ONLINE APPENDIX SUPPLEMENTAL METHODS 22 Participating
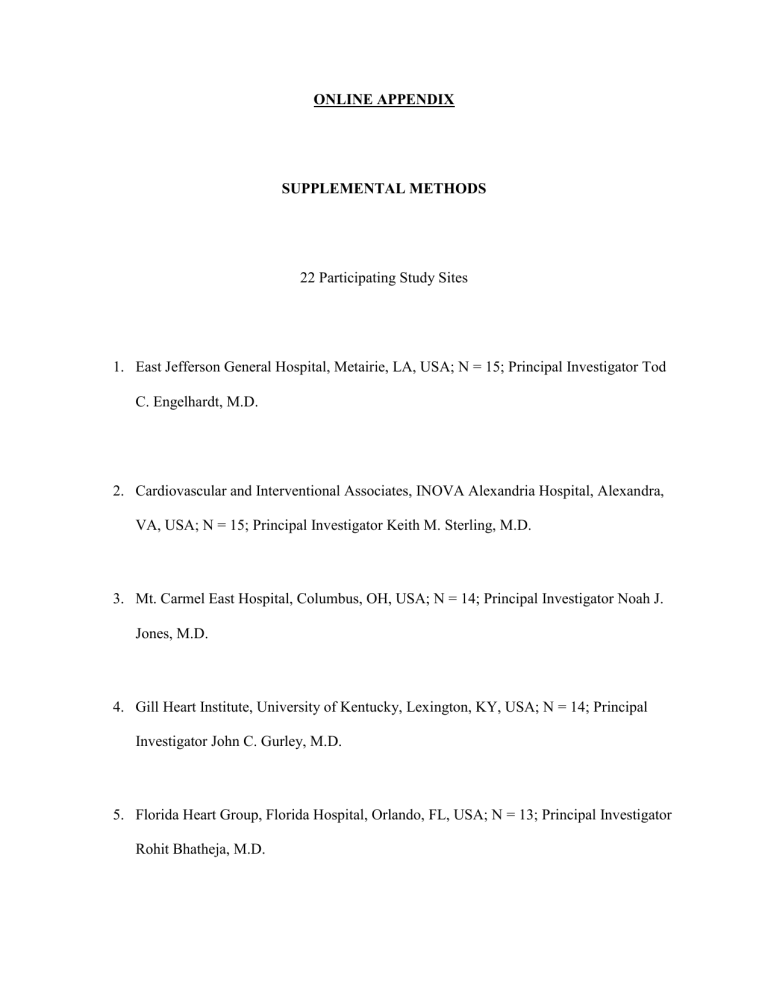
ONLINE APPENDIX
SUPPLEMENTAL METHODS
22 Participating Study Sites
1.
East Jefferson General Hospital, Metairie, LA, USA; N = 15; Principal Investigator Tod
C. Engelhardt, M.D.
2.
Cardiovascular and Interventional Associates, INOVA Alexandria Hospital, Alexandra,
VA, USA; N = 15; Principal Investigator Keith M. Sterling, M.D.
3.
Mt. Carmel East Hospital, Columbus, OH, USA; N = 14; Principal Investigator Noah J.
Jones, M.D.
4.
Gill Heart Institute, University of Kentucky, Lexington, KY, USA; N = 14; Principal
Investigator John C. Gurley, M.D.
5.
Florida Heart Group, Florida Hospital, Orlando, FL, USA; N = 13; Principal Investigator
Rohit Bhatheja, M.D.
6.
Holmes Regional Medical Center, Melbourne, FL, USA; N = 13; Principal Investigator
Robert J. Kennedy, M.D.
7.
Prairie Heart Institute, St. John’s Hospital, Springfield, IL, USA; N = 12; Principal
Investigator Nilesh Goswami, M.D.
8.
St. Vincent Medical Group, Indianapolis, IN, USA; N = 8; Principal Investigator Kannan
Natarajan, M.D.
9.
Holy Name Medical Center, Teaneck, NJ, USA; N = 6; Principal Investigator John
Rundback, M.D.
10.
Vascular Medicine Division, Hartford Hospital, Hartford, CT, USA; N = 6; Principal
Investigator Immad R. Sadiq, M.D.
11.
Lifelink Interventional Center, Memorial Medical Center, Modesto, CA, USA; N = 5;
Principal Investigator Stephen K. Liu, M.D.
12.
River Region Cardiology Associates, Baptist Medical Center, Montgomery, AL, USA; N
= 4; Principal Investigator Narinder Bhalla, M.D.
13.
Orlando Regional Medical Center, Orlando, FL, USA; N = 4; Principal Investigator
Barry S. Weinstock, M.D.
14.
El Paso Cardiology Associates, PA, Providence Memorial Hospital, El Paso, TX, USA;
N = 3; Principal Investigator Laiq Raja, M.D
15.
Montefiore Medical Center, Bronx, NY, USA to Department of Radiology, Division of
Vascular Interventional Radiology, Montefiore Medical Center, Bronx, NY, USA; N = 3;
Principal Investigator Jacob Cynamon, M.D.
16.
Radiology and Imaging Specialists of Lakeland, Lakeland Regional Medical Center,
Lakeland, FL, USA; N = 3; Principal Investigator Fakhir F. Elmasri, M.D.
17.
Christiana Care Center for Heart and Vascular Health, Newark, DE, USA; N = 3;
Principal Investigator Mark J. Garcia M.D.
18.
The Cardiovascular Care Group, Overlook Medical Center, Summit, NJ, USA; N = 3;
Principal Investigator Mark Kumar, M.D.
19.
Macon Cardiovascular Institute, Medical Center of Georgia, Macon, GA, USA; N = 2;
Principal Investigator Juan Ayerdi, M.D.
20.
Miriam Cardiology Inc., The Miriam Hospital, Providence, RI, USA; N = 2; Principal
Investigator Peter Soukas, M.D.
21.
Stanford University, Stanford, CA, USA; N = 1; Principal Investigator William Kuo,
M.D.
22.
El Paso Cardiology Associates, PA, Sierra Medical Hospital, El Paso, TX, USA; N = 1;
Principal Investigator Laiq Raja, M.D
Inclusion Criteria
We included patients with:
1.
Computed tomographic (CT) evidence of proximal pulmonary embolism (PE) (filling defect in at least one main or lobar pulmonary artery),
2.
Age ≥18 years,
3.
PE symptom duration ≤14 days,
4.
Informed consent obtained from subject or a Legally Authorized Representative, AND
5.
Right ventricular (RV)-to-left ventricular (LV) diameter ratio ≥ 0.9 on contrast-enhanced chest CT.
Patients with massive (defined as syncope, systemic arterial hypotension, cardiogenic shock, or resuscitated cardiac arrest) or submassive (defined as a normotensive patient with PE and evidence of RV dysfunction) were eligible for enrollment.
Exclusion Criteria
We excluded patients with:
1.
Stroke or transient ischemic attack, head trauma, or other active intracranial or intraspinal disease within 12 months
2.
Recent (within one month) or active bleeding from a major organ
3.
Hematocrit < 30%
4.
Platelets < 100 thousand/μL
5.
International Normalized Ratio (INR) > 3 on no anticoagulants
6.
Activated partial thromboplastin time (aPTT) > 50 seconds on no anticoagulants
7.
Major surgery within seven days
8.
Serum creatinine > 2 mg/dL
9.
Clinician-determined high-risk for catastrophic bleeding
10.
History of heparin-induced thrombocytopenia (HIT)
11.
Pregnancy
12.
Catheter-based pharmacomechanical therapy for PE within three days of study enrollment
13.
Systolic blood pressure < 80 mmHg despite vasopressor or inotropic support;
14.
Cardiac arrest (including pulseless electrical activity and asystole) requiring active ongoing cardiopulmonary resuscitation
15.
Evidence of irreversible neurological compromise
16.
Life expectancy < 30 days
17.
Use of systemic fibrinolytic therapy or glycoprotein IIb/IIIa antagonists within three days prior to inclusion in the study
18.
Previous enrollment in the current study
Bleeding
Bleeding events were defined according to the Global Use of Strategies to Open Occluded
Coronary Arteries (GUSTO) classification (1) for severe or life-threatening, moderate, or mild bleeding:
Severe or life-threatening Either intracranial hemorrhage or bleeding that causes hemodynamic compromise and requires intervention
Moderate Bleeding that requires blood transfusion but does not result in hemodynamic compromise
Mild Bleeding that does not meet criteria for either severe/life-threatening or moderate bleeding
ONLINE REFERENCE
1. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators. N Engl J Med . 1993;329:673-682.