximate oxygen percentage delivered with a nasal cannula at 4 liters/min? A. 28% B. 32% C. 36% D. 40% 20 31. The respiratory therapist has been asked to deliver a low percentage of oxygen to a patient that is breathing 30 times per minute with an irregular breathing pattern. Which device would be the best to set up on this patient? A. air entrainment mask at 28% B. nasal cannula at 2 L/min. C. nasal catheter at 2 L/min. D. simple oxygen mask at 6 L/min. 32. You have just completed setting up an oxygen cannula at 6 L/min. As you kink the cannula tubing you notice no sound coming from the humidifier. This could indicate which of the following? I. a leak around the humidifier top II. a cracked humidifier jar III. no leaks are present A. I only B. II only C. III only D. I and II only 33. You are asked to set up a moderate percent of oxygen on a patient who is breathing a consistent tidal volume of 450 milliliters at a respiratory rate that fluctuates between 20 and 30. Based on this information, the respiratory therapist should recommend setting up which oxygen delivery device? A. partial rebreathing mask B. nonrebreathing mask C. venturi mask D. nasal cannula 34. The oxygen percent on a nebulizer is decreased from 60% to 40%. After this oxygen change, which one of the following statements is true? A. Less room air will be entrained into the nebulizer. B. The aerosol density will increase. C. A higher total flow will be delivered to the patient. D. The liter flow must be decreased. 21 35. Which of the following statements are correct about venturi oxygen dilution systems? I. The FIO2 will decrease when the internal diameter of the jet is decreased. II. The FIO2 will increase when the size of the entrainment port is increased. III. The total flow will increase when the size of the entrainment port is increased. A. I only B. II only C. I and III only D. II and III only 36. While making oxygen rounds you discover that the 6-inch reservoir tubing on a T-piece (Briggs adaptor) set up has fallen off. What may result from this situation? I. The FIO2 could decrease. II. The total flow to the patient could increase. III. More room air entrainment could occur. A. I only B. II only C. I and III only D. II and III only 37. While preparing to analyze the oxygen percentage coming from a patient's aerosol mask, you notice water in the large bore aerosol tubing. What effect would this have on the operation of this aerosol set-up? A. decreased FIO2 B. increased FIO2 C. increased air entrainment into the nebulizer D. increased gas flow to the patient 38. After setting up a nonrebreathing mask on a patient, you remove a one way valve from one of the exhalation ports on the mask. This is done for what purpose? A. To increase the FIO2. B. To increase the humidity. C. To increase the flow to the reservoir bag. D. To allow air to enter the mask should oxygen flow become interrupted. 22 39. Which of the following are believed to be an advantage of the nasal cannula as compared with an air entrainment mask? I. The cannula needn't be removed while patient is eating. II. It may be safely used on patients with irregular breathing patterns. III. It is generally more comfortable for the patient. IV. It eliminates fluctuations in inspired oxygen concentrations. A. I and II only B. I and III only C. II and III only D. III and IV only 40. Choose the false statement regarding pulse-dose oxygen systems. A. This device can deliver oxygen to the patient on inspiration only. B. This device conserves oxygen by delivering a “pulse” of oxygen at higher flow rates than conventional flowmeters do. C. The device is attached to a 50 psi oxygen wall outlet or gas cylinder. D. This system may be used in conjunction with a reservoir cannula. 41. An order is written by the physician to put a patient on a 40% aerosol mask and he wants to meet the patient's inspiratory flow demand of 36 L/min. What would be the minimum flow rate to use to achieve this? A. 6 L/min B. 8 L/min C. 10 L/min D. 12 L/min 42. A patient with a broken nose and cheekbone who has thick pulmonary secretions is ordered to be placed on 40% oxygen. Based on this information which oxygen delivery device would be most indicated for this patient? A. nasal cannula at 5 L/min B. face tent C. simple mask at 8 L/min D. aerosol mask 23 43. Which piece of equipment is most commonly used for the set up of a tracheostomy collar? A. bubble humidifier B. impeller nebulizer C. ultrasonic nebulizer D. jet nebulizer 44. You notice after setting up a partial rebreathing mask on a patient that the reservoir bag totally collapses during inspiration. The respiratory therapist should recommend which of the following? A. Increase the flowrate. B. Place a one-way valve on the exhalation port.. C. Tighten the mask around the patient's face. D. Increase the flowrate. 45. The physician has ordered oxygen to be set up on a patient with a spontaneous tidal volume of 500 ml (0.5 L) and an inspiratory time of 1 second. Which of the following O2 devices will provide sufficient flow to meet this patient’s inspiratory flow demands. A. 35% air entrainment mask at 6 L/min B. 40% aerosol mask at 7 L/min C. simple oxygen mask at 10 L/min D. partial rebreathing mask at 15 L/min 46. A patient is placed on a 35% venturi mask at 8 L/min. What is the total flow being delivered to the patient? A. 36 L/min B. 42 L/min C. 48 L/min D. 54 L/min 47. The respiratory therapist is called to a patient’s room to check the oxygen setup. The flow to the patient’s mask is supplied by an air flowmeter running at 15 L/min and an O2 flowmeter running at 15 L/min. The delivered oxygen percentage from this device is A. 24% B. 35% C. 40% D. 60% 24 48. Which of the following are considered oxygen-conserving (reservoir) devices? I. partial rebreathing mask II. reservoir cannula III. pendant cannula IV. nasal cannula A. I and II only B. II and III only C. I, II and III only D. I, III and IV 49. A patient is set up on a 40% aerosol mask running at 10 L/min of oxygen. There is a 10 L/min air bleed in downstream. What percent oxygen is this set up delivering? A. 45% B. 40% C. 36% D. 30% 50. Inadequate alveolar ventilation caused by atelectasis resulting in hypoxia is an example of which type of hypoxia? A. anemic hypoxia B. stagnant hypoxia C. hypoxemic hypoxia D. histotoxic hypoxia 51. An example of histotoxic hypoxia would be A. carbon monoxide poisoning. B. upper airway obstruction. C. pulmonary embolism. D. alcohol poisoning. 25 52. Hypoxemic hypoxia may result from which of the following: I. hypoventilation II. ventilation/perfusion mismatch III. carbon monoxide poisoning A. I only B. II only C. I and II only D. II and III only 53. Cyanosis will be detected when A. the patient's PaO2 drops below 80 torr. B. there is 7 gm/dL of unsaturated hemoglobin. C. the patient's heart rate increases 20 beats/minute. D. the patient's SaO2 drops to 93%. 54. A patient on 50% oxygen has a PaO2 of 252 torr. Which of the following should the respiratory care practitioner recommend? A. Decrease the oxygen to 40%. B. Decrease the oxygen to 30%. C. Discontinue oxygen therapy. D. Repeat the blood gases as the PaO2 is not possible on this FIO2. 55. Which of the following statements is true regarding a patient who has a Hb level of 8 gm/dL and a SpO2 of 98%? A. The patient will not be cyanotic. B. Hypoxia is most likely not present. C. Oxygen is not indicated at this time. D. The patient is polycythemic. 56. Which statement about circulatory hypoxia is true? A. Tissue cells are unable to utilize oxygen due to an impairment of cellular oxidative enzymes. B. The O2 content and O2 carrying capacity are normal but blood flow through the capillaries is diminished. C. The hemoglobin levels in the blood are decreased. D. Tissue perfusion is adequate but the PaO2 is reduced. 26 57. Anemic hypoxia may be the result of A. carbon monoxide poisoning. B. right to left intrapulmonary shunting. C. pulmonary embolism. D. congestive heart failure. 58. Which one of the following is not an acute symptom of hypoxia? A. cyanosis B. dyspnea C. headache D. bradycardia 59. A patient has a PaO2 of 54 torr on a 40% aerosol mask. After the oxygen is increased to 60%, the PaO2 is 56 torr. This poor response to O2 therapy is most likely the result of which of the following? I. pulmonary edema II. hypoventilation III. atelectasis IV. diffusion defect A. I and III only B. III and IV only C. I, II and IV only D. II, III and IV only 60. Which of the following plays a role in the development of cor pulmonale in a severe COPD patient? I. pulmonary vasoconstriction II. increased red blood cell count III. anemic hypoxia A. I only B. II only C. III only D. I and II only 27 61. Which of the following is characteristically observed with cor pulmonale? A. right ventricular hypertrophy B. left ventricular hypertrophy C. atelectasis D. decreased hemoglobin levels 62. Given the following data, calculate total oxygen content. pH 7.41 PaCO2 43 torr PaO2 94 torr Hb 14 gm/dL SaO2 96% A. 13.4 vol.% B. 15.6 vol.% C. 17.8 vol.% D. 18.3 vol.% 63. A severe COPD patient is on a 28% air entrainment mask and has a PaO2 of 61 torr. Which of the following should the respiratory therapist recommend at this time? A. Place on CPAP. B. No changes are required at this time. C. Increase to O2 to 40%. D. Place on a nonrebreathing mask. 64. A patient is brought into the emergency department after being pulled from a burning house. The patient's ABG results on a nonrebreathing mask are pH 7.21, PaCO2 19 torr, PaO2 187 torr, HCO3 10 mEq/L, SaO2 65%. From this information, which of the following are true about this patient? I. The patient should be placed on a simple O2 mask at 10 L/min. II. The SpO2 should be measured due to the discrepency in the PaO2 and SaO2. III. The patient is hyperventilating due to severe hypoxia. IV. The blood gases reveal a partially compensated respiratory acidemia. A. III only B. I and IV only C. III and IV only D. II, III and IV only 28 65. In order to prevent neonatal retinopathy, the PaO2 should not exceed what level? A. 50 torr B. 60 torr C. 70 torr D. 80 torr 66. A physician orders a nonrebreathing mask on a severe chronic lung patient with a PaO2 of 59 torr. The patient seems to be in no acute distress. The respiratory therapist should do which of the following? A. Set up the mask as ordered. B. Ask the nurse for clarification. C. Notify the physician before setting up the mask and ask for clarification. D. Set up the mask and notify your supervisor at shift change. 67. Which of the following are not hazards of oxygen therapy? I. atelectasis II. respiratory depression III. pneumothorax IV. increased surfactant production A. I and II only B. III and IV only C. I, II and IV only D. II, III and IV only 68. A 28-year-old male presents with pneumonia and is placed on a 60% aerosol mask. His PaO2 is 51 torr and his PaCO2 is normal indicating he is ventilating adequately. The respiratory therapist should recommend which of the following? A. Place the patient on CPAP. B. Increase the aerosol mask to 70%. C. Place the patient on a nasal cannula at 2 L/min. D. Place the patient on a nonrebreathing mask. 29 69. A patient is brought into the emergency room having been pulled from a burning house. He is receiving oxygen through a nasal cannula at 4 l/min. Which of the following would you recommend at this time? A. Get a stat arterial blood gas. B. Remove the cannula and replace with a nonrebreathing mask. C. Increase the liter flow on the cannula to 6 l/min. D. Obtain an arterial blood gas on room air. 70. A patient presents in the emergency room after being rescued from a house fire. Which of the following devices would you recommend to most accurately determine the severity of the patient's carbon monoxide blood level? A. pulse oximeter B. co-oximeter C. oxygen analyzer D. capnometer 71. An alert, spontaneously breathing patient has a PaCO2 of 33 torr and a PaO2 of 55 torr while receiving an FIO2 of 0.70. Which of the following is the most appropriate way to increase the patient's PaO2? A. Increase the FIO2 only. B. Intubate and increase the FIO2. C. Apply CPAP at 60% oxygen. D. Apply CPAP at 100% oxygen. 72. CPAP is appropriate in the treatment of patients with which of the following? A. spontaneous breathing without hypoxemia B. spontaneous breathing with intrapulmonary shunting C. apnea D. a PaO2 of 90 torr on 25% oxygen 73. A patient has just been resuscitated following carbon monoxide poisoning. Which of the following values would best determine this patient's oxygen carrying capacity? A. SaO2 B. Hb level C. arterial oxygen content D. PaO2 30 74. The following blood gases have been obtained from a patient on a 40% airentrainment mask. pH 7.47 PaCO2 32 torr PaO2 58 torr Based on this data, the respiratory therapist should recommend to A. place the patient on CPAP. B. place the patient on a 60% aerosol mask. C. place the patient on a nonrebreathing mask. D. continue the current oxygen therapy and get a blood gas in one hour. 75. The following data has been collected on a patient. pH 7.42 PaCO2 42 torr PaO2 62 torr SaO2 91% Hb 13 gm/dL Based on this data, which of the following represents the amount of oxygen bound to hemoglobin? A. 0.23 vol% B. 10.8 vol% C C. 15.9 vol% D. 18.2 vol% 76. Which of the following is the most appropriate range to maintain a COPD patient’s PaO2 who is chronically hypercapnic? A. 45-55 torr B. 55-65 torr C. 65-75 torr D. 75-85 torr 77. Approximately how many hours will an H cylinder run at 5 L/min until empty if it contains a pressure of 1500 psi? A. 5 hours B. 10 hours C. 15 hours D. 20 hours 31 78. The respiratory care practitioner is setting up a portable liquid oxygen system for a chronic lung patient who attends church each week. The patient is on a 2 L/min nasal cannula and the portable oxygen container holds 4 lbs of oxygen. The practitioner should explain to the patient the oxygen supply will last for approximately what length of time? A. 4.5 hours B. 8 hours C. 11.5 hours D. 14 hours 79. Choose the FALSE statement(s) concerning the proper storage of medical gas cylinders. I. Cylinders shouldn't be stored in areas where the temperature exceeds 125oF. II. Flammable and non-flammable gases may be stored together. III. Cylinders must be stored with protective caps in place. IV. Full and empty cylinders should be segregated in the storage area. A. I only B. II only C. II and III only D. III and IV only 80. Which of the following represents the cylinder factor for a cylinder that has a filling pressure of 2000 psig and contains 50 cubic feet of gas? A. .28 L/psig B. .70 L/psig C. 1.41 L/psig D. 3.14 L/psig 81. A molecular sieve oxygen concentrator is capable to delivering a maximum oxygen percentage of which of the following? A. 40% B. 65% C. 95% D. 100% 82. Which statement about liquid oxygen storage is FALSE? A. It is stored at a higher pressure than gaseous oxygen. B. It is more economical and convenient than gaseous oxygen. C. The container in which it is stored is similar to a large thermos bottle keeping the temperature fairly constant. D. More oxygen may be stored in liquid form. 32 Humidity and Aerosol Therapy 1. Which of the following devices is capable of delivering gas to the patient that is fully saturated at body temperature? A. bubble humidifier B. heated Cascade humidifier C. passover humidifier D. heat moisture exchanger 2. While on rounds you notice that a bubble humidifier connected to a simple oxygen mask is not bubbling. Which of the following may be causing this problem? I. crack in the humidifier jar II. plugged capillary tube III. loose diffuser A. I only B. II only C. I and III only D. II and III only 3. After setting up a nasal cannula on 4 L/min, the respiratory therapist kinks the cannula tubing and a high-pitched whistling noise is heard coming from the humidifier. Which of the following is true regarding this situation? A. The liter flow is too high. B. The cannula tubing may have a crack in it. C. The oxygen setup is functioning properly. D. The humidifier should be replaced. 4. An immunocompromised patient is to be placed on oxygen with a humidity/aerosol device. Which of the following devices is most likely to deliver contaminated water to the patient? A. heated Cascade humidifier B. bubble humidifier C. heated wick humidifier D. heated jet nebulizer 33 5. While analyzing the oxygen on a patient that is set up on a heated 40% aerosol mask, you observe the analyzer reading 75%. Which of the following may be causing this high reading? A. There is water in the aerosol tubing. B. The liter flow to the nebulizer is too high. C. The air-entrainment port is opened more than it should be. D. The heater has malfunctioned. 6. A patient is on a ventilator with a heat moisture exchanger (HME) being used to humidify the inspired air. You notice that suctioning the patient has become more difficult due to the increase in the thickness of the secretions. Which of the following should the respiratory care practitioner recommend at this time? A. Replace the heat moisture exchanger with a heated humidifier. B. Increase the suction level. C. Use a larger suction catheter. D. Suction the patient more frequently. 7. A heated humidifier is delivering 100% body humidity to a patient’s airway. What volume of water is being delivered? A. 24 mg/L B. 37 mg/L C. 44 mg/L D. 47 mg/L 8. The respiratory therapist is instructing a patient on the proper use of a metered-dose inhaler. To deliver the optimal amount of medication, the patient should be instructed to activate the MDI A. after a deep inspiration. B. just before the patient begins to inhale. C. just after the patient has started to inhale. D. after a normal inspiration. 34 9. A patient in ICU with bronchiectasis has very thick, hard to mobilize pulmonary secretions. A bronchodilator has been ordered by the physician. Which of the following devices should the respiratory care practitioner recommend to deliver the medication? A. hand-held nebulizer B. metered-dose inhaler C. impeller nebulizer D. ultrasonic nebulizer 10. While making oxygen rounds, the respiratory care practitioner notices very little mist being produced by a nebulizer attached to an aerosol mask. Which of the following may be the cause of this? I. The liter flow is too low. II. The jet is obstructed. III. The capillary tube filter is clogged. A. I only B. I and II only C. II and III only D. I, II and III 11. Which of the following is not a hazard of aerosol therapy? A. overhydration B. bradycardia C. bronchospasm D. contaminated aerosol delivery 12. While administering an ultrasonic nebulizer treatment, the respiratory care practitioner notices that the couplant chamber light comes on. If this is not corrected, this may result in which of the following? A. The mist output will decrease. B. The temperature of the mist will increase. C. The electrical power will shut off. D. The vibration frequency will increase. 35 13. Absolute humidity is defined as A. the amount of moisture in a given volume of gas. B. the percent of water in the air at body temperature. C. the ratio of the amount of water in the air to the total amount that can be held at a given temperature. D. the amount of water the body's humidification process produces in the airway. 14. A patient is placed on an aerosol mask with a non-heated nebulizer that is delivering 18 mg of water/liter of gas. This patient has a humidity deficit of which of the following? A. 10 mg/L B. 16 mg/L C. 23 mg/L D. 26 mg/L 15. A volume of air at 22oC can hold 19 mg of water/liter of gas. What is the relative humidity of the air if it is holding 12 mg/liter at this temperature? A. 32% B. 48% C. 63% D. 74% 16. A patient's heated nebulizer is delivering 38 mg of water/liter of gas. What percent body humidity is being delivered with this device? A. 35% B. 54% C. 86% D. 93% 17. Tracheal secretions tend to dry in an intubated patient when the inspired air has which of the following characteristics? I. an absolute humidity of 22 milligrams of water/L of air II. a water vapor pressure of 47 mm Hg (torr) III. 52 milligrams of particulate water per liter of gas IV. a relative humidity of 100% at 25oC A. I and III only B. I and IV only C. II and III only D. III and IV only 36 18. In order to minimize an increased airway resistance produced by high density aerosol inhalation, the respiratory therapist should recommend which of the following? A. Administer a bronchodilator along with the aerosol. B. Instruct the patient to breathe through their nose. C. Use a heated nebulizer to deliver the aerosol.. D. Perform chest physiotherapy following the aerosol treatment. 19. Which of the following are considered indications for aerosol therapy? I. mobilization of retained secretions II. overhydration III. deliver a bronchodilator IV. following extubation to reduce swelling of the airway A. I and II only B. II and III only C. I and IV only D. I, III and IV only 20. A patient the respiratory therapist has just extubated complains his throat feels swollen and is sore when he swallows. Which of the following should the therapist recommend at this time? A. Deliver warm humidity to the patient’s airway. B. Deliver cool aerosol to the patient’s airway. C. Deliver warm aerosol to the patient’s airway. D. No therapy is recommended, but the patient should be told the symptoms should subside in a couple of days. 21. When an aerosol particle is termed hygroscopic, it means the particle A. is less than .1 microns in size. B. is influenced by gravity. C. is dry. D. retains moisture. 37 22. Which type of breathing pattern will improve aerosol delivery to a patient's lungs? A. fast rate and large volume B. slow rate, large volume and exhale through pursed lips C. fast paced inspiration with moderately deep volume and 3 second breath hold at end inspiration D. slow inspiration with moderately deep volume and a 2-3 second breath hold at end inspiration 23. Which of the following are not clinical uses of humidity? I. to humidify dry gases II. to provide 100% body humidity to intubated patients III. to deliver particulate water particles to the airway A. I only B. I and II only C. II and III only D. I, II and III 24. A gas mixture composed of three gases exerts a pressure of 747 mm Hg. The fractional concentrations of the gases are: Gas # 1 - 0.31 Gas # 2 - 0.52 Gas # 3 - 0.17 Correcting for water vapor pressure, what is the partial pressure of gas # 3? A. 104 mm Hg B. 119 mm Hg C. 217 mm Hg D. 364 mm Hg 25. The reason that a patient with thick retained secretions should have a heated nebulizer attached to the oxygen delivery device is to A. ensure that the patient doesn't become overhydrated. B. deliver more moisture to the airway thereby decreasing the thickness of the secretions. C. decrease the total water output in the inspired air. D. decrease the relative humidity in the inspired air. 38 26. The secretions of a tracheotomized patient are thick and difficult to mobilize. Which of the following should the respiratory therapist recommend? A. Add a heater to the nebulizer. B. Suction the patient every hour. C. Restrict fluid intake. D. Suction with a pressure of –140 mm Hg. 27. The respiratory therapist is asked to recommend a humidifier that will be able to provide the highest water vapor content to the patient’s airway. Which of the following humidifiers should the therapist select? A. passover B. heat moisture exchanger C. heated wick D. bubble 28. A patient receiving mechanical ventilation has a heat moisture exchanger attached at the circuit wye(Y). While making ventilator checks the respiratory therapist notes an increased dynamic lung compliance with no change in the static compliance. The therapist should recommend which of the following? A. Change to a heated wick humidifier. B. Suction the patient every hour. C. Initiate chest physiotherapy. D. Increase the patient’s tidal volume. 29. After administering a bland aerosol treatment to a patient, the respiratory therapist auscultates bilateral rhonchi. The therapist should recommend which of the following? A. Discontinue the treatment and initiate IPPB therapy. B. Encourage the patient to deep breath and cough. C. Initiate bronchodilator therapy. D. Discontinue the therapy. 30. The respiratory therapist is called to check the operation of a patient’s 35% aerosol mask. As you enter the room you notice the mist is being delivered intermittently, in short puffs of mist. The therapist should A. replace the nebulizer with a new one. B. drain the water from the aerosol tubing. C. increase the temperature to the nebulizer heater. D. increase the oxygen to 40%. 39 31. Which of the following would be able to provide the highest relative humidity to a patient on mechanical ventilation? A. HME B. bubble humidifier C. heated passover humidifier D. heated cascade humidifier 40 Equipment Troubleshooting and Decontamination 1. Which of the following methods is most commonly used to sterilize bacteria filters? A. autoclave B. ethylene oxide gas exposure C. pasteurization D. glutaraldehyde immersion 2. A patient is diagnosed with pulmonary tuberculosis. Which of the following isolation precautions should the respiratory care practitioner recommend? A. strict isolation B. reverse isolation C. respiratory isolation D. enteric isolation 3. Which of the following is the most cost-effective method for preventing cross contamination of a tracheostomy patient? A. Suction no more frequently than every four hours. B. Wash hands after each patient. C. Use sterile technique when suctioning. D. Change tracheosotomy dressing every eight hours. 4. Which of the following organisms is most frequently responsible for contamination of respiratory care equipment? A. Klebsiella B. Serratia C. E. coli D. Pseudomonas 5. The respiratory therapist is instructing a patient who is about to be discharged from the hospital the proper method for cleaning equipment in the home. Which of the following should be included in the procedure? A. The equipment should be towel dried immediately after it is removed from the liquid disinfectant. B. After rinsing the equipment in a vinegar solution for 30 minutes, it should be rinsed and allowed to air dry. C. The equipment should be disinfected after each use. D. An autoclave should be purchased to ensure adequate cleaning of the equipment 41 6. Which of the following cleaning methods or solutions does not have the capability of sterilizing equipment? I. autoclave II. pasteurization III. glutaraldehyde A. I only B. II only C. I and III only D. II and III only 7. Following a bronchoscopy, the respiratory care practitioner should clean the bronchoscope using which of the following cleaning methods? A. Wipe down with alcohol. B. Soak for thirty minutes in a glutaraldehyde solution. C. Place in an autoclave for fifteen minutes. D. Soak in acetic acid for one hour. 8. The respiratory therapist is calibrating a blood gas analyzer using a gas mixture containing 8% CO2 and 15% O2. The barometric pressure is 747 torr. The PCO2 should be set at which of the following values? A. 8 torr B. 24 torr C. 56 torr D. 60 torr 9. A patient is receiving cool mist entrained through a 30% venturi mask. The FIO2 measured at the mask is 35%. The respiratory therapist should do which of the following? A. Calibrate the analyzer and re-analyze the FIO2. B. Check the entrainment port setting. C. Check for condensation in the aerosol tubing. D. Check the flow to the venturi. 10. The respiratory therapist is calibrating a transcutaneous oxygen monitor to be set up on a two-day-old neonate. The barometric pressure is 747 torr. The PO2 should be set at which of the following values? A. 0 torr B. 21 torr C. 147 torr D. 157 torr 42 11. The respiratory therapist is having difficulty calibrating a transcutaneous oxygen electrode. Which is the most likely cause of this problem? A. The sensor is not attached to the patient properly. B. The membrane is damaged. C. The sensor is warm. D. Perfusion to the sensor site is poor. 12. While delivering IPPB to a tracheostomized patient air can be heard leaking around the patient’s mouth and the machine will not cycle off. The therapist should A. add air to the tube cuff. B. increase the flow. C. increase the sensitivity. D. decrease the inspiratory pressure. 13. The high pressure alarm is activated on a patient’s volume ventilator. Which of the following could be causing this problem? I. secretions in the airway II. bronchospasm III. leak around the chest tube IV. static compliance is increasing A. I and II only B. II and III only C. III and IV only D. I, II and IV only 14. The physician has ordered 35% oxygen via an oxygen hood and blender for a 5-day-old neonate. The flowmeter on the blender is reading 10 L/min and is attached to a nebulizer set on 40%. The blender is set at 35%. When analyzing the O2 concentration, the respiratory therapist observes the analyzer reading 25%. The therapist should do which of the following to correct this problem? A. Increase the flow to 12 L/min. B. Set the blender to 100% oxygen. C. Set the nebulizer’s entrainment port to 35%. D. Set the nebulizer’s entrainment port to 100%. 43 15.. The inverse I:E ratio alarm is sounding on a patient’s volume ventilator. Which of the following should the respiratory therapist recommend to correct this problem? A. Decrease the tidal volume. B. Increase the rate. C. Increase the flow. D. Set a 1 second inspiratory pause. 16. The respiratory therapist is analyzing the oxygen concentration from a heated 40% nebulizer running at 15 L/min. The analyzer reads 75%. The therapist should A. decrease the flow to 10 L/min. B. recalibrate the O2 analyzer. C. drain the condensation from the aerosol tubing. D. shorten the aerosol tubing. 17. While checking a volume ventilator that is to be set up on a postoperative cardiac bypass patient, the exhaled tidal volume display reads 300 ml less than the machine’s set tidal volume. The respiratory therapist should do which of the following to determine what is causing this problem? I. Measure the volume at the exhalation valve. II. Measure the volume leaving the ventilator outlet. III. Calculate the tubing compliance. A. I only B. I and II only C. II and III only D. I, II and III only 18. A patient is receiving volume-controlled ventilation. The respiratory therapist receives an order to increase the patient’s tidal volume from 600 to 800 ml. After changing the tidal volume, the therapist should adjust which of the following alarm settings? I. high minute volume alarm II. low exhaled tidal volume alarm III. high pressure alarm A. II only B. I and II only C. II and III only D. I, II, and III 44 19. While assessing a ventilator patient with a pneumothorax, the respiratory therapist observes a blood clot occluding the patient’s chest tube. The first action the therapist should take would be to A. clamp off the drainage tube. B. “milk” the drainage from the chest tube. C. insert a new chest tube. D.get a stat chest x-ray. 20. While transporting a patient on oxygen the cannula tubing becomes kinked between the mattress and bedrail. What affect will this have on the reading on the Bourdon gauge flowmeter attached to the e cylinder? A. The gauge will read lower. B. The gauge will read slightly higher. C. The gauge reading will remain the same. D. The gauge reading will increase at least 4 L/min. 21. An oxygen analyzer is reading inaccurately. To calibrate the analyzer which of the following gases should be used? I. oxygen II. room air III. nitrogen A. I only B. II only C. I and II D. II and III only 22. The mist exiting the aerosol mask attached to an ultrasonic nebulizer is minimal. Which of the following should be done to correct this problem? I. Drain the aerosol tubing. II. Decrease the amplitude. III. Add water to the couplant chamber. A. I only B. I and III only C. II an III only D. I, II and III 45 23. Which of the following could result in the high pressure alarm being triggered on a volume ventilator? I. patient experiencing bronchospasm II. patient disconnected from the ventilator III. increased lung compliance IV. decreased static pressure A. I only B. I and IV only C. II and III only D. III and IV only 24. The respiratory therapist notices very little mist exiting the reservoir tubing of a T-piece flow-by set-up as the patient inspires. The therapist should A. Increase the flow to the nebulizer. B. Instruct the patient to breathe deeper. C. Instruct the patient to breathe slower. D. Analyze the oxygen percentage. 25. The low volume alarm is triggered on a volume ventilator. Which of the following may be causing this problem? I. patient disconnection II. leak around chest tube III. excessive air in E-T tube cuff IV. inappropriate alarm setting A. I and II only B. II and IV only C. I, II and III only D. I, II and IV only 26. A patient receiving IPPB therapy has difficulty cycling the machine into exhalation. Which of the following should the respiratory therapist do first to correct this problem? A. Instruct the patient to breath deeper. B. Increase the inspiratory pressure. C. Instruct the patient to keep lips sealed tight around the mouthpiece. D. Give the treatment with a mask. 46 27. A patient with a suspected drug overdose is on a volume ventilator on the following settings. Tidal volume 650 ml Rate 12/min Mode Assist/control Inspiratory flow 25 L/min Pressure limit 45 cm H2O The I:E ratio alarm is triggered. Which ventilator adjustment should the respiratory therapist make at this time? A. Increase the pressure limit. B. Increase the tidal volume. C. Increase the inspiratory flow. D. Increase the rate. 28. A polarographic oxygen analyzer is being used to monitor the oxygen on a ventilator patient. The patient is on 100% oxygen and the analyzer is reading 102%. Which of the following should be done to correct this problem? A. Replace the membrane on the electrode. B. Calibrate the analyzer. C. Reduce the inspiratory flow on the ventilator. D. Change the batteries in the analyzer. 29. A patient is receiving 6 cm H2O of CPAP by mask at home but the CPAP level can’t be maintained. Which of the following should the respiratory therapist do? A. Reposition the patient’s head and neck. B. Make sure the tubing isn’t kinked. C. Suction the patient. D. Check for leaks in the set-up. 30. While administering IPPB to a patient the machine cycles without any effort on the patient’s part. Which of the following controls should the respiratory therapist check at this time? A. flow B. rate C. pressure D. oxygen 47 31. A patient is on a 70% T-piece with the oxygen flow to the nebulizer set at 15 L/min. The patient is dyspneic and no mist is visible exiting the T-piece reservoir. The respiratory therapist should do which of the following at this time? A. Add a second nebulizer. B. Increase the nebulizer setting to 100%. C. Shorten the aerosol tubing. D. Decrease the flow to the nebulizer. 32. Which of the following may result in inadequate mist output by a nebulizer? I. obstructed capillary tube II. inadequate flow III. water in the aerosol tubing A. I only B. I and II only C. II and III only D. I, II and III 33. The exhaled tidal volume display on a patient’s volume ventilator consistently reads lower than the set volume. Which of the following is the most likely cause? A. water in the tubing B. inadequate flow rate C. sensitivity control set too high D. leak around th HME 34. The high pressure alarm suddenly sounds on a patient receiving volumecycled ventilation. The most appropriate action to take is to A. decrease the inspiratory flow. B. increase the high pressure limit. C. suction the patient. D. Increase the inspiratory flow. 48 35. A patient receiving oxygen via concentrator at 2 L/min at home complains he can’t feel oxygen coming out the prongs of the cannula. Which of the following should the respiratory therapist do first? A. Place the cannula under water and see if bubbling occurs. B. Attach the cannula to a cylinder/flowmeter set-up. C. Increase the flow to 5 L/min. D. Replace the concentrator with a new one. 36. A demand-valve resuscitator is being used to ventilate an apneic patient in the emergency department. Inadequate tidal volumes are being delivered. The therapist should do which of the following first? A. Place the patient on a mechanical ventilator. B. Change to a manual resuscitator. C. Determine the resuscitator’s problem. D. Begin chest compressions. 37. While manually ventilating an intubated apneic patient with a manual resuscitator there is very little resistance when the bag is compressed and the patient’s chest rises only minimally. Which of the following may be the cause of this problem? A. Excessive E-T tube cuff pressure. B. Exhalation valve jammed in the closed position. C. The patient’s lungs are non-compliant. D. Inadequate E-T tube cuff pressure. 38. Which of the following is the most appropriate method to prevent the crosscontamination of a Wright respirometer that is being used on several patients? A. Place the respirometer is Cidex between patient use. B. Use a one-way valve so that only exhaled air flows through the respirometer. C. Have the respirometer autoclaved after each patient use. D. Wipe the respirometer with alochol after each patient use. 39. Which of the following is most likely responsible for a staphylcoccal outbreak in ICU patients requiring respiratory care? A. health care workers B. ventilators C. disposable humidifiers D. MDIs 49 40. Pulse oximeters are inaccurate in which of the following situations? I. carbon monoxide poisoning II. hypotension III. inadequate perfusion A. I only B. I and II only C. II and III only D. I, II and III 41. A respiratory care practitioner is called to a patient's room because oxygen is leaking from an E cylinder. The practitioner should do which of the following? I. Tighten all connections II. Replace the washer between the cylinder and regulator connections III. Knock the pins off the regulator to assure a tight fit IV. Lubricate around the connection where the leak is occurring. A. I and II only B. I and III only C. II and III only D. III and IV only 42. Hydrostatic testing of a gas cylinder will determine which of the following? I. cylinder expansion II. leaks in the cylinder III. cylinder wall stress A. II only B. I and III only C. II and III only D. I, II and III 43. The respiratory therapist is performing a routine home visit on a 58-year-old emphysema patient. The patient receives continuous oxygen with a nasal cannula at 2 L/min through an oxygen concentrator. The patient states that when traveling in his car, he uses an E cylinder secured in the back seat of his car and a spare cylinder in his trunk for especially long trips. The therapist should explain the proper method of cylinder transport and inform him that A. if he transports a cylinder in his trunk, he must make sure it is properly secured. B. he should leave the trunk open approximately 1 inch when transporting a spare cylinder. C. he should not transport cylinders in his car. D. he should not transport the spare cylinder in the trunk, but secure it in the back seat of the car. 50 44. The respiratory therapist is making a routine visit to the home of a 62-year-old patient who receives continuous oxygen through a nasal cannula at 2 L/min using an oxygen concentrator. The patient states she is going to start bowling each week and wants to know the best method of oxygen delivery while she bowls. The therapist should explain to the patient A. to use a portable liquid system. B. to use an E cylinder. C. to use the oxygen concentrator. D. she won’t be able to bowl while she is using oxygen. 45. It's important to "crack" a cylinder prior to the attachment of a regulator because A. the regulator won't function properly. B. it clears the valve outlet of dust and debris. C. it ensures the cylinder is full. D. it makes for an easier attachment 46. Which of the following statements regarding oxygen concentrators is FALSE? A. The concentrator is connected to an electrical wall outlet. B. When the flow is increased, the delivered oxygen percent increases. C. When using an oxygen enricher, it is recommended to triple the ordered O2 flow. D. Concentrators are primarily devices used to administer oxygen in the home setting. 47. Choose the FALSE statement regarding flow restrictors. A. They generally are used in delivery of oxygen in the home. B. They operate off a 50 psig gas source. C. The flow generally varies from 5-10 L/min. D. They are a fixed-orifice, constant-pressure flow metering device. 48. A Bourdon gauge regulator indirectly measures gas flow by directly measuring A. pressure B. liters per minute C. liters per second D. flow velocity 51 49. A flowmeter has a completely closed needle valve and the float jumps when the flowmeter is plugged into a wall gas outlet. Which of the following statements are true? I. This is a normal function in an uncompensated flowmeter. II. The flowmeter must have a restriction on it's outlet. III. This is a normal function in a compensated flowmeter. A. I only B. III only C. I and II only D. II and III only 50. You turn a flowmeter completely off in a patient's room following a treatment but hear gas leaking out of it. What is the most likely cause of this? A. The flowmeter is uncompensated. B. This is normal when using a compensated flowmeter. C. The flowmeter housing is cracked. D. The flowmeter has a faulty valve seat. 51. Reinserting a flowmeter into an oxygen wall outlet has failed to correct a massive gas leak in a patient's room. Which of the following should be done NEXT? A. Evacuate the patients from the floor. B. Provide necessary supplemental oxygen to patients in the area and close the zone valve. C. Have engineering shut off the hospital's master oxygen valve. D. Check the pressure relief valve on the patient's bubble humidifier. 52. The respiratory care practitioner needs to transport a patient on oxygen from ICU to the Radiology Department to have a CAT scan performed. In order to place an E cylinder in the bed in a horizontal position, which type of device should be used on the cylinder to measure the flow? A. uncompensated Thorpe tube flowmeter B. compensated Thorpe tube flowmeter C. Bourdon gauge flowmeter D. kinetic flowmeter 52 53. While making oxygen rounds the respiratory therapist discovers the reservoir tubing on a T-piece set-up has fallen off. Which of the following is true regarding this situation? A. The FIO2 may decrease. B. The total flow to the device will decrease. C. The FIO2 may increase. D. Less room air will be entrained. 54. After setting up a nonrebreathing mask the respiratory therapist removes one of the one-way valves covering the exhalation port. This is done to A. increase the FIO2. B. make sure the patient will get air should the oxygen flow be disrupted. C. increase the humidity output. D. increase the flow to the reservoir bag. 55. A polarographic oxygen analyzer is being used to analyze the oxygen on a nebulizer set on 40%. The analyzer reads 28%. Which of the following could be causing this inaccurate reading? I. weak batteries II. water on the membrane III. inappropriate nebulizer setting A. I only B. I and II only C. II and III only D. I, II and III 56 The respiratory care practitioner is making equipment rounds and hears the relief valve on a humidifier. Which of the following could be causing this problem? I. a loose tubing connection II. an excessive oxygen flow setting III. an obstruction in the attached tubing A. I only B. I and II only C. II and III only D. I, II, and III 53 57. The respiratory care practitioner opens the valve on an E cylinder that has a regulator attached and hears a loud hissing noise. The flowmeter is turned off. Which of the following actions might correct this problem? I. Tighten the regulator connection. II. Replace the regulator washer. III. Turn the flowmeter on. A. I only B. I and II only C. II and III only D. I, II, and III 58. A 20-month-old infant is to receive 35% oxygen by mist tent. While performing a routine equipment check, the respiratory therapist notices that the oxygen analyzer inside the tent reads 30%. After calibrating the analyzer, it still indicates 30%. The therapist should I. add sterile water to the nebulizer reservoir. II. check for leaks. III. check for water condensation in the aerosol tubing. A. II only B. I and II only C. II and III only D. I, II and III 59. A patient is receiving oxygen at home from a liquid oxygen reservoir at 1 L/min. He complains he does not feel gas coming out of the nasal cannula. Possible reasons for this complaint include which of the following? I. The electrical system has failed. II. The tubing is not connected properly. III. The system is delivering a relatively low flow. A. I only B. III only C. II and III only D. I, II and III 60. While checking an oxygen tent, the respiratory care practitioner is unable to detect any aerosol particles in the tent. The practitioner should do which of the following? A. Add a heater to the nebulizer. B. Decrease the flow from the nebulizer. C. Decrease the FIO2 setting on the nebulizer. D. Check the patency of the jet and capillary tube on the nebulizer. 54 61. While performing oxygen rounds you have difficulty obtaining an accurate reading with a polarographic oxygen analyzer. Which of the following would not help correct this problem? A. Changing the membrane. B. Drying the water off the membrane. C. Replacing the fuel cell. D. Adding electrolyte gel. 62. A patient is set up on a 40% aerosol mask which when analyzed reads 65%. What is the appropriate action to take? A. Increase the nebulizer flow. B. Decrease the nebulizer flow. C. Drain the water from the aerosol tubing. D. Shorten the length of the aerosol tubing. 55 Management of the Airway 1. The physician wants to begin weaning a patient from a tracheostomy tube. Which of the following should the respiratory therapist recommend? A. Change to a tracheostomy tube with a foam cuff. B. Change to a fenestrated tracheostomy tube. C. Change to a smaller tracheostomy tube. D. Change to a metal tracheosotomy tube. 2. The maximum amount of time a suction catheter should remain in the airway is A. 5 seconds. B. 10 seconds. C. 15 seconds. D. 20 seconds. 3. The respiratory therapist is using a 12 French suction catheter to suction a female patient who is intubated with a 7.0 mm E-T tube and is having difficulty removing the thick secretions. Which of the following should be recommended to correct this problem? A. Increase the suction pressure to -140 mm Hg. B. Instill 5 ml of normal saline down the E-T tube. C. Change to a 14 French suction catheter. D. Change to a coude-tipped suction catheter. 4. Immediately following extubation, the patient begins experiencing inspiratory stridor and difficulty breathing. The respiratory care practitioner should suspect which of the following? A. glottic edema B. tracheal stenosis C. vocal cord ulceration D. laryngeotracheal web 5. Immediately following intubation, which of the following should the respiratory therapist recommend first to determine proper tube placement? A. Order a stat chest x-ray. B. Palpate for symmetrical chest movement. C. Listen over the proximal end of the E-T tube for air movement. D. Auscultate the chest for equal breath sounds. 56 6. An oropharyngeal airway is indicated in which of the following situations? I. To prevent an unconscious patient from biting the E-T tube. II. To prevent upper airway obstruction in a conscious patient with neuromuscular disease. III. To prevent upper airway obstruction in a semicomatose patient with closedhead trauma. A. I only B. I and II only C. II and III only D. I, II and III 7. A patient has just been intubated and the CO2 detector placed on the proximal end of the E-T tube reads 1.5%. The respiratory care practitioner should suspect which of the following? A. The tube is in the trachea. B. The tube is in the right mainstem bronchus and should be withdrawn 4 cm. C. The tube is in the esophagus. D. The tube is at the level of the carina and should be withdrawn 2 cm. 8. An oral endotracheal tube is inserted into an adult patient. A leak is heard after 35 cm H2O is placed in the cuff. This would suggest which of the following? A. The E-T tube is too long. B. The E-T tube’s outside diameter is too small. C. The E-T tube’s inside diameter is too large. D. The E-T tube is too short. 9. A patient’s pulse drops from 86/min to 56/min when a suction catheter is inserted into the oral pharynx. The most likely cause is A. coughing. B. hypoxemia. C. hypocarbia. D. vagal stimulation. 57 10. The respiratory therapist is preparing to extubate a patient. The patient should be told the tube will be removed A. immediately following exhalation. B. after a strong cough effort. C. when the patient reaches the point of maximal inspiration. D. just as the patient begins to inhale. 11. While preparing to intubate a patient, the respiratory care practitioner attaches the laryngoscope blade to the handle and the light bulb fails to light. Which of the following should the practitioner do first? A. Tighten the light bulb. B. Replace the laryngoscope blade. C. Replace the batteries in the handle. D. Proceed to intubate without a light source. 12. Which of the following will increase the possibility of the E-T tube cuff causing tracheal mucosa damage? I. maintaining intracuff pressure of 28 mm Hg II. using minimal leak technique III. using a low volume, high pressure cuff IV. using minimal occluding volume technique A. I and III only B. II and IV only C. I, III and IV only D. II, III and IV 13. Which of the following is not an immediate complication of a tracheostomy tube? A. airway obstruction B. pneumothorax C. bleeding D. air embolism 14. The respiratory therapist has instilled air into a ventilator patient’s E-T tube cuff so that a slight leak is heard with a stethoscope at peak inspiration. The 58 peak pressure manometer on the ventilator reads 42 cm H2O at the time. Two hours later, the patient is suctioned and the peak inspiratory pressure drops to 25 cm H2O. Which of the following is now true regarding this situation? I. The leak around the cuff has increased. II. Minimal leak technique should be done at 25 cm H2O. III. The cuff pressure on the trachea wall has increased. A. I only B. II only C. I and II only D. II and III only 15. A frail, 76-year-old woman on a 2 L/min nasal cannula with retained secretions complains of pain and discomfort as the respiratory care practitioner performs percussion and postural drainage. The practitioner should recommend which of the following? A. Decrease the frequency of the treatment from QID to BID. B. Place the patient on BiPAP ventilation during the treatment. C. Increase the patient’s oxygen to 4 L/min during the treatment. D. Discontinue the therapy and begin intrapulmonary percussive ventilation. 16. A patient receiving positive expiratory pressure (PEP) therapy through a mouthpiece at 10 cm H2O has minimal secretion production. The respiratory therapist should recommend which of the following? A. Decrease the PEP to 5 cm H2O. B. Discontinue the treatment and begin percussion and postural drainage. C. Increase the PEP to 15 cm H2O. D. Administer the treatment with a mask in place of the mouthpiece. 17. Following suctioning of a ventilator patient’s ET tube, the following EKG tracing is observed on the cardiac monitor. NEED STRIP OF SINUS BRADYCARDIA The respiratory therapist should A. discontinue suction and increase the patient’s FIO2. B. recommend stat ABGs. C. continue suctioning but monitor the patient closely. D. recommend a stat chest x-ray. 59 18. A 34-year-old patient on a 40% aerosol mask has right lower lobe pneumonia. He becomes short of breath and his SpO2 drops from 96% to 89% when lying on his right side. What should the respiratory therapist recommend? A. Increase the O2 to 80%. B. Place the patient on his left side. C. Place the patient on CPAP. D. Suction the patient. 19. The respiratory therapist has instilled air into a ventilator patient’s ET tube cuff so that a slight leak is heard with a stethoscope at peak inspiration. The pressure manometer on the ventilator is reading 38 cm H2O at the time. Three hours later, the peak inspiratory pressure reading is 24 cm H2O. Which of the following is now true regarding this situation? I. Minimal leak technique should be done at 24 cm H2O. II. The leak around the cuff has increased. III. The cuff pressure on the trachea wall has increased. A. I only B. I and III only C. II and III only D. I, II and III 20. Following extubation, the patient develops inspiratory stridor and shortness of breath. The respiratory therapist should recommend which of the following? A. Reintubate the patient. B. Administer aerosolized racemic epinephrine. C. Begin IPPB with albuterol. D. Get a stat chest x-ray. 21. The respiratory therapist is using a 12 French suction catheter to suction a female patient who is intubated with a 6.5 mm ET tube and is having difficulty removing the thick secretions. Which of the following is the most appropriate action to take? A. Change to a coude-tip suction catheter. B. Increase the suction pressure to –150 mm Hg. C. Change to a 14 French suction catheter. D. Instill 4 ml of normal saline down the ET tube. 60 22. The respiratory therapist auscultates diminished breath sounds with little air movement on a patient presenting in the emergency department with acute asthma. After administering aerosolized albuterol, the therapist observes audible wheezing. Which of the following statements is true regarding this situation? A. The patient should be intubated immediately. B. The patient’s ventilatory status is improving. C. The patient most likely has developed glottic edema. D. The bronchodilator therapy is ineffective. 23. The following EKG rhythm is observed during the suctioning of a patient’s endotracheal tube. Strip shows sinus bradycardia Which of the following should the respiratory therapist do at this time? A. Decrease the suction pressure. B. Limit suction time to 20 seconds. C. Continue suctioning and monitor closely. D. Discontinue suctioning and hyperoxgenate the patient. 24. The respiratory therapist is called to pediatric ICU to suction an 8-year-old ventilator patient with pneumonia who is intubated with a 6.0 ET tube. Which of the following represents the most appropriate catheter size and suction pressure to use on this patient? A. 8 French catheter, -100 mm Hg B. 10 French catheter, -120 mm Hg C. 12 French catheter, - 80 mm Hg D.10 French catheter, -100 mm Hg 25. Which of the following increases the potential for damage to the tracheal mucosa by the endotracheal tube? I. Maintaining cuff pressure at 26 mm Hg. II. Use of a low volume, high pressure cuff. III. Maintaining cuff pressure at 27 cm H2O. A. I only B. I and II only C. II and III only D. I, II and III 61 26. Prior to nasally intubating an adult patient, which of the following should the respiratory therapist have available? I. suction catheter II. Magill forceps III. stylet IV. lubricating gel A. I and II only B. I, II and IV only C. II, III and IV D. I, II, III and IV 27. An intubated patient begins exhibiting severe respiratory distress and the respiratory therapist auscultates no breath sounds and determines there is no gas flow passing through the end of the ET tube. The high pressure alarm is sounding on the ventilator. Which of the following should the therapist do at this time? A. Instill 5 ml of saline down the ET tube and suction. B. Extubate and manually ventilate the patient. C. Obtain an arterial blood gas. D. Recommend a stat chest x-ray. 28. A patient on a volume ventilator is intubated with a 7.5 mm ET tube. The respiratory therapist has pre-oxygenated the patient and begins suctioning with a 12 Fr catheter and notes the patient is becoming bradycardic along with a drop in the SpO2. Which of the following should the therapist recommend at this time? A. Change to a closed-suction system. B. Instill Lidocaine down the ET tube. C. Change to a 14 Fr catheter. D. Increase the suction pressure to –140 mm Hg. 29. The respiratory therapist has received an order for postural drainage and percussion for a 34-year-old patient whose chest x-ray shows atelectasis of the posterior basal segment of the right lower lobe. The patient should be placed in which of the following positions to help drain this segment? A. lying on left side with bed flat B. prone, with head of bed down C. lying on left side with head of bed down D. supine, with head of bed down 62 30. The respiratory therapist is called to the emergency department to evaluate a patient suspected of a drug overdose. A Miller laryngoscope blade is selected to orally intubate the patient. When properly positioned, the blade will rest A. in the valeculla. B. 1 cm past the vocal cords. C. directly under the epiglottis. D. directly above the epiglottis. 31. The respiratory therapist is called to the ICU to change the tracheostomy tube of a ventilator patient due to a leak in the cuff. After replacing the tube and connecting it to the ventilator, the patient becomes cyanotic, tachycardic and the high pressure alarm begins sounding on the ventilator. The therapist notes subcutaneous emphysema around the upper chest and neck. Which of the following should the therapist do at this time? A. Increase the high pressure limit and increase the FiO2 to 1.0. B. Instill 5 ml of saline and suction the patient. C. Ensure there is adequate air in the cuff. D. Deflate the cuff, reposition the tube and attempt manual ventilation. 32. A 25-year-old patient with cystic fibrosis wants to continue his pulmonary hygiene program while working at his full-time job. Which of the following devices would be the most appropriate to recommend for this patient? A. MDI with bronchodilator B. ultrasonic nebulizer with bronchodilator C. intermittent percussive ventilation (IPV) D. Flutter mucous clearance device 33. Five minutes after extubating a patient, the respiratory therapist observes marked inspiratory stridor, intercostal retractions, labored breathing and a decreasing SpO2 value. Aerosolized racemic epinephrine has been administered with no affect. Which of the following should the therapist recommend at this time? A. an aerosol treatment with beclomethasone (Vanceril) B. a cool aerosol treatment C. manual ventilation with bag and mask D. reintubation 63 34. Which of the following represents the appropriate size suction catheter to use with a 6.0 mm endotracheal tube? A. 8 Fr B. 10 Fr C. 12 Fr D. 14 Fr 35. Which of the following is the most appropriate suction catheter size and suction pressure to use on an adult with an 8.0 mm ET tube. A. 10 Fr, -120 torr B. 14 Fr, -100 torr C. 12 Fr, -60 torr D. 14 Fr, -140 torr 64 IPPB Therapy/Incentive Spirometry 1. A patient is receiving IPPB therapy with a bronchodilator. At the start of the treatment the patient’s heart rate is 76/min and increases to 92/min after five minutes of the treatment. The respiratory therapist should do which of the following? A. Stop the treatment and notify the physician. B. Recommend decreasing the dose of the bronchodilator. C. Recommend changing the treatment to a hand-held nebulizer. D. Continue the treatment as ordered. 2. During IPPB, the patient complains the machine is having difficulty cycling into the expiratory phase. Which of the following may be causing this problem? I. The sensitivity is set too low. II. There is a leak around the patient’s mouthpiece. III. The exhalation valve is malfunctioning. A. I only B. I and II only C. II and III only D. I, II and III 3. While administering IPPB, the patient suddenly complains of chest pain and difficulty breathing. Upon further assessment of the patient, the respiratory care practitioner observes asymmetrical chest movement and tachycardia. The patient has most likely developed which of the following? A. pneumothorax B. pulmonary edema C. massive atelectasis D. pleural effusion 4. Incentive spirometry is most effective in which of the following conditions? A. treating preexisting atelectasis B. treating pneumonia C. preventing postoperative atelectasis D. emphysema 65 5. A patient is receiving IPPB therapy at a peak inspiratory pressure of 20 cm H2O. The patient begins having bronchospasms during the treatment. Which of the following is true regarding this situation? I. The peak inspiratory pressure will increase. II. The delivered tidal volume will decrease. III. The inspiratory time will increase. A. I only B. II only C. I and III only D. II and III 6. A patient complains during an IPPB treatment that he is having difficulty cycling the machine on. Which of the following should the respiratory care practitioner do to correct this problem? A. Decrease the machine sensitivity. B. Decrease the inspiratory pressure. C. Increase the machine sensitivity. D. Increase the inspiratory flow. 7. Five minutes into an IPPB treatment the patient begins coughing up a moderate amount of fresh blood. The respiratory care practitioner should do which of the following at this time? A. Decrease the inspiratory pressure. B. Stop the treatment and notify the physician. C. Stop the treatment for five minutes and continue if there are no other complications. D. Continue the treatment and have the nurse notify the physician. 8. While administering IPPB to a patient on air mix with the Bird Mark-7, the respiratory therapist adjusts the control so that 100% oxygen is now being delivered. Which of the following statements is true after this change is made? A. The inspiratory flow will decrease. B. The inspiratory pressure will increase. C. The inspiratory time will decrease. D. The sensitivity will increase. 66 9. While evaluating a postoperative patient for which incentive spirometry has been ordered, the respiratory therapist obtains a vital capacity of 6 ml/kg of body weight. The practitioner should do which of the following? A. Recommend IPPB in place of incentive spirometry. B. Start the treatment as ordered. C. Measure the patient’s tidal volume. D. Recommend a bronchodilator using a hand-held nebulizer. 10. While administering IPPB, the respiratory care practitioner increases the inspiratory flow. Which of the following would be true after this change is made? I. The inspiratory time will decrease. II. The tidal volume will decrease. III. The inspiratory pressure will increase. A. I only B. III only C. I and II only D. II and III only 11. During the administration of IPPB, the respiratory care practitioner notices the machine repeatedly cycles on shortly after the patient has begun expiration. In order to correct this problem, the practitioner should check which of the following controls? I. sensitivity control II. flow control III. inspiratory pressure control IV. rate control A. I only B. I and II only C. II and III only D. I and IV only 12. Which of the following is not a complication of IPPB? A. barotrauma B. increased cardiac output C. excessive ventilation D. gastric insufflation 67 13. The respiratory therapist is administering sustained maximal inspiratory maneuvers to a patient with postoperative atelectasis. The practitioner should expect all of the following results EXCEPT A. decreased functional residual capacity. B. increased lung compliance. C. reduced right-to-left shunting. D. improved distribution of ventilation. 14. Which of the following would be the most appropriate recommendation to help prevent postoperative atelectasis after a hypotensive patient’s abdominal surgery? A. IPPB B. incentive spirometry C. blow bottles D. CPAP 15. A severe COPD patient is on a 28% air entrainment mask. While taking IPPB on oxygen with air-mix in use, the patient’s respiratory rate decreases from 16/min at the start of the treatment, to 6/min five minutes into the treatment. Which of the following is the most appropriate recommendation at this time? A. Turn on the oxygen control to 100%. B. Place the patient on a nasal cannula at 2 L/min and administer the treatment on room air. C. Increase the inspiratory pressure. D. Increase the sensitivity level. 16. A patient is receiving IPPB therapy with a peak inspiratory pressure of 22 cm H2O following abdominal surgery. He has a vital capacity of 2.2 L. The respiratory therapist should recommend which of the following? A. Decrease the peak pressure to 18 cm H2O. B. Discontinue IPPB and begin deep breathing and coughing exercises. C. Continue IPPB as ordered. D. Obtain an arterial blood gas. 68 17. Which of the following would help reduce the potential of cardiac side effects caused by IPPB? I. Increase the flow. II. Increase the pressure. III. Increase the inspiratory time.. IV. Decrease the pressure. A. I and II only B. I and IV only C. II and III only D. III and IV only 18. While administering IPPB the patient begins experiencing bronchospasms. Which of the following will decrease as a result of this? A. inspiratory pressure B. FIO2 C. inspiratory time D. sensitivity 69 CPR/Manual Resuscitators 1. The respiratory care practitioner begins manually ventilating an apneic patient and the resuscitator bag malfunctions. Which of the following should the practitioner do first? A. Go find another resuscitator bag. B. Try to repair the bag. C. Perform mouth-to-mask ventilation. D. Call for a stat IPPB treatment. 2. While manually ventilating a patient with a manual resuscitator, arterial blood gas results show a PaO2 of 46 torr. Which of the following would increase the oxygen being delivered by the bag? I. Increase the ventilation rate. II. Add a reservoir to the bag. III. Increase the oxygen flow to the bag. A. II only B. I and II only C. II and III only D. I, II and III 3. You enter a patient’s room to administer an IPPB treatment and find the patient unconscious and apneic. After calling for help, which of the following should be done next? A. Administer two breaths. B. Check for a pulse and call for help. C. Place the patient in the fowler’s position. D. Open the patient’s airway. 4. Which of the following is the most appropriate method to open a patient’s airway who is suspected of having a neck fracture? A. jaw thrust maneuver B. head-tilt chin lift C. hyperextension of the neck D. place the patient in trendelenburg 70 5. The compression to ventilation ratio for single rescuer CPR on an infant is which of the following? A. 15:1 B. 5:2 C. 5:1 D. 15:2 6. While bagging a patient who has a tracheostomy tube, the respiratory care practitioner hears air leaking around the patient’s mouth and observes minimal chest excursion. Which of the following should the practitioner do at this time? A. Increase flow to the bag. B. Add more air to the tracheostomy tube cuff. C. Replace the resuscitator bag. D. Begin mouth-to-tube ventilation. 7. The respiratory care practitioner enters a patient’s room to administer an IPPB treatment and finds the patient unresponsive and not breathing. After two breaths are delivered, what should the practitioner do next? A. Begin chest compressions. B. Administer five abdominal thrusts. C. Administer IPPB for five minutes and assess for spontaneous breathing. D. Check for a pulse. 8. The respiratory care practitioner palpates no pulse on a patient but observes QRS complexes on the cardiac monitor. Which of the following should the practitioner do at this time? A. Obtain a 12-lead EKG . B. Begin cardiac compressions. C. Get a stat arterial blood gas. D. Recommend insertion of a Swan-Ganz catheter. 9. While ventilating a patient with a manual resuscitator, the respiratory care practitioner notices when the bag is squeezed, it collapses with little resistance and there is no chest movement. Which of the following could be causing this problem? A. excessive gas flow B. jammed exhalation valve C. reservoir attachment is loose D. leak around oxygen inlet valve 71 10. An infant in respiratory failure has just been delivered by a woman who states she has ingested a narcotic three hours ago. Which of the following medications should the respiratory care practitioner recommend for the infant at this time? A. epinephrine B. Narcan C. sodium bicarbonate D. Lidocaine 11. The respiratory therapist is performing bag-mask ventilation on a severe COPD patient during CPR. Which of the following describes the best method for ventilating this patient? A. The bag should be connected to an air wall outlet. B. The flow to the bag should be 10 L/min with no reservoir attachment. C. The bag should be connected to an O2 blender set at 30%. D. The bag should have a reservoir attachment and a flow of 15 L/min. 12. While participating in the resuscitation of a patient, the EKG monitor shows ventricular fibrillation after ten minutes of CPR. The arrhythmia does not reverse after the patient is defibrillated with 200 joules. The respiratory therapist should recommend which of the following at this time? A. Administer dopamine. B. Repeat defibrillation with 350 joules. C. Administer sodium nitroprusside. D. Implement cardioversion at 300 joules. 13. The physician is having difficulty placing an IV line in a patient with a pulse of 32/min. Which of the following medications should the respiratory therapist recommend instilling through the endotracheal tube? A. lidocaine (Xylocaine) B. sodium bicarbonate C. epinephrine D. atropine 72 14. A drug overdose patient who is unresponsive and intubated begins developing frequent PVCs. Attempts at placing peripheral or central catheters are unsuccessful. The respiratory therapist should recommend which of the following? A. endotracheal atropine B. endotracheal lidocaine (Xylocaine) C. defibrillation D. endotracheal epinephrine 15. The respiratory therapist is called to the emergency department to assess a 3-year-old male brought in after being pulled from the bottom of a swimming pool. He is unresponsive and pale with peripheral cyanosis. Vital signs are below: Heart rate 52/min Blood pressure 56/24 mm Hg Respiratory rate 10/min with intercostal retractions Temperature 33oC (91.4oF) Which of the following treatments are appropriate? I. endotracheal intubation II. heated aerosol mask at 100% O2 III. manual ventilation with 100% O2 IV. chest compressions A. I and III only B. II and IV only C. I and IV only D. I, III and IV only 16. The respiratory therapist assigned to NICU is called back to the delivery room to attend the delivery of a full term infant. The infant presents with the following vital signs after delivery: Heart rate 72/min Respiratory rate 22/min Color peripheral cyanosis The most appropriate treatment at this time should include which of the following? A. chest compressions and manual ventilation with 100% O2 B. endotracheal intubation C. oxyhood with 100% O2 D. administer Narcan 73 17. Sinus bradycardia is observed on the EKG monitor during the resuscitation of a 63-year-old female who was admitted to the emergency department following an episode of severe chest pain. The patient has no peripheral pulse and blood pressure cannot be measured. Which of the following should the respiratory therapist recommend? A. Defibrillate the patient with 200 joules. B. Cardiovert the patient. C. Administer atropine. D. Initiate chest compressions. 18. The respiratory therapist is asked to assist a physician performing cardioversion on a spontaneously breathing patient with atrial fibrillation. The patient is awake and alert. To prepare for this procedure, the therapist should do which of the following? I. Intubate the patient. II. Set up oxygen therapy equipment. III. Set up a manual resuscitator. IV. Assemble suction and airway care equipment. A. I and II only B. II and III only C. II, III and IV only D. I, II , III and IV 19. The respiratory therapist enters a patient’s room to administer IPPB and is unable to arouse the patient. The therapist should do which of the following first? A. open the patient’s airway B. call for help C. administer oxygen D. check for a pulse 20. The respiratory therapist enters a patient’s room to initiate incentive spirometry and finds the patient slumped over in bed and unresponsive to verbal and tactile stimuli. After calling for help, which of the following should the therapist do next? A. check for a pulse B. determine if the patient is breathing C. administer a precordial thump D. administer oxygen 74 21. An unconscious, apneic patient has just been intubated and the respiratory therapist begins ventilating with a manual resuscitator. Air can be heard leaking around the patient’s mouth and there is minimal chest during inspiration. The therapist should do which of the following? A. Check the ET tube cuff pressure. B. Make sure the reservoir is attached to the bag. C. Increase the flow to the bag. D. Suction the patient. 22. While providing ventilation with a manual resuscitator the reservoir attachment falls off the bag. This will result in which of the following? A. Decreased flow to the patient. B. Decreased ventilatory pressure. C. Decreased FIO2 delivery. D. A massive leak in the ventilating system. 23. Which of the following are complications of chest compressions? I. fractured ribs II. lacerated liver III. fat embolism A. I only B. I and II only C. II and III only D. I, II and III 24. A patient with a history atrial fibrillation which is normally controlled by medication enters the emergency department complaining of palpitations and shortness of breath. An EKG reveals atrial fibrillation. Which of the following is indicated? A. cardioversion with 200 joules B. defibrillation with 350 joules C. cardiovesion with 100 joules D. external pacemaker 75 25. A patient’s EKG monitor indicates ventricular fibrillation. Which of the following is most appropriate initial treatment? A. Cardioversion with 100 joules. B. Defibrillation with 350 joules. C. Defibrllation with 150 joules. D. Defibrillation with 200 joules. 76 Arterial Blood Gas Interpretation 1. A patient exhibiting Kussmaul’s breathing would have which of the following arterial blood gas results? A. pH 7.21, PaCO2 56 torr, PaO2 66 torr, HCO3 25 mEq/L B. pH 7.53, PaCO2 27 torr, PaO2 107 torr, HCO3 24 mEq/L C. pH 7.22, PaCO2 21 torr, PaO2 70 torr, HCO3 10 mEq/L D. pH 7.55, PaCO2 42 torr, PaO2 81 torr, HCO3 31 mEq/L 2. To best determine how well a patient is ventilating, the respiratory care practitioner should assess which of the following? A. pH B. SpO2 C. PaCO2 D. PaO2 3. Arterial blood gas values for a patient on a 40% venturi mask are below: pH 7.28 PaCO2 41 torr PaO2 88 torr HCO3 16 mEq/L These blood gases would be interpreted as which of the following? A. Uncompensated metabolic acidosis B. Compensated respiratory acidosis C. Partially compensated metabolic alkalosis D. uncompensated respiratory acidosis 4. Which of the following arterial blood gas results, drawn on room air, would you expect to observe on a 23-year-old asthmatic who has been in moderate respiratory distress for the past thirty minutes? A. pH 7.26, PaCO2 51 torr, PaO2 58 torr, HCO3 25 mEq/L B. pH 7.43, PaCO2 42 torr, PaO2 92 torr, HCO3 24 mEq/L C. pH 7.52, PaCO2 28 torr, PaO2 104 torr, HCO3 23 mEq/L D. pH 7.51, PaCO2 30 torr, PaO2 58 torr, HCO3 25 mEq/L 77 5. A patient on a volume ventilator has the following arterial blood gas results: pH 7.27 PaCO2 28 torr PaO2 88 torr HCO3 27 mEq/L Based on this data, the respiratory care practitioner should recommend which of the following? A. Increase the tidal volume. B. Decrease the ventilator rate. C. Get repeat blood gases since these results indicate a lab error. D. Decrease the FiO2. 6. A severe COPD patient arrives in the emergency department on a 2 L/min nasal cannula. Arterial blood gas results are below: pH 7.34 PaCO2 57 torr PaO2 46 torr HCO3 35 mEq/L Based on this data, the most appropriate recommendation is which of the following? A. Increase the liter flow to 3 L/min. B. Place the patient on CPAP mask of 4 cm H2O and an FiO2 of 0.60. C. Intubate and institute mechanical ventilation. D. Place on a nonrebreathing mask at 12 L/min. 7. A patient on a 35% venturi mask has the following arterial blood gas values: pH 7.45 PaCO2 27 torr PaO2 87 torr HCO3 16 mEq/L The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic alkalosis B. fully compensated respiratory alkalosis C. uncompensated respiratory alkalosis D. fully compensated metabolic alkalosis 78 8. The following blood gases are obtained on a severe, cyanotic COPD patient on a 2 L/min nasal cannula. pH 7.53 PaCO2 27 torr PaO2 160 torr HCO3 35 mEq/L Which of the following most likely accounts for these ABG values? A. The patient’s cannula flow was higher than 2 L/min at the time of the arterial stick. B. There is air in the blood sample. C. The blood was inadvertently obtained from a vein. D. These represent normal blood gases for a severe COPD patient. 9. A 32-year-old male patient on a 2 L/min nasal cannula in no apparent respiratory distress and no cyanosis present has arterial blood gases drawn. The results are below. pH 7.36 PaCO2 45 torr PaO2 43 torr Which of the following should the respiratory care practitioner recommend at this time? A. Repeat the arterial stick, as these most likely represent venous blood. B. Place the patient on a non-rebreathing mask. C. Increase the liter flow to 4 L/min. D. Place the patient on CPAP. 10. The following blood gases have been obtained from a ventilator patient in ICU. pH 7.26 PaCO2 51 torr PaO2 70 torr HCO3 15 mEq/L These ABGs would be interpreted as which of the following? A. partially compensated respiratory acidosis B. compensated metabolic acidosis C. combined metabolic and respiratory acidosis D. partially compensated metabolic acidosis 79 11. A patient on a 24% venturi mask has the following arterial blood gas values: pH 7.50 PaCO2 27 torr PaO2 87 torr HCO3 24 mEq/L BE +2 The correct interpretation of these ABGs is which of the following? A. uncompensated metabolic alkalosis B. partially compensated respiratory alkalosis C. uncompensated respiratory alkalosis D.partially compensated metabolic alkalosis 12. A patient on a 50% aerosol mask has the following arterial blood gas values: pH 7.26 PaCO2 54 torr PaO2 77 torr HCO3 16 mEq/L The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic alkalosis B. fully compensated respiratory acidosis C. uncompensated respiratory acidosis D. combined metabolic and respiratory acidosis 13. A COPD patient on a 30% venturi mask has the following arterial blood gas values: pH 7.37 PaCO2 58 torr PaO2 64 torr HCO3 36 mEq/L BE +12 The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic alkalosis B. fully compensated respiratory acidosis C. uncompensated respiratory acidosis D. partially compensated respiratory acidosis 80 14. A patient on a 40% venturi mask has the following arterial blood gas values: pH 7.49 PaCO2 27 torr PaO2 55 torr HCO3 25 mEq/L The respiratory therapist increases the oxygen percent to 50%. Which of the following blood gas values should increase after this change? I. pH II. PaCO2 III. PaO2 IV. HCO3 A. III only B. II and III only C. I, II and III only D. II, III and IV only 15. The following ABGs are observed on a 70 kg (154 lb) ventilator patient on a tidal volume of 800 ml. pH 7.19 PaCO2 27 torr PaO2 75 torr HCO3 15 mEq/L Which statement is true regarding this clinical scenario? A. The patient is hyperventilating. B. The blood gases reveal a respiratory alkalosis. C. The acidotic pH is a result of the decreased PaCO2. D. The patient’s ventilator tidal volume should be decreased. 16. Which of the following ABG results represents a partially compensated respiratory alkalosis? A. pH 7.37, PCO2 25 torr, HCO3 18 mEq/L, BE - 6 B. pH 7.52, PCO2 42 torr, HCO3 31 mEq/L, BE +6 C. pH 7.50, PCO2 28 torr, HCO3 25 mEq/L, BE 0 D. pH 7.51, PCO2 29 torr, HCO3 18 mEq/L, BE -5 81 17. Which of the following ABG results represents a partially compensated respiratory acidosis? A. pH 7.31, PCO2 55 torr, HCO3 18 mEq/L, BE -8 B. pH 7.29, PCO2 57 torr, HCO3 31 mEq/L, BE +6 C. pH 7.38, PCO2 60 torr, HCO3 35 mEq/L, BE +10 D. pH 7.31, PCO2 29 torr, HCO3 18 mEq/L, BE -5 18. Which of the following ABG results represents a partially compensated metabolic alkalosis? A. pH 7.49, PCO2 49 torr, HCO3 32 mEq/L, BE +5 B. pH 7.52, PCO2 40 torr, HCO3 33 mEq/L, BE +7 C. pH 7.50, PCO2 28 torr, HCO3 23 mEq/L, BE -2 D. pH 7.51, PCO2 29 torr, HCO3 19 mEq/L, BE -6 19. Which of the following ABG results represents an uncompensated respiratory alkalosis? A. pH 7.52, PCO2 48 torr, HCO3 34 mEq/L, BE +8 B. pH 7.50, PCO2 31 torr, HCO3 25 mEq/L, BE +1 C. pH 7.50, PCO2 28 torr, HCO3 32 mEq/L, BE +6 D. pH 7.51, PCO2 29 torr, HCO3 20 mEq/L, BE -5 20. Which of the following ABG results represents a fully compensated respiratory alkalosis? A. pH 7.35, PCO2 25 torr, HCO3 18 mEq/L, BE –10 B. pH 7.52, PCO2 40 torr, HCO3 33 mEq/L, BE +6 C. pH 7.50, PCO2 28 torr, HCO3 25 mEq/L, BE 0 D. pH 7.44, PCO2 29 torr, HCO3, 18 mEq/L, BE -5 21. Which of the following values would be increased with a patient in chronic respiratory acidemia? A. pH B. HCO3 C. SaO2 D. PaO2 82 22. A patient on a 40% aerosol mask has the following arterial blood gas values: pH 7.54 PaCO2 31 torr PaO2 77 torr HCO3 24 mEq/L The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic alkalosis B. fully compensated respiratory alkalosis C. uncompensated respiratory alkalosis D. combined metabolic and respiratory alkalosis 23. A patient receiving 25% oxygen with an air-entrainment mask has the following arterial blood gas values: pH 7.45 PaCO2 35 torr PaO2 96 torr HCO3 25 mEq/L BE 0 The correct interpretation of these ABGs is which of the following? A. fully compensated metabolic alkalosis B. fully compensated respiratory alkalosis C. uncompensated respiratory acidosis D. normal acid-base status 24. A patient on a 50% venturi mask has the following arterial blood gas values: pH 7.26 PaCO2 43 torr PaO2 81 torr HCO3 29 mEq/L The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic acidosis B. A lab error must exist. C. uncompensated respiratory acidosis D. combined metabolic and respiratory acidosis 83 25. Which of the following ABG values would most likely be decreased in a diabetic ketoacidosis patient? I. pH II. PCO2 III. HCO3 A. I only B. II only C. II and III only D. I, II and III 26. A patient’s PaCO2 is 43 torr with a pH of 7.51. Which of the following is true regarding these data? A. Bicarbonate must be increased. B. Hyperventilation is occurring. C. Base excess must be decreased. D. Respiratory alkalosis is present. 27. Which of the following ABG results represents a severe COPD patient in acute ventilatory failure? A. pH 7.25, PCO2 87 torr, PO2 62 torr, HCO3 32 mEq/L, BE +8 B. pH 7.35, PCO2 65 torr, PO2 64 torr, HCO3 33 mEq/L, BE +7 C. pH 7.41, PCO2 81 torr, PO2 70 torr, HCO3 38 mEq/L, BE +12 D. pH 7.37, PCO2 90 torr, PO2 67 torr, HCO3 39 mEq/L, BE + 14 28. A patient has a pH of 7.18 and a PaCO2 of 24 torr. Which of the following can be concluded regarding this blood gas data? A. Respiratory acidosis is present. B. The patient is hypoventilating. C. Metabolic acidosis is present. D. The base excess must be increased. 84 29. A patient receiving 35% oxygen with an air-entrainment mask has the following arterial blood gas values: pH 7.49 PaCO2 32 torr PaO2 96 torr HCO3 29 mEq/L BE +5 The correct interpretation of these ABGs is which of the following? A. partially compensated metabolic alkalosis B. combined metabolic and respiratory alkalosis C. uncompensated respiratory alkalosis D. A lab error must exist. 30. A patient receiving 28% oxygen with an air-entrainment mask has the following arterial blood gas values: pH 7.37 PaCO2 49 torr PaO2 75 torr HCO3 31 mEq/L BE +5 The correct interpretation of these ABGs is which of the following? A. fully compensated metabolic alkalosis B. combined metabolic and respiratory alkalosis C. fully compensated respiratory acidosis D. normal acid/base status 31. Which of the following represents a normal capillary PO2 on a 4-week-old neonate? A. 35 torr B. 45 torr C. 55 torr D. 65 torr 32. Which of the following represents the normal PaO2 on a 2-week-old neonate? A. 40 torr B. 60 torr C. 80 torr D. 100 torr 85 Ventilator Management 1. The following data is collected from a 75 kg (165 lb) patient on a volume ventilator. VT - 650 ml ABG results: pH 7.28 mode - assist/control PaCO2 53 torr ventilator rate - 12/min PaO2 68 torr FiO2 - 0.40 HCO3 25 mEq/L Based on these data, the most appropriate recommendation is which of the following? A. Increase the FiO2 to 0.60. B. Add PEEP at 4 cm H2O. C. Increase VT to 750 ml. D. Add 50 ml of deadspace. 2. Optimal PEEP is indicated by which of the following data? Peak Inspiratory Plateau Tidal PEEP Pressure Pressure Volume (cm H2O) (cm H2O (cm H2O) (ml) ________ ______________ ________ _______ A. 5 37 22 500 B. 8 41 26 500 C. 11 45 27 500 D. 14 48 31 500 3. The following data is collected from a 75 kg (165 lb) patient on a 40% aerosol mask. VT - 500 ml respiratory rate - 12 This patient’s alveolar minute ventilation is which of the following? A. 4.0 L B. 5.0 L C. 6.0 L D. 7.0 L 86 4. The following arterial blood gases have been collected from a 42 year-old patient on a 60% aerosol mask with a diagnosis of lobar pneumonia. pH 7.45 PaCO2 34 torr PaO2 57 torr HCO3 25 mEq/L The most appropriate recommendation is which of the following? A. Intubate and place on mechanical ventilation. B. Increase oxygen to 70%. C. Place on CPAP mask of 4 cm H2O and 60% oxygen. D. Place on nonrebreathing mask. 5. A 65 kg (143 lb) female patient arrives in the emergency department intubated and being manually ventilated with 100% oxygen. The respiratory therapist should select which of the following ventilator settings to best ventilate this patient? A. mode - assist/control, VT - 700 ml, rate - 12 B. mode - control, VT - 600 ml, rate - 12 C. mode - SIMV, VT - 700 ml, rate - 6 D. mode - SIMV, VT - 650 ml, rate - 14 6. The following data has been collected from a patient on a volume ventilator. VT - 750 ml ABG results: pH 7.41 mode - SIMV PaCO2 42 torr ventilator rate - 12/min PaO2 157 torr FiO2 - 0.80 HCO3 24 mEq/L PEEP - 10 cm H2O Based on this data, the most appropriate recommendation is which of the following? A. Decrease PEEP to 8 cm H2O. B. Decrease SIMV rate to 6/min. C. Decrease VT to 650 ml. D. Decrease FiO2 to 0.70. 87 7. Which of the following is the most important alarm in a CPAP system? A. high respiratory rate B. low pressure C. high FiO2 D. I:E ratio 8. The I:E ratio alarm is activated on the Bennett 7200 ventilator. The most appropriate action to correct this situation is which of the following? A. Increase the high pressure limit. B. Increase the flow. C. Decrease the tidal volume. D. Decrease the flow. 9. Which of the following ventilation parameters indicate a ventilator patient is most likely ready to be weaned from the ventilator? I. MIP of -28 cm H2O II. VC of 8 ml/kg III. A-a gradient of 170 torr on 100% oxygen A. I only B. I and III only C. II and III only D. I, II and III 10. The following data has been obtained from a patient on a volume ventilator and a tidal volume of 800 ml. Time 1 PM 2 PM 3 PM peakpressure (cm H2O) 38 42 46 plateau pressure (cm H2O) 18 23 26 Which of the following statements regarding these data are true? A. Lung compliance is decreasing. B. Airway resistance is decreasing. C. The lungs are becoming easier to ventilate. D. Lung compliance is increasing. 88 11. A patient on a volume ventilator is on the following settings: SIMV mode ABG results: pH 7.29 VT - 700 ml PaCO2 50 torr ventilator rate - 4/min PaO2 72 torr FiO2 - 0.30 Based on this data, which of the following is the most appropriate recommendation at this time? A. Increase VT to 800 ml. B. Increase FiO2 to 0.40. C. Change to assist/control mode, rate of 12. D. Increase SIMV rate to 6/min. 12. A patient on a volume ventilator has a PaO2 of 56 torr on a PEEP of 8 cm H2O and an FiO2 of 0.50. After increasing the PEEP to 12 cm H2O, the cardiac output decreases from 5.1 L/min to 4.1 L/min. The most appropriate recommendation is to A. discontinue PEEP and increase the FiO2 to 0.70. B. increase PEEP to 15 cm H2O. C. decrease PEEP to 8 cm H2O and increase the FiO2 to 0.60. D. maintain the current settings and measure cardiac output in one hour. 13. A premature infant on a pressure ventilator has a PaCO2 of 54 torr. Which of the following ventilator settings should be increased to correct this situation? A. FiO2 B. tidal volume C. PEEP D. inspiratory pressure 14. The respiratory care practitioner is called to a ventilator patient’s room and finds the high pressure alarm sounding. Which of the following could the practitioner do to help correct this problem? I. Suction the patient. II. Drain water from the tubing. III. Check high pressure limit for appropriateness of set level. A. I and II only B. I and III only C. II and III only D. I, II and III 89 15. A 42-year-old postoperative patient is on the following ventilator settings. Mode – SIMV Ventilator rate – 6/min Tidal volume – 700 ml FIO2 – 0.35 Peak flow – 50 L/min Pressure support – 25 cm H2O During weaning trials using a T-piece, the patient becomes tachypneic, agitated and short of breath, and must be placed back on the ventilator. Based on this information, the respiratory therapist should recommend which of the following to wean this patient? A. Increase the peak flow. B. Increase the FIO2. C. Decrease the pressure support. D. Decrease the tidal volume. 16. A patient on a volume ventilator is set on a tidal volume of 800 ml but the exhaled volume display is reading 500 ml. The respiratory care practitioner wants to determine the volume that the ventilator is actually delivering. To most accurately measure this volume, the practitioner should place a respirometer A. at the exhalation valve. B. at the patient wye connector. C. at the ventilator outlet. D. at the humidifier outlet. 17. After PEEP is initiated on a patient, the respiratory therapist should expect which of the following to occur? I. increased FRC II. increased plateau pressure III. increased lung compliance IV.decreased A-a gradient A. I and II only B. III and IV only C. I, III and IV only D. I, II, III and IV only 90 18. A premature infant is ventilated with a pressure ventilator in the NICU. The infant’s lung compliance begins to decrease. Which of the following statements is true regarding this situation? A. Peak inspiratory pressure will increase. B. The delivered tidal volume will decrease. C. The infant’s lungs will be easier to ventilate. D. The infant’s PaCO2 should begin to decrease. 19. Venous return is least impaired by which of the following ventilator settings? A. SIMV mode, rate 12/min B. Control mode, rate 10/min C. Assist/control mode, rate 10/min D. SIMV mode, rate 8/min 20. The following data is collected from a 4-day-old neonate on a pressure ventilator in the NICU. IMV mode Rate - 30/min Inspiratory pressure - 26 cm H2O FIO2 - 0.50 PEEP - 4 cm H2O pH 7.29 PaCO2 53 torr PaO2 51 torr Which of the following should the respiratory care practitioner recommend to increase? A. FIO2 B. PEEP C. inspiratory pressure D. inspiratory flow 21. A patient is in the control mode on a volume ventilator. Which of the following should be increased in order to most effectively increase alveolar ventilation? A. FIO2 B. ventilator rate C. tidal volume D. inspiratory flow 91 22. The following data is collected on a 75 kg (165 lb) patient being ventilated in the pressure-control mode. Peak inspiratory pressure - 22 cm H2O PEEP - 5 cm H2O Rate - 12/min FIO2 - 0.50 Exhaled tidal volume - 500 ml ABG results: pH 7.27 PaCO2 54 torr PaO2 68 torr HCO3 24 mEq/L The respiratory therapist should recommend which of the following? A. Increase the PIP to 26 cm H2O. B. Increase the FIO2 to 0.70. C. Increase PEEP to 10 cm H2O. D. Increase rate to 15/min. 23. A 70 kg ( 154 lb) patient in ICU is being mechanically ventilated on a volume ventilator in the assist-control mode, rate of 12/min, tidal volume of 750 ml and 40% oxygen. Arterial blood gases are below. pH 7.50 PaCO2 31 torr PaO2 54 torr HCO3 25 mEq/l Which of the following ventilator changes is most appropriate at this time? A. Increase the oxygen to 50%. B. Decrease the tidal volume to 700 ml. C. Place the patient on 4 cm H2O PEEP. D. Increase the ventilator rate to 15/min. 92 24. The following data is collected from a 65 kg (143 lb) patient with a closedhead injury and elevated intracranial pressure levels receiving volume-cycled ventilation. Mode - SIMV Mandatory rate - 10/min Total rate - 10/min Tidal volume - 650 ml FIO2 - 0.50 pH 7.36 PaCO2 44 torr PaO2 110 torr HCO3 25 mEq/L Which of the following is the most appropriate ventilator change at this time? A. Decrease the FIO2 to 0.40. B. Increase the rate to 15/min. C. Decrease the inspiratory flow. D. Decrease the tidal volume to 600 ml. 25. The following arterial blood gas results are obtained from a patient on volume ventilation in the SIMV mode. pH 7.56 PaCO2 27 torr PaO2 128 torr HCO3 23 mEq/L Which of the following ventilator changes should the respiratory therapist make first? A. Decrease the FIO2. B. Decrease the inspiratory flow. C. Increase the pressure support. D. Decrease the tidal volume. 93 26. A 54-year-old patient with pneumonia is being mechanically ventilated in the pressure-control mode. Over the past several hours, his exhaled tidal volume has increased from 350 ml to 550 ml. Other data is recorded below. Peak inspiratory pressure - 28 cm H2O Rate - 12/min FIO2 - 0.50 PEEP - 6 cm H2O ABG results: pH 7.50 PaCO2 27 torr PaO2 96 torr HCO3 23 mEq/L Based on this data, the respiratory therapist should recommend which of the following? A. Decrease the FIO2 to 0.40. B. Decrease PIP to 24 cm H2O. C. Increase the inspiratory flow. D. Decrease PEEP to 4 cm H2O. 27. A patient with ARDS is being mechanically ventilated on 80% oxygen. The PEEP level is increased from 8 cm H2O to 12 cm H2O resulting in the PaO2 increasing from 52 torr to 91 torr and a drop in the cardiac output from 4.6 L/min to 3.2 L/min. Which of the following is the most appropriate recommendation? A. Maintain PEEP at 12 cm H2O. B. Decrease PEEP to 8 cm H2O. C. Decrease PEEP to 10 cm H2O. D. Maintain PEEP at 12 cm H2O and decrease FIO2 to 0.70. 28. A patient is on a 750 ml tidal volume and a mandatory respiratory rate of 12/min in the control mode on a volume ventilator. An arterial blood gas reveals a PaCO2 of 31 torr. The respiratory therapist is asked to adjust the minute volume to maintain a PaCO2 of 40 torr. Which of the following ventilator settings should the therapist use to achieve the desired PaCO2? A. tidal volume - 750 ml, rate - 8/min B. tidal volume - 700 ml, rate - 10/min C. tidal volume - 650 ml. rate - 12/min D. tidal volume - 600 ml, rate - 16/min 94 29. A 34-year-old patient in the ICU is receiving noninvasive positive pressure ventilation by mask. The settings and ABG results are below. Inspiratory positive airway pressure (IPAP) 14 cm H2O Expiratory positive airway pressure (EPAP) 5 cm H2O Respiratory rate 12/min pH 7.29 PaCO2 51 torr PaO2 63 torr HCO3 23 mEq/L BE -1 Which of the following should be recommended to improve the patient’s ventilatory status? A. Increase the EPAP to 10 cm H2O. B. Decrease the IPAP to 12 cm H2O. C. Decrease the EPAP to 3 cm H2O. D. Increase the IPAP to 18 cm H2O. 30. A 26-year-old male patient is brought to the recovery room following abdominal surgery. The patient is intubated and has normal pulmonary function. The patient is 5’5” and weighs 150 kg (330 lb). Which of the following ventilator settings should the respiratory therapist recommend? A. rate - 10/min, tidal volume - 500 ml B. rate - 12/min, tidal volume - 700 ml C. rate - 12/min, tidal volume - 950 ml D. rate - 8/min, tidal volume - 1500 ml 31. A patient receiving mechanical ventilation is placed on a PEEP of 6 cm H2O. Which of the following will most likely decrease? I. FRC II. P(A-a)O2 III. static lung compliance A. I only B. II only C. I and III only D. I, II and III 95 32. The data below have been collected from a 70 kg (154 lb) male patient on a volume ventilator. Mode – A/C ABGs: pH 7.27 Ventilator rate – 12/min PaCO2 52 torr Tidal volume – 600 ml PaO2 62 torr FIO2 – 0.40 HCO3 25 mEq/L BE +1 Based on these data, the most appropriate ventilator change is which of the following? A. Increase tidal volume to 700 ml. B. Increase FIO2 to 0.50. C. Initiate PEEP at 5 cm H2O. D. Add 50 ml of mechanical deadspace. 33. Which of the following would most likely indicate that a ventilator patient is ready to be weaned. I. MIP of –25 cm H2O II. VC of 8 ml/kg III. P(A-a)O2 of 275 torr on 100% oxygen IV. VD/VT of 0.65 A. I only B. I and III only C. I, III and IV only D. II, III and IV only 34. A 36-year-old, 75 kg (165 lb) man is receiving mechanical ventilation on the settings below. Mode – A/C Ventilator rate – 10/min Tidal volume – 850 ml FIO2 – 0.35 Flow – 20 L/min Pressure limit – 40 cm H2O The pressure limit alarms with each breath and wide fluctuations are observed on the pressure manometer. The most appropriate action to take at this time would be to A. increase the ventilator rate to 15/min. B. increase the pressure limit to 50 cm H2O. C. decrease the tidal volume to 750 ml. D. increase the flow to 40 L/min. 96 35. The following data are collected from a 75 kg (165 lb) female patient with ARDS on a volume ventilator. Mode – SIMV Ventilator rate – 12/min Tidal volume – 700 ml FIO2 – 0.55 PEEP – 8 cm H2O ABGS: pH 7.36 PaCO2 43 torr PaO2 57 torr HCO3 26 mEq/L BE +2 Based on these data, the most appropriate recommendation is which of the following? A. Increase tidal volume to 750 ml. B. Increase FIO2 to 0.65. C. Increase ventilator rate to 15/min. D. Increase PEEP to 12 cm H2O. 36. The respiratory therapist notes the following data while reviewing the patient’s chart: Dynamic compliance – 34 ml/cm H2O Static compliance – 28 ml/cm H2O The therapist should conclude which of the following? A. Airway resistance is 6 cm H2O/L/sec. B. A pneumothorax has likely developed. C. The data is erroneous. D. The patient has severe obstructive disease. 37. A three-day-old neonate is on a pressure ventilator in the NICU. Ventilator settings and arterial blood gases are recorded below. Mode – IMV pH 7.51 Ventilator rate – 40/min PaCO2 30 torr Inspiratory pressure – 24 cm H2O PaO2 54 torr FIO2 – 0. 50 HCO3 22 mEq/L PEEP – 4 cm H2O BE 0 Based on these data, which of the following is the most appropriate recommendation? A. Decrease the ventilator rate to 35/min. B. Increase the FIO2 to 0.60. C. Increase the inspiratory pressure to 28 cm H2O. D. Increase the PEEP to 6 cm H2O. 97 38. A two-month-old infant is receiving mechanical ventilation with a pressure ventilator. Ventilator settings and capillary blood gases are recorded below. pH 7.36 Mode - IMV PcCO2 44 torr Ventilator rate – 35/min PcO2 55 torr Inspiratory pressure – 24 cm H2O HCO3 23 mEq/L PEEP – 6 cm H2O BE +1 FIO2 – 0.50 The most appropriate recommendation at this time is which of the following? A. Increase the FIO2 to 0.60. B. Decrease PEEP to 4 cm H2O. C. Increase inspiratory pressure to 28 cm H2O. D. Maintain the current settings. 39. A 42-year-old postoperative patient is on the following ventilator settings. Mode – SIMV Ventilator rate – 6/min Tidal volume – 700 ml FIO2 – 0.35 Peak flow – 50 L/min Pressure support – 25 cm H2O During weaning trials using a T-piece, the patient becomes tachypneic, agitated and short of breath, and must be placed back on the ventilator. Based on this information, the respiratory therapist should recommend which of the following to wean this patient? A. Increase the peak flow. B. Increase the FIO2. C. Decrease the pressure support. D. Decrease the tidal volume. 98 40. The following data are collected on an 80 kg (176 lb) man receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.50 Ventilator rate – 8/min PaCO2 29 torr Tidal volume – 800 ml PaO2 57 torr FIO2 – 0.40 HCO3 26 mEq/L Pressure support – 10 cm H2O BE 0 Based on these data, the respiratory therapist should recommend which of the following ventilator changes at this time? A. Decrease the ventilator rate to 6/min. B. Increase the FIO2 to 0.50. C. Decrease the pressure support to 5 cm H2O. D. Decrease the tidal volume to 700 ml. 41. While reviewing a ventilator patient’s chart, the respiratory therapist notes increasing plateau pressures over the past six hours while the tidal volume setting has remained unchanged. Which of the following is the most likely cause of this? A. The patient is experiencing bronchospasm. B. Secretions are present in the upper airways. C. The patient’s lungs are becoming stiffer D. The patient’s FRC is increasing. 42. Which of the following indicates optimal PEEP? PEEP 4 6 8 10 PIP 34 37 42 45 Plateau 22 23 26 29 VT (ml) 600 600 600 600 A. 4 cm H2O B. 6 cm H2O C. 8 cm H2O D. 10 cm H2O 99 43. The following data are collected from a patient receiving mechanical ventilation. PEEP (cm H2O) PvO2 (torr) PaO2 (torr) 3 35 65 6 37 70 9 39 74 12 35 79 Based on these data, which of the following would be the most appropriate level of PEEP? A. 3 cm H2O B. 6 cm H2O C. 9 cm H2O D. 12 cm H2O 44. Cardiac output would most likely be affected least by which of the following ventilator settings? A. SIMV, rate 8/min, PEEP 4 cm H2O B. Assist control, rate 8/min, PEEP 4 cm H2O C. SIMV, rate 12/min, PEEP 6 cm H2O D. Control mode, rate 14/min, PEEP 4 cm H2O 45. A 36-year-old patient with aspiration pneumonia is receiving mechanical ventilation. The chest x-ray indicates complete opacification of the right lung. The left lung appears normal. The patient’s blood pressure is 114/80 mm Hg and PIP is 50 cm H2O. Ventilator settings and ABGs are recorded below. Mode – SIMV Ventilator rate – 18/min Tidal volume – 900 ml FIO2 – 1.0 PEEP – 18 cm H2O pH 7.37 PaCO2 43 torr PaO2 45 torr HCO3 25 mEq/L BE +1 Which of the following should the respiratory therapist recommend at this time? A. Increase the tidal volume to 1.0 L. B. Decrease the ventilator rate to 12/min. C. Increase the PEEP to 24 cm H2O. D. Initiate independent lung ventilation. 100 46. A 70 kg (154 lb) patient is receiving mechanical ventilation in the pressurecontrol mode. Ventilator settings and ABG results are below. Peak inspiratory pressure – 26 cm H2O pH 7.28 Ventilator rate – 10/min PaCO2 54 torr Total rate – 28/min PaO2 67 torr FIO2 – 0.50 HCO3 27 mEq/L Exhaled VT – 250 ml BE +3 Based on these data, which of the following is the most appropriate recommendation? A. Increase ventilator rate to 12/min. B. Increase inspiratory pressure to 30 cm H2O. C. Increase FIO2 to 0.60. D. Initiate PEEP of 4 cm H2O. 47. A 5’6” female patient who weighs 130 kg (286 lb) has just been transported to SICU following abdominal surgery. Which of the following initial ventilator settings are most appropriate? A. SIMV, rate – 12/min, tidal volume – 500 ml B. SIMV, rate – 10/min, tidal volume – 650 ml C. SIMV, rate – 12/min, tidal volume – 900 ml D. SIMV, rate – 8/min, tidal volume – 1300 ml 48. The following data were collected from a patient on a volume ventilator in the control mode. Tidal volume – 700 ml (0.7 L) Ventilator rate – 10/min FIO2 – 0.50 Flow – 50 L/min ABGs: pH 7.27 PaCO2 58 torr PaO2 72 torr HCO3 25 mEq/L BE 0 The physician wants to reduce the patient’s PaCO2 to 45 torr. Which of the following ventilator settings would accomplish this? A. tidal volume – 700 ml, rate – 12/min B. tidal volume – 750 ml, rate – 12/min C. tidal volume – 800 ml, rate – 10/min D. tidal volume – 800 ml, rate – 12/min 101 49. A 34-year-old patient in the ICU is receiving noninvasive positive pressure ventilation by mask. The settings and ABG results are below. Inspiratory positive airway pressure (IPAP) 14 cm H2O Expiratory positive airway pressure (EPAP) 5 cm H2O Respiratory rate 12/min pH 7.29 PaCO2 51 torr PaO2 63 torr HCO3 23 mEq/L BE -1 Which of the following should be recommended to improve the patient’s ventilatory status? A. Increase the EPAP to 10 cm H2O. B. Decrease the IPAP to 12 cm H2O. C. Decrease the EPAP to 3 cm H2O. D. Increase the IPAP to 18 cm H2O. 50. The following data are collected from a patient on a volume ventilator. Tidal volume – 600 ml Peak inspiratory pressure – 35 cm H2O Plateau pressure – 25 cm H2O PEEP – 5 cm H2O This patient’s static lung compliance is which of the following? A. 17 ml/cm H2O B. 20 ml/cm H2O C. 24 ml/cm H2O D. 30 ml/cm H2O 51. A patient is receiving mechanical ventilation with a volume-cycled ventilator. The respiratory therapist hears the low volume alarm and notices that the manometer is reading a system pressure of 3-4 cm H2O during the inspiration phase. The therapist should do which of the following? A. Reconnect the expiratory drive line. B. Suction the patient’s ET tube. C. Drain the water out of the inspiratory line. D. Straighten the kink in the inspiratory line. 102 52. A patient is receiving mechanical ventilation with the following ventilator parameters: SIMV mode Ventilator rate 8 Total rate 32 Ventilator Vt 700 ml Spontaneous Vt 200 ml The physician asks the respiratory therapist to recommend a ventilator mode that would augment the patient’s spontaneous breathing efforts. Which of the following should the therapist select? A. pressure-controlled ventilation (PCV) and titrate the PCV level to achieve a spontaneous Vt of about 10 ml/kg or greater. B. pressure-support ventilation (PSV) and titrate the PSV level until the spontaneous rate is less than 15/min. C. pressure-controlled ventilation (PCV) and titrate PCV until the spontaneous rate is less than 20/min. D. pressure-support ventilation (PSV) and titrate the PSV level until the spontaneous Vt is about 8-10 ml/kg. 53. The following data has been collected on a patient receiving continuous mechanical ventilation. 1:00 PM 3:00 PM Delivered VT 700 ml 700 ml Peak airway pressure 43 cm H2O 54 cm H2O Static airway pressure 28 cm H2O 39 cm H2O Inspiratory flow 50 L/min 50 L/min PEEP 5 cm H2O 5 cm H2O Which of the following is the best interpretation of these data? A. The peak airway pressure increased as a result of increased airway resistance. B. The peak airway pressure increased as a result of decreased lung compliance. C. The patient’s lung compliance is improving. D. The patient’s dynamic compliance is increasing. 103 54. A 27-week gestational age neonate with severe IRDS is receiving high frequency oscillation ventilation (HFOV). The neonate has a heart rate of 150/min and a blood pressure of 66/42 mm Hg. Arterial blood gases drawn thirty minutes after initiation of HFOV are recorded below. pH 7.24 PaCO2 62 torr PaO2 60 torr HCO3 23 mEq/L BE -1 The respiratory therapist should recommend which of the following? A. increasing the oscillatory amplitude B. increasing the FIO2 C. initiating conventional ventilation D. decreasing the mean airway pressure 55. The following information is from a patient receiving pressure-control ventilation. 9:00 AM 11:00 AM Rate 14/min 14/min Peak pressure 30 cm H2O 30 cm H2O PEEP 5 cm H2O 5 cm H2O Exhaled VT 700 ml 500 ml This information is consistent with a decreased A. lung compliance. B. A-a gradient. C. airway resistance. D. VD/VT ratio. 56. The following data is collected from a 65 kg (143 lb) patient with a closedhead injury and elevated intracranial pressure levels receiving volume-cycled ventilation. Mode - SIMV Mandatory rate - 10/min Total rate - 10/min Tidal volume - 800 ml FIO2 - 0.50 pH 7.48 PaCO2 28 torr PaO2 98 torr HCO3 25 mEq/L Which of the following should the respiratory therapist recommend at this time? A. Decrease the FiO2 to 0.40. B. Decrease the tidal volume to 700 ml. C. Maintain the ventilator settings. D. Add 100 ml of deadspace. 104 57. The following data are collected on an 80 kg (176 lb) man receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.50 Ventilator rate – 8/min PaCO2 26 torr Total rate 18/min PaO2 92 torr Tidal volume – 800 ml HCO3 26 mEq/L FIO2 – 0.40 BE +2 Pressure support – 25 cm H2O Which of the following ventilator changes are appropriate at this time? A. Decrease the pressure support. B. Add deadspace. C. Decrease the SIMV rate D. Make no changes at this time. 58. The following data are collected on a 70 kg (154 lb) female receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.28 Ventilator rate – 10/min PaCO2 53 torr Total rate 22/min PaO2 72 torr Tidal volume – 700 ml HCO3 23 mEq/L FIO2 – 0.40 BE -2 Pressure support – 7 cm H2O Deadspace – 100 ml PEEP – 5 cm H2O Which of the following ventilator changes are appropriate at this time? A. Increase the pressure support to 10 cm H2O. B. Remove the deadspace. C. Increase the SIMV rate to 15/min. D. Increase the PEEP to 10 cm H2O. 105 59. The following data are collected on a 70 kg (154 lb) female receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.48 Ventilator rate – 12/min PaCO2 30 torr Total rate 24/min PaO2 62 torr Tidal volume – 800 ml HCO3 23 mEq/L FIO2 – 0.65 BE -2 Pressure support – 7 cm H2O PEEP – 5 cm H2O Which of the following ventilator changes are appropriate at this time? A. Increase the PEEP to 10 cm H2O. B. Decrease the tidal volume to 700 ml. C. Decrease the SIMV rate to 8/min. D. Decrease the pressure support to 5 cm H2O. 60. The following data are collected on a 70 kg (154 lb) female receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.43 Ventilator rate – 10/min PaCO2 43 torr Total rate 14/min PaO2 125 torr Tidal volume – 700 ml HCO3 26 mEq/L FIO2 – 0.40 BE +2 Pressure support – 10 cm H2O PEEP – 10 cm H2O Which of the following ventilator changes should the respiratory therapist recommend? A. Decrease the pressure support to 5 cm H2O. B. Decrease the FIO2 to 0.30. C. Decrease the SIMV rate to 6/min. D. Decrease the PEEP to 5 cm H2O. 106 61. The following data are collected on a 70 kg (154 lb) female with bibasilar atelectasis receiving mechanical ventilation with a volume ventilator. Mode – SIMV Ventilator rate – 10/min Total rate 24/min Tidal volume – 600 ml FIO2 – 0.40 PEEP – 5 cm H2O ABGS: pH 7.29 PaCO2 53 torr PaO2 65 torr HCO3 27 mEq/L BE +3 Which of the following ventilator changes should the respiratory therapist recommend? A. Increase the SIMV rate to 15/min. B. Increase the FIO2 to 0.50. C. Increase the tidal volume to 700 ml. D. Increase the PEEP to 10 cm H2O. 62. The following data are collected on a 65 kg (143 lb) female with severe COPD receiving mechanical ventilation with a volume ventilator. Mode – SIMV ABGS: pH 7.35 Ventilator rate – 10/min PaCO2 63 torr Total rate 14/min PaO2 62 torr Tidal volume – 600 ml HCO3 36 mEq/L FIO2 – 0.40 BE +12 Pressure support – 10 cm H2O PEEP – 4 cm H2O Which of the following ventilator changes should the respiratory therapist recommend? A. Increase the pressure support to 15 cm H2O. B. Increase the FIO2 to 0.50. C. Increase the tidal volume to 700 ml. D. Maintain the current ventilator settings. 107 63. The following data are collected on a patient receiving mechanical ventilation with a volume ventilator. Mode – A/C ABGS: pH 7.43 Ventilator rate – 10/min PaCO2 43 torr Tidal volume – 700 ml PaO2 125 torr FIO2 – 0.80 HCO3 26 mEq/L PEEP – 12 cm H2O BE 0 Which of the following ventilator changes should the respiratory therapist recommend? A. Decrease the PEEP to 8 cm H2O. B. Decrease the FIO2 to 0.70. C. Increase the rate to 15/min. D. Decrease the tidal volume to 600 ml. 64. A patient in the ICU is receiving noninvasive positive pressure ventilation by mask. The settings and ABG results are below. Inspiratory positive airway pressure (IPAP) 15 cm H2O Expiratory positive airway pressure (EPAP) 5 cm H2O Respiratory rate 12/min pH 7.28 PaCO2 53 torr PaO2 73 torr HCO3 24 mEq/L BE -1 Which of the following changes are appropriate at this time? A. Increase the EPAP to 8 cm H2O. B. Decrease the IPAP to 12 cm H2O. C. Decrease the EPAP to 3 cm H2O. D. Increase the IPAP to 18 cm H2O. 65. Which of the following would most likely indicate that a ventilator patient is ready to be weaned? I. MIP of –17 cm H2O II. VC of 18 ml/kg III. P(A-a)O2 of 475 torr on 100% oxygen IV. VD/VT of 0.50 A. I and II only B. II and IV only C. II, III and IV only D. I, II, III and IV 108 66. The respiratory therapist is assessing a ventilator patient to determine if weaning is appropriate. Which of the following parameters indicate weaning will most likely be successful? I. VC – 14 ml/kg II. Rapid shallow breathing index – 70 III. MIP – -32 cm H2O A. I only B. III only C. II and III only D. I, II and III 67. A patient receiving mechanical ventilation is placed on a PEEP of 5 cm H2O. Which of the following will most likely increase? I. FRC II. P(A-a)O2 III. static lung compliance A. I only B. II only C. I and III only D. I, II and III 68. A two-month-old infant is receiving mechanical ventilation with a pressure ventilator. Ventilator settings and capillary blood gases are recorded below. pH 7.38 Mode - IMV PcCO2 46 torr Ventilator rate – 25/min PcO2 45 torr Inspiratory pressure – 20 cm H2O HCO3 22 mEq/L PEEP – 4 cm H2O BE -1 FIO2 – 0.40 The most appropriate recommendation at this time is which of the following? A. Increase the FIO2 to 0.50. B. Increase PEEP to 6 cm H2O. C. Increase inspiratory pressure to 24 cm H2O. D. Maintain the current settings. 109 69. The following data are collected from a patient on a volume ventilator. Tidal volume – 800 ml Peak inspiratory pressure – 50 cm H2O Plateau pressure – 30 cm H2O PEEP – 10 cm H2O This patient’s static lung compliance is which of the following A. 16 ml/cm H2O B. 20 ml/cm H2O C. 27 ml/cm H2O D. 40 ml/cm H2O 70. The following data are collected from a patient receiving mechanical ventilation. PEEP (cm H2O) SvO2 SaO2 4 75% 93% 6 78% 94% 8 73% 96% 10 72% 96% Based on these data, which of the following would be the most appropriate level of PEEP? A. 4 cm H2O B. 6 cm H2O C. 8 cm H2O D. 10 cm H2O 71. A patient on a volume ventilator has a PaO2 of 62 torr on a PEEP of 6 cm H2O and an FiO2 of 0.50. After increasing the PEEP to 10 cm H2O, the cardiac output decreases from 5.1 L/min to 4.1 L/min. The most appropriate recommendation is to A. discontinue PEEP and increase the FiO2 to 0.60. B. increase PEEP to 10 cm H2O. C. decrease PEEP to 6 cm H2O and increase the FiO2 to 0.60. D. maintain the current settings and measure cardiac output in one hour. 110 72. A patient is receiving mechanical ventilation with a volume-cycled ventilator. The low pressure alarm is activated and the manometer is reading a system pressure of 2-3 cm H2O during the inspiration phase. The respiratory therapist should do which of the following? A. Check to function of the expiratory valve. B. Suction the patient’s ET tube. C. Drain the water out of the inspiratory line. D. Straighten the kink in the inspiratory line. 73. The respiratory therapist notes the following data while reviewing the patient’s chart: Dynamic compliance – 44 ml/cm H2O Static compliance – 32 ml/cm H2O The therapist should conclude which of the following? A. Airway resistance is 12 cm H2O/L/sec. B. A pneumothorax has likely developed. C. The data is erroneous. D. The patient has severe restrictive disease. 74. The following data has been obtained from a patient on a volume ventilator and a tidal volume of 700 ml. Time 2 PM 3 PM 4 PM peak pressure (cm H2O) 30 36 40 plateau pressure (cm H2O) 18 18 18 Which of the following statements regarding these data are true? A. Lung compliance is decreasing. B. Airway resistance is increasing. C. The lungs are becoming easier to ventilate. D. Lung compliance is increasing. 111 75. The following data has been obtained from a patient on a volume ventilator and a tidal volume of 650 ml. Time 6 PM 7 PM 8 PM peak pressure plateau pressure (cm H2O) (cm H2O) 34 16 38 20 41 24 Which of the following statements regarding these data are true? A. Static lung compliance is decreasing. B. Airway resistance is increasing. C. The lungs are becoming easier to ventilate. D. Dynamic lung compliance is increasing. 76. A 49-year-old postoperative patient is on the following ventilator settings. Mode – SIMV Ventilator rate – 6/min Tidal volume – 600 ml FIO2 – 0.40 Peak flow – 60 L/min Pressure support – 24 cm H2O A weaning trial is started with the patient being placed on a T-piece. The patient becomes tachypneic and short of breath, and must be placed back on the ventilator. Based on this information, the respiratory therapist should recommend which of the following? A. Increase the peak flow. B. Increase the FIO2 to 0.50 while on the T-piece. C. Decrease the pressure support to 10 cm H2O. D. Increase the tidal volume to 650 ml. 112 77. A two-day-old neonate is on a pressure ventilator in the NICU. Ventilator settings and arterial blood gases are recorded below. Mode – IMV pH 7.43 Ventilator rate – 40/min PaCO2 42 torr Inspiratory pressure – 20 cm H2O PaO2 44 torr FIO2 – 0. 60 HCO3 22 mEq/L PEEP – 4 cm H2O BE 0 Based on these data, which of the following is the most appropriate recommendation? A. Decrease the ventilator rate to 35/min. B. Increase the FIO2 to 0.70. C. Increase the inspiratory pressure to 24 cm H2O. D. Increase the PEEP to 6 cm H2O. 78. A five-day-old premature neonate is on a pressure ventilator in the NICU. Ventilator settings and arterial blood gases are recorded below. Mode – IMV pH 7.29 Ventilator rate – 30/min PaCO2 51 torr Inspiratory pressure – 20cm H2O PaO2 50 torr FIO2 – 0. 40 HCO3 24 mEq/L PEEP – 6 cm H2O BE +2 Based on these data, which of the following is the most appropriate recommendation? A. Increase the ventilator rate to 35/min. B. Increase the FIO2 to 0.50. C. Decrease the inspiratory pressure to 18 cm H2O. D. Increase the PEEP to 8 cm H2O. 79. A drug overdose patient is being transferred to the ICU. The patient weighs 60 kg (132 lb) and is being bagged with 100%. Which of the following represents the most appropriate initial ventilator settings? A. mode – A/C, tidal volume – 600 ml, rate – 6/min, FIO2 – 0.60 B. mode – control, tidal volume – 800 ml, rate – 12/min, FIO2 – 0.60 C. mode – A/C, tidal volume – 650 ml, rate – 16/min, FIO2 – 1.0 D. mode – SIMV, tidal volume – 600 ml, rate – 12/min, FIO2 – 1.0 113 80. A premature infant on a pressure-controlled ventilator has a PaCO2 of 28 torr. Which of the following ventilator settings should be decreased to correct this situation? A. FiO2 B. tidal volume C. PEEP D. inspiratory pressure 81. The following data are collected on a patient receiving mechanical ventilation with a volume ventilator. Mode – A/C ABGS: pH 7.28 Ventilator rate – 10/min PaCO2 53 torr Tidal volume – 700 ml PaO2 75 torr FIO2 – 0.50 HCO3 25 mEq/L PEEP – 8 cm H2O BE 0 Which of the following ventilator changes should the respiratory therapist recommend? A. Increase the PEEP to 10 cm H2O. B. Increase the FIO2 to 0.60. C. Increase the tidal volume to 800 ml.. D. Add 100 ml of deadspace. 82. The following data are collected on a patient receiving mechanical ventilation with a volume ventilator. Mode – SIMV Ventilator rate – 8/min Tidal volume – 700 ml FIO2 – 0.40 PEEP – 4 cm H2O ABGS: pH 7.48 PaCO2 33 torr PaO2 95 torr HCO3 24 mEq/L BE -1 Which of the following ventilator changes should the respiratory therapist recommend? A. Add mechanical deadspace. B. Decrease the FIO2 to 0.25. C. Decrease the rate to 6/min. D. Decrease the tidal volume to 600 ml. 114 83. The following data are collected on a 70 kg (154 lb) ventilator patient who has suffered head trauma as a result of a motor vechicle accident. The patient has an ICP of 18 mm Hg. Mode – A/C Ventilator rate – 10/min Tidal volume – 700 ml FIO2 – 0.40 ABGS: pH 7.31 PaCO2 47 torr PaO2 95 torr HCO3 24 mEq/L BE -1 Which of the following ventilator changes should the respiratory therapist recommend? A. Increase the tidal volume to 800 ml. B. Decrease the FIO2 to 0.30. C. Maintain current ventilator settings. D. Increase the rate to 15/min. 84. A 27-year-old male weighing 65 kg (143 lb) is receiving mechanical ventilation after being diagnosed with a drug overdose. Her chest radiograph is consistent with pulmonary edema. Pertinent data are listed below. Mode – SIMV ABGs: pH 7.41 Rate – 12/min PaCO2 38 torr Tidal volume – 650 ml PaO2 49 torr FIO2 – 0.60 HCO3 26 PEEP – 8 cm H2O BE +1 PIP – 54 cm H2O SaO2 83% Plateau pressure – 45 cm H2O Which of the following changes should the respiratory therapist recommend at this time? I. Change mode to pressure control at 35 cm H2O. II. Increase the FIO2 to 0.70. III. Increase the PEEP to 12 cm H2O. IV. Increase the rate to 20/min. A. I and III only B. II and IV only C. I, III and IV only D. II, III and IV only 115 85. The following data are collected on a patient receiving mechanical ventilation with a volume ventilator. Mode – A/C ABGS: pH 7.38 Ventilator rate – 10/min PaCO2 42 torr Tidal volume – 700 ml PaO2 131 torr FIO2 – 0.70 HCO3 26 mEq/L PEEP – 10 cm H2O BE +2 Which of the following ventilator changes should the respiratory therapist recommend? A. Decrease the PEEP to 8 cm H2O. B. Decrease the FIO2 to 0.60. C. Increase the rate to 15/min. D. Decrease the tidal volume to 600 ml. 86. The following data are collected on a 7-year-old child who weighs 30 kg (66 lb) and is receiving mechanical ventilation. Mode – A/C ABGS: pH 7.48 Ventilator rate – 22/min PaCO2 31 torr Tidal volume – 300 ml PaO2 57 torr FIO2 – 0.80 HCO3 21 mEq/L BE -2 Which of the following ventilator changes should the respiratory therapist recommend? A. Initiate 5 cm H2O PEEP. B. Decrease the rate to 18/min. C. Increase the FIO2 to 0.90. D. Decrease the tidal volume to 250 ml. 116 87. The following data are collected on a 55-year-old COPD patient receiving mechanical ventilation with a volume ventilator. Mode – A/C ABGS: pH 7.36 Ventilator rate – 10/min PaCO2 58 torr Tidal volume – 900 ml PaO2 67 torr FIO2 – 0.35 HCO3 35 mEq/L BE +10 Which of the following ventilator changes should the respiratory therapist recommend? A. Maintain the current settings. B. Increase the FIO2 to 0.45. C. Increase the rate to 15/min. D. Decrease the tidal volume to 750 ml. 88. The blood gas results below are for a 75 kg (165 lb) COPD patient who is breathing room air. pH 7.26 PaCO2 75 torr PaO2 40 torr HCO3 38 mEq/L BE +12 Which of the following ventilator settings is most appropriate for this patient? A. tidal volume – 900 ml, rate – 10/min, FIO2 – 0.60 B. tidal volume – 700 ml, rate – 12/min, FIO2 – 0.40 C. tidal volume – 750 ml, rate – 15/min, FIO2 – 0.50 D. tidal volume – 800 ml, rate – 8/min, FIO2 - 0.80 117 89. The following data are collected on a 60 kg (132 lb) patient receiving mechanical ventilation with a volume ventilator. Mode – A/C Ventilator rate – 10/min Tidal volume – 700 ml FIO2 – 1.0 PEEP – 12 cm H2O PIP – 55 cm H2O SpO2 – 83% A chest radiograph indicates diffuse bilateral infiltrates. Which of the following ventilator changes should the respiratory therapist recommend? A. Increase the PEEP to 16 cm H2O. B. Increase the ventilator rate. C. Change to pressure-control ventilation. D. Decrease the tidal volume to 600 ml. 90. Which of the following flow settings is required to maintain an I:E ratio of 1:2 with a respiratory rate of 20/min and a tidal volume of 700 ml? A. 28 L/min B. 36 L/min C. 42 L/min D. 48 L/min 91. The following data has been collected on a mechanical ventilator patient. A/C mode rate – 15/min flowrate – 60 L/min FIO2 – 0.40 PIP – 30 cm H2O plateau pressure – 15 cm H2O Based on this information, which of the following represents the patient’s airway resistance (Raw)? A. 5 cm H2O/L/sec B. 10 cm H2O/L/sec C. 15 cm H2O/L/sec D. 20 cm H2O/L/sec 118 92. Which of the following indicates the patient’s static lung compliance is increasing? A. increasing peak pressure B. increasing plateau pressure C. decreasing peak pressure D. decreasing plateau pressure 93. Which of the following pressures below indicate the best static lung compliance? A. PEEP – 4 cm H2O plateau – 24 cm H2O Vt – 700 ml B. PEEP – 8 cm H2O plateau – 26 cm H2O Vt – 700 ml C. PEEP – 12 cm H2O plateau – 34 cm H2O Vt – 700 ml D. PEEP – 15 cm H2O plateau - 38 cm H2O Vt – 700 ml 94. The physician wants to help reduce cerebral blood flow to a closed-head injury patient by using the ventilator. Which of the following PaCO2 levels would be most appropriate to maintain on this patient? A. 20 torr B. 30 torr C. 40 torr D. 50 torr 95. A four-day-old neonate on CPAP of 6 cm H2O and 60% oxygen is experiencing nasal flaring, grunting and retractions with a respiratory rate of 72/min. The SpO2 is 82%. Which of the following should the respiratory therapist recommend? A. Increase CPAP to 10 cm H2O. B. Intubate and initiate mechanical ventilation. C. Place on 100% oxygen hood. D. Administer a bronchodilator. 119 Disorders of the Respiratory System 1. Which of the following should be taught to the COPD patient to help relieve dyspnea? I. diaphragmatic breathing II. increased accessory muscle use III. pursed lip breathing A. I and II only B. I and III only C. II and III only D. I, II and III 2. The respiratory care practitioner is assessing a patient in the emergency room who states he has had a cough off and on for the past three years which often produces thick secretions. The practitioner should suspect this patient most likely has A. asthma. B. emphysema. C. chronic bronchitis. D. pulmonary edema. 3. The respiratory therapist obtains a sputum sample from a patient and the lab report determines it contains acid-fast bacilli. This is indicative of which of the following lung conditions? A. tuberculosis B. asthma C. emphysema D. bronchiectasis 4. Which of the following should the respiratory therapist recommend as the most effective treatment for an obese patient with obstructive sleep apnea? A. Have the patient sleep on their right side. B. Recommend a tracheotomy be done. C. Have the patient sleep sitting up in a chair. D. Sleep using nasal CPAP. 120 5. The respiratory care practitioner is evaluating a ventilator patient with ARDS. Which of the following findings is commonly assessed with this lung disorder? I. increased lung compliance II. refractory hypoxemia III. decreased P(A-a)O2 A. II only B. I and II only C. I and III only D. II and III only 6. A patient enters the emergency department following a motor vehicle accident in severe respiratory distress. Upon assessment of the patient, the respiratory care practitioner observes asymmetrical chest movement with absent breath sounds on the right and the trachea shifted toward the left. Which of the following should the practitioner recommend first? A. Obtain a stat chest x-ray. B. Intubate and manually ventilate the patient. C. Evacuate air from the pleural space. D. Administer a stat IPPB treatment. 7. The respiratory care practitioner is assessing a patient in the emergency department who presents with shortness of breath and is coughing up large amounts of pink, frothy secretions. The practitioner auscultates crackles throughout all lung fields. This patient’s most likely diagnosis is which of the following? A. pulmonary embolism B. bacterial pneumonia C. bronchiectasis D. pulmonary edema 8. A 77-year-old patient is recovering on the orthopedic floor from a broken hip. After being moved to a bedside chair the patient suddenly becomes dyspneic, cyanotic and tachycardic. This sudden deterioration in the patient’s condition is most likely the result of which of the following? A. pulmonary edema B. pneumonia C. pneumothorax D. pulmonary embolism 121 9. A 16-year-old patient enters the emergency department in moderate respiratory distress. She states she suffered an asthma attack less than one hour ago with no improvement using her routine medication regimen. Which of the following arterial blood gas results on room air would you expect at this time? A. pH 7.26, PaCO2 56 torr, PaO2 52 torr, HCO3 25 mEq/L B. pH 7.54, PaCO2 40 torr, PaO2 78 torr, HCO3 36 mEq/L C. pH 7.47, PaCO2 31 torr, PaO2 57 torr, HCO3 25 mEq/L D. pH 7.28, PaCO2 43 torr, PaO2 81 torr, HCO3 15 mEq/L 10. While evaluating a patient’s chest x-ray, the respiratory care practitioner observes areas of hyperinflated lung markings, a flattened diaphragm and reduced vascular markings. This x-ray is indicative of which of the following? A. emphysema B. pleural effusion C. pneumothorax D. pulmonary edema 11. Cor pulmonale is an indication of A. an elevated PCWP. B. right ventricular hypertrophy. C. systemic hypertension. D. decreased pulmonary vascular resistance. 12. While assessing the patient’s laboratory results, the respiratory care practitioner notices an elevated eosinophil level in the patient’s sputum. The practitioner should suspect the patient most likely has which of the following lung conditions? A. carcinoma of the lung B. bronchiectasis C. asthma D. emphysema 122 13. Pulmonary vascular congestion caused by congestive heart failure may result in which of the following? I. pneumothorax II. orthopnea III. paroxysmal nocturnal dyspnea IV. Kussmaul’s respirations A. I and II only B. II and III only C. II, III and IV only D. I, II, III and IV 14. The most common initial treatment for a patient with pulmonary thromboembolic disease is which of the following? A. heparin B. Lasix C. Lidocaine D. Atropine 15. The respiratory therapist is evaluating a chest radiograph on a patient with a pulmonary embolism and observes an elevated right hemidiaphragm. This is most likely the result of which of the following? A. pneumothorax B. pleural effusion C. atelectasis D. infiltrates 16. Which of the following would you expect to observe on a 25-year-old female patient with cystic fibrosis? I. digital clubbing II. increased A-P chest diameter III. pedal edema A. I only B. I and II only C. II and III only D. I, II and III 123 17. The respiratory therapist observes jugular venous distension (JVD) during a patient evaluation on a patient with chronic bronchitis. The JVD is most likely the result of which of the following? A. cor pulmonale B. atelectasis C. pulmonary hyperinflation D. decreased CVP level 18. Which of the following are common findings for patients with acute respiratory distress syndrome (ARDS)? I. decreased V/Q mismatch II. decreased lung compliance III. PaO2/FIO2 < 150 IV. normal PCWP A. I and II only B. II and III only C. I, II and IV only D. II, III and IV only 19. The most common causative organism of epiglottitis is A. pseudomonas aeruginosa. B. Streptococcus. C. type B Haemophilus influenza. D. parainfluenza virus. 20. The physician has ordered 30% oxygen for a 3-year-old boy with croup. Which of the following devices would be most appropriate to deliver the oxygen? A. nasal cannula B. nonrebreathing mask C. oxygen tent D. oxyhood 21. A flail chest is most commonly associated with A. pleural effusion B. chest trauma C. pneumonia D. emphysema 124 22. Which of the following conditions may result in a decreased lung compliance? I. atelectasis II. pneumonia III. pulmonary edema IV. emphysema A. I and II only B. III and IV only C. I, II and III only D. I, II, III and IV 23. A patient is suspected of having a pulmonary embolus. Which of the following should the respiratory therapist recommend to aid in the diagnosis? A. chest radiograph B. lung scan C. bronchoscopy D. pulmonary angiography 24. A polysomnogram shows no air flow with abdominal and chest movement. This is indicative of which of the following? A. obstructive sleep apnea B. normal polysomnogram C. central sleep apnea D. mixed apnea 25. Which of the following characteristics are common in patients with severe COPD? I. pulmonary hypertension II. decreased lung compliance III. right ventricular hypertrophy IV. decreased Hb level A. I and III only B. II and IV only C. I, II and III only D. II, III and IV only 125 26. Which of the following should the respiratory therapist suggest to a long term smoker with COPD prior to discharge from the hospital? I. nicotine patches II. smoking cessation program III. breathing exercise training A. I only B. I and II only C. II and III only D. I, II and III 27. Purulent, foul-smelling secretions are most commonly associated with which of the following? I. bronchiectasis II. pulmonary edema III. lung abscess IV. asthma A. I and II only B. I and III only C. II and IV only D. I, III and IV only 28. A patient brought into the emergency department was found unconscious and lying on his back. He is suspected to have vomited and aspirated. Which of the following lungs segments would most likely be involved in the aspiration event? A. anterior segment of right upper lobe B. lateral segment of left lower lobe C. posterior segment of right upper lobe D. anterior segment of left upper lobe 29. Which of the following are common pathological consequences of aspiration pneumonitis? I. severe hypoxemia II. reduced intrapulmonary shunting III. ventilation-perfusion mismatch A. I only B. I and III only C. II and III only D. I, II and III 126 30. Which of the following could result in a transudative pleural effusion? A. bacterial infection B. metastatic lung disease C. pulmonary embolism D. congestive heart failure 31. It is noted in the patient’s chart that during that pus is removed from the pleural space of a patient during a thoracentesis. This is indicative of which of the following? A. pyothorax B. hemothorax C. pneumothorax D. chylothorax 32. The most common presenting symptom with pulmonary embolism is A. dyspnea. B. anxiety. C. hemoptysis. D. cough. 33. Postoperative pneumonia can be the result of which of the following? I. ineffective cough II. abnormal mucus transport III. aspiration of upper airway secretions A. I only B. I and II only C. II and III only D. I, II and III 34. It is noted in the patient’s chart that the patient has recurrent and unresolved pulmonary emboli. This may directly result in which of the following clinical conditions? A. hypertension B. right ventricular hypertrophy C. left ventricular hypertrophy D. mitral valve stenosis 127 35. Cardiogenic pulmonary edema would be indicated by which of the following values? A. PAP – 26/14 B. PCWP – 28 mm Hg C. CVP – 5 mm Hg D. Cardiac output – 4.8 L/min 128 Respiratory Medications 1. A 12-year-old patient with cystic fibrosis is having difficulty expectorating his thick pulmonary secretions. The respiratory care practitioner should recommend administering which of the following medications to treat this condition? A. normal saline B. Mucomyst C. aminophylline D. cromolyn sodium 2. The respiratory therapist is having difficulty intubating a combative patient. To temporarily paralyze the patient to facilitate tracheal intubation, which of the following medications should be administered? A. succinylcholine B. Valium C. Pavulon D. Versed 3. Immediately following extubation, the patient becomes short of breath and inspiratory stridor is heard. The respiratory care practitioner should recommend which of the following to reduce the upper airway edema? A. Terbutaline B. Atrovent C. Mucomyst D. Racemic epinephrine 4. A 12-year-old asthmatic patient is being release from the hospital following a 2-day stay to treat her condition. Upon discharge, the respiratory care practitioner should recommend which of the following medications to help prevent further attacks? A. cromolyn sodium (Intal) B. Theophylline C. metaproteronol (Alupent) D. terbutaline sulfate (Brethine) 129 5. To help stimulate a cough in order to obtain a sputum culture from a patient, the respiratory care practitioner should recommend aerosol therapy with the administration of which of the following? A. sterile water B. hypotonic saline C. normal saline D. hypertonic saline 6. A 6-month-old infant is diagnosed with respiratory syncytial virus (RSV). The respiratory care practitioner should recommend which of the following aerosolized medications? A. beclovent B. ribavirin C. pentamidine D. amphotericin B 7. A patient in cardiogenic shock has a blood pressure of 70/40. The respiratory therapist should recommend which of the following medications to treat this patient’s hypotension? A. Dopamine (Intropin) B. Lidocaine (Xylocaine) C. Nitroprusside (Nipride) D. Furosemide (Lasix) 8. Oral candidiasis is a potential side effect of which of the following medications? I. Ipratropium bromide (Atrovent) II. Flunisolide (AeroBid) III. Beclomethasone (Beclovent) A. II only B. I and II only C. II and III only D. I, II and III 130 9. Atrovent is characterized as which type of respiratory medication? A. beta adrenergic bronchodilator B. anticholinergic bronchodilator C. steroid D. mucolytic 10. The physician wants to add a medication to a cystic fibrosis patient’s aerosol therapy treatment that will help reduce the viscosity of his pulmonary secretions. Which of the following would be the most appropriate drug to recommend? A. atrovent B. serevent C. pulmozyme D. albuterol 11. A 24-year-old asthmatic is being mechanically ventilated. His rate is 38/min and he appears very agitated. The high pressure alarm is frequently being triggered. The patient’s breath sounds are equal bilaterally with few wheezes. Which of the following should the respiratory therapist recommend at this time? A. succinylcholine (Anectine) B. cromolyn sodium (Intal) C. midazolam (Versed) D. flunisolide (Aerobid) 12. A patient has been diagnosed with aspergillosis. Which of the following medications should the respiratory therapist recommend to treatment this condition? A. amphotericin B B. ribavirin C. pentamidine D. gentamicin 13. A patient experiencing bronchospams is receiving metaproterenol sulfate (Alupent) and his heart rate increases by 40 beats/min with each treatment. Which of the following medications should the respiratory therapist recommend in place of Alupent? A. beclomethasone (Vanceril) B. cromolyn sodium (Intal) C. albuterol (Proventil) D. acetylcysteine (Mucomyst) 131 14. Thick, tenacious secretions are best mobilized from the airway using which of the following medications? I. beclomethasone II. pulmozyme III. Mucomyst A. I only B. I and II only C. II and III only D. I, II and III 15. The following hemodynamic data is recorded for a patient: heart rate 86/min cardiac output 3.9 L/min SVR 3200 dynes. sec. cm-5 Blood pressure 162/98 Which of the following medications is the most appropriate recommendation? A. albuterol (Proventil) B. furosemide (Lasix) C. dopamine (Intropin) D. nitroprusside (Nipride) 16. A patient is brought into the emergency department following a motor vechicle accident. The patient is in shock with a blood pressure of 72/42. Which of the following medications is most appropriate to recommend at this time? A. furosemide (Lasix) B. dopamine (Intropin) C. nitroprusside (Nipride) D. beclomethasone (Vanceril) 17. A patient with status asthmaticus is being mechanically ventilated. Over the past two hours, the patient’s dynamic compliance has dramatically decreased. Which of the following drugs should be recommended to help improve this situation the fastest? A. beclomethasone (Vanceril) B. albuterol (Proventil) C. racemic epinephrine (Vaponefrin) D. cromolyn sodium (Intal) 132 18. The physician wants to paralyze an agitated, combative asthmatic patient who is being mechanically ventilated. Which of the following would the most appropriate drug to utilize at this time? A. vecuronium (Norcuron) B. succinylcholine (Anectine) C. d-tubocurarine (Curare) D. midazolam (Versed) 19. The physician is preparing to perform a bronchoscopy on a patient with suspected lung cancer. The Doctor wants to accomplish conscious sedation for the procedure. The respiratory therapist should recommend which of the following medications? A. midazolam (Versed) B. vecuronium (Norcuron) C. succinylcholine (Anectine) D. pancuronium (Pavulon) 20. An HIV positive patient has been diagnosed with Pneumocystis carinii pneumonia. Which of the following medications should the respiratory therapist recommend to treat this pneumonia? A. pancuronium (Pavulon) B. gentamicin C. pentamidine (NebuPent) D. rifampin (Rifadin) 21. A patient being mechanically ventilated in the asist/control mode and a rate of 12/min is cycling the ventilator at a rate of 34/min. The patient is anxious and agitated and has the following ABG results: pH 7.55 PaCO2 25 torr PaO2 96 torr HCO3 25 mEq/L BE +1 Which of the following medications should the respiratory therapist recommend at this time? A. albuterol (Proventil) B. nitroprusside (Nipride) C. theophyilline (Aminophylline) D. midazolam (Versed) 133 22. The physician is preparing to perform a bronchoscopy on a patient and wants to make sure the airway is dry prior to beginning the procedure. Which of the following drugs shold the respiratory therapist administer to accomplish this? A. atropine sulfate (Atropisol) B. midazolam (Versed) C. albuterol (Proventil) D. furosemide (Lasix) 23. Following extubation the patient begins experiencing inspiratory stridor and shortness of breath. The respiratory therapist should recommend administering which of the following medications? A. terbutaline (Breathine) B. metaproterenol sulfate (Alupent) C. racemic epinephrine (Vaponefrin) D. ipratropium bromide (Atrovent) 24. A patient is receiving 0.5 ml of albuterol (Proventil) in 2.5 ml of NaCl through a small-volume nebulizer. The patient’s heart rate increases from 82/min at the start of the treatment to 128/min half way through the treatment. The patient is also experiencing tremors. The respiratory therapist should recommend which of the following at this time? A. Instruct the patient to breath in deeper breaths. B. Decrease the dosage of the albuterol. C. Instruct the patient to breath slower. D. Recommend changing to Alupent. 25. During a fiberoptic bronchoscopy, the patient’s airway begins to bleed following tissue biopsy. Which of the following should be instilled down the bronchoscope to help stop the bleeding? A. epinephrine B. xylocaine C. hypertonic saline D. isoproteronol 134 Pulmonary Function Testing 1. The FEF 25-75 is measured using which of the following pulmonary function tests? A. FRC B. FVC C. TLC D. MVV 2. Which of the following pulmonary function values are increased in patients with emphysema? A. FVC B. FEF 200-1200 C. FRC D. MVV 3. To best determine an asthmatic’s response to a bronchodilator, which of the following tests should be performed before and after the use of a bronchodilator? A. tidal volume B. minute volume C. peak flow D. maximal inspiratory pressure 4. The respiratory care practitioner explains to the patient at his bedside to take the deepest breath he can and exhale completely as fast and forcefully as possible. From this instruction, the practitioner will be able to measure the patient’s A. FVC. B. FRC. C. MVV D. tidal volume. 135 5. Below are the results of a patient’s spirometry test before and after a bronchodilator is administered. Before After FEV1 38% of predicted 55% of predicted FVC 40% of predicted 59% of predicted FEV1 / FVC 42% 61% Which of the following is the correct interpretation of these results? A. severe restrictive disease with significant bronchodilator response B. severe obstructive disease with significant bronchodilator response C. mild restrictive disease with no significant bronchodilator response D. severe obstructive disease with no significant bronchodilator response 6. Vital capacity is defined as the sum of which of the following? A. VT + IRV + ERV B. IRV + RV + FRC C. IC + ERV D. VT + FRC + ERV 7. Below are the results of a PFT performed on a 52-year-old male patient. VC 2.1 L FRC 1.4 L TLC 2.8 L RV .84 L FEV1% FEF25-75 Actual Predicted %Predicted 3.2 L 66% 2.2 L 64% 4.3 L 65% 1.2 L 70% 84% 76% 4.2 L 4.5 L 93% These results indicate which of the following? A. obstructive disorder B. restrictive disorder C. combined restrictive and obstructive disorder D. small airway obstruction 136 8. Below are PFT values obtained on a 47-year-old female patient. Actual Predicted %Predicted VC 2.24 L 3.5 L 64% TLC 3.51 L 5.4 L 65% FEV/FVC 68% 75% These results are indicative of which of the following? A. restrictive lung disorder B. obstructive lung disorder C. combined restrictive and obstructive lung disorder D. normal PFT values 9. The following PFT values have been obtained on a 57-year-old male. Actual Predicted %Predicted FEV1 1.4 L 3.0 L 47% FEV/FVC 48% 70% VC 2.1 L 3.8 L 55% TLC 6.4 L 4.8 L 133% FRC 3.4 L 2.5 L 136% Which of the following pulmonary disorders is consistent with these findings? A. pulmonary fibrosis B. pneumonia C. atelectasis D. emphysema 10. Functional residual capacity (FRC) may be measured using which of the following techniques? I. helium dilution test II. simple spirometry III. nitrogen washout test A. I only B. I and III only C. II and III only D. I, II and III 137 Answer Key Pulmonary Patient Assessment 1. B 7. B 13. B 19. A 25. A 31. C 37. C 2. C 8. A 14. C 20. C 26. B 32. C 38. B 3. C 9. B 15. A 21. C 27. D 33. D 39. A 4. B 10. B 16. A 22. B 28. B 34. A 40. D 5. A 11. D 17. C 23. D 29. C 35. B 41. B 6. D 12. A 18. D 24. C 30. A 36. B 42. A 43. B 47. B 44. C 48. A. 45. D 49. B 46. D 50. C Oxygen Therapy 1. B 8. B 15. D 22. B 29. B 36. C 2. C 9. D 16. C 23. B 30. C 37. B 3. C 10. A 17. D 24. B 31. A 38. D 4. D 11. D 18. A 25. C 32. D 39. B 5. C 12. C 19. C 26. B 33. C 40. B 6. B 13. C 20. A 27. C 34. C 41. C 7. C 14. A 21. C 28. D 35. C 42. B 43. D 50. C 57. A 64. A 71. C 78. C 44. A 51. D 58. D 65. D 72. B 79. B 45. A 52. C 59. A 66. C 73. C 80. B 46. C 53. B 60. D 67. A 74. A 81. C 47. D 54. B 61. A 68. A 75. D 82. A 48. B 55. B 62. D 69. B 76. B 49. D 56. B 63. B 70. B 77. C Humidity and Aerosol Therapy 1. B 7. C 13. A 19. D 25. B 31. D 2. B 8. C 14. D 20. B 26. A 3. C 9. D 15. C 21. D 27. C 4. D 10. D 16. C 22. D 28. A 5. A 11. B 17. B 23. B 29. B 6. A 12. A 18. A 24. B 30. B 138 Equipment Decontamination/Infection Control 1. A 8. C 15. C 22. B 29. D 36. B 43. D 50. D 2. C 9. B 16. C 23. A 30. B 37. D 44. D 51. B 3. B 10. C 17. B 24. A 31. A 38. B 45. B 52. C 4. D 11. B 18. D 25. D 32. D 39. A 46. B 53. A 5. B 12. A 19. B 26. C 33. D 40. D 47. C 54. B 6. B 13. A 20. B 27. C 34. C 41. A 48. A 55. D 7. B 14. D 21. C 28. B 35. A 42. D 49. B 56. C 57. B 58. A 59. C 60. D 61. C 62. C Management of the Airway 1. B 8. B 15. D 22. B 29. B 2. C 9. D 16. C 23. D 30. C 3. B 10. C 17. A 24. D 31. D 4. A 11. A 18. B 25. B 32. D 5. D 12. A 19. B 26. B 33. D 6. A 13. A 20. B 27. B 34. B 7. C 14. D 21. D 28. A 35. B IPPB/Incentive Spirometry 1. D 8. A 15. B 2. C 9. A 16. B 3. A 10. C 17. B 4. C 11. D 18. C 5. B 12. B 6. C 13. A 7. B 14. B CPR/Manual Resuscitators 1. C 6. B 11. D 16. A 21. A 2. C 7. D 12. B 17. D 22. C 3. D 8. B 13. D 18. C 23. D 4. A 9. D 14. B 19. B 24. C 5. C 10.B 15. D 20. B 25. D 139 ABG Interpretation 1. C 8. B 15. A 22. C 29. B 2. C 9. A 16. D 23. D 30. C 3. A 10. C 17. B 24. B 31. B 4. D 11. C 18. A 25. D 32. B 5. C 12. D 19. B 26. A 6. A 13. B 20. D 27. A 7. B 14. B 21. B 28. C Ventilator Management 1. C 10. A 19. D 28. B 37. A 46. B 55. A 64. D 2. C 11. D 20. C 29. D 38. B 47. B 56. C 65. B 3. A 12. C 21. C 30. B 39. C 48. B 57. A 66. D 4. C 13. D 22. A 31. B 40. B 49. D 58. B 67. C 5. A 14. D 23. A 32. A 41.C 50. D 59. A 68. D 6. D 15. C 24. B 33. B 42. B 51. A 60. D 69. D 7. B 16. C 25. D 34. D 43. C 52. D 61. C 70. B 8. B 17. C 26. B 35. D 44. A 53. B 62. D 71. C 9. B 18. B 27. C 36. C 45. D 54. A 63. A 72. A 73. C 81. C 89. C 74. B 82. C 90. C 75. A 83. D 91. C 76. C 84. C 92. D 77. D 85. B 93. B 78. A 86. A 94. B 79. D 87. A 95. B 80. D 88. B Disorders of the Respiratory System 1. B 6. C 11. B 16. D 21. B 26. D 31. A 2. C 7. D 12. C 17. A 22. C 27. B 32. A 3. A 8. D 13. B 18. D 23. D 28. C 33. D 4. D 9. C 14. A 19. C 24. A 29. B 34. B 5. A 10. A 15. C 20. C 25. A 30. D 35. B Respiratory Medications 1. B 6. B 11. C 16. B 21. D 2. A 7. A 12. A 17. B 22. A 3. D 8. C 13. C 18. A 23. C 4. A 9. B 14. C 19. A 24. B 5. D 10. C 15. D 20. C 25. A Pulmonary Function Testing 1. B 6. A 2. C 7. B 3. C 8. C 4. A 9. D 5. B 10. B 140