RESPIRATORY PHYSIOLOGY - Angelo State University
advertisement

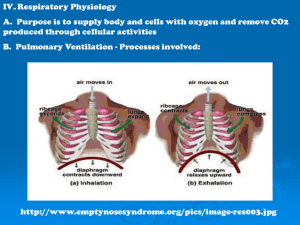
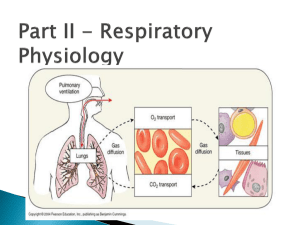
1 RESPIRATORY PHYSIOLOGY MECHANICS OF BREATHING: Pressure Considerations: 1. Air tends to move from a region of higher pressure to a region of lower pressure, that is, down a pressure gradient. 2. Air flows in and out of the lungs during the act of breathing by moving down pressure gradients that alternate between the inside of the body and the outside the body. Always from H to L. To breathe in: High pressure outside, Low inside, air flows in. To breathe out: High pressure inside, Low outside, air flows out. Air flow pressure gradients are established by by cyclical respiratory muscle activity of the diaphragm and intercostal muscles, abdominal muscles, the natural elasticity of the lungs, pleural fluid (adhere lungs to the thorax wall), and absorption of gases in the alveoli, and the surface tension of the alveoli. Atmospheric Pressure: 1. 2. 3. Is the pressure exerted by the weight of the air in the atmosphere on objects on the earth’s surface (pressure exerted by the gases of the atmosphere). Composed of about 79% N, 21% O2, 0.04% CO2, 0.46% H2O, and other inert gases. At sea level this pressure is equal to 760 mmHg, the pressure exerted by a column of mercury 760mm high. Atmospheric pressure decreases with increasing altitude above sea level and increases. Atmospheric pressure increases with decreasing depth below sea level. Intra-alveolar/Intrapulmonary Pressure: is the pressure within the alveoli. 1. It rises and falls with the phases of breathing, but it always equalizes itself with the atmospheric pressure outside the body. Intrapleural Pressure: is the pressure within the pleural sac containing the lungs. Pressure exerted outside the lungs within the thoracic cavity. 1. It is always 4mm Hg less than the pressure in the alveoli and the atmospheric pressure, so a greater pressure is pushing outward than is pushing inward across the lung wall. 2. This pressure difference that exists across the lungs, holds the lungs tightly to the thoracic wall and allows them to expand and contract = transmural pressure. PULMONARY VENTILATION: 1. 2. 3. 4. 5. 6. 7. Pulmonary ventilation, or breathing, is a completely mechanical process that depends on volume changes occurring in the thoracic cavity. A rule to keep in mind throughout the following discussion is: Volume changes lead to pressure changes, which lead to flow of gases to equalize the pressure. Because air flows down a pressure gradient, the intra-alveolar pressure must be less than atmospheric pressure for air to flow into the lungs during inspiration. Similarly, the intra-alveolar pressure must be greater than the atmospheric pressure for air to flow out of the lungs during expiration. Intra-alveolar pressure can be changed by altering the volume of the lungs. The relationship between the pressure and volume of gases is given by Boyle's Law, which states that under conditions of constant temp., their pressure of a gas varies inversely with its volume. • Gases like liquids, conform to the shape of their container, however, unlike liquids, gases fill their container. • Therefore in a large volume, the gas molecules will be far apart and the pressure will be low. • If the volume is reduced, the gas molecules will be closer together and the pressure will rise. The respiratory muscles that accomplish breathing do not act directly on the lungs to change their volume. Instead, these muscles change the volume of the thoracic cavity, causing a corresponding change in lung volume because the thoracic wall and lungs are linked together by the transmural pressure gradient. 2 INSPIRATION: • • • 1. 2. 3. 4. 5. Visualize the thoracic cavity as a box with a tube attached (trachea). The volume of this box is changeable and can be increased by enlarging all of its diameters, thereby decreasing the gas pressure within it. This in turn, will result in air rushing into the box from the atmosphere, since gases always flow along their pressure gradients Analogous to normal quiet respiration. When the dome-shaped diaphragm contracts, it move inferiorly and flattens out. As a result the vertical diameter (height) of the thoracic cavity increases. Contraction of the external intercostals results in an elevation of the rib cage and in a thrusting forward of the sternum. The ribs also swing outward (much like t he action that occurs when a curved bucket handle is raised), expanding the diameter of the thorax both laterally and in the anteroposterior plane. These muscle contractions result in the increase of the volume of the thoracic cavity by almost 1/2 a liter, which is the usual volume of air that enters the lungs. Because the lungs are anchored to the thorax wall, they are stretched and the intrapulmonary volume also increases as the thoracic dimensions increase. • As a result, intrapulmonary volume increases while its pressure drops to -1 to -3mm Hg from 760 mmHg to 757 mmHg relative to atmospheric pressure (760 mm Hg). • Intrapleural pressure declines 6-8mm Hg as its volume increases. • And Air rushes into the lungs along this pressure gradient from H to L until the intrapulmonary and atmospheric pressures become equal. During deep or forced Inspiration, the capacity of the thorax is increased maximally by the activation of accessory muscles. • These muscles raise the ribs even more than in quiet respiration. • Include the sternocleidomastoid, pectorals, and scalenes. • Additionally, the back is extended as the thoracic curvature is straightened by contraction of the erector spinae muscles. EXPIRATION: 1. Quiet expiration in healthy individuals is chiefly a passive process that depends more on the natural elasticity of the lungs than on muscular contraction. • As the inspiratory muscles relax and resume their initial resting length, the lungs recoil. • Thus both the thoracic and intrapulmonary volumes decrease at the same time. • This compresses the alveoli, and the intrapulmonary pressure rises to 1-3 mmHg above atmospheric pressure (763 mmHg), which results in an outflow of gases from the lungs. 2. In contrast, forced expiration is an active process produced by contraction of abdominal wall muscles, primarily the oblique and transverse abdominals. These contractions: • Increase the intra-abdominal pressure, which forces the abdominal organs superiorly against the diaphragm and, • Depress the rib cage. • The internal intercostal mujscle and latissimus dorsi muscles of the back may also contribute to enhance rib cage depression. • It is interesting that the ability of a trained vocalist or instrumentalist (brass and wind) to hold a particular note depends on the coordinated activity of several muscles normally used in force expiration. • Thus, muscle control of expiration is very important during speaking, singing, or playing an instrument when a precise regulation of airflow from the lungs is desired. You have learned that during the respiratory cycle that: The lungs alternately expand during inspiration and recoil during expiration. What properties of the lungs enable them to behave like balloons, able to be stretched and then snapping back to their resting position when the stretching forces are removed? 1. 2. Elastic Recoil: this refers to how readily the lungs rebound after having been stretched. It is responsible for the lungs returning to their pre-inspiratory volume when the inspiratory muscles relax at the end of inspiration. Due to elastic connective tissue. Compliance: refers to how much effort is required to stretch or distend the lungs; it is analogous to how hard you have to work to blow up a balloon. (By comparison, 100 times more distending pressure is required to inflate a child’s toy balloon than to inflate the lungs. The ease with which the lungs an be expanded, that is their distensibility. Specifically, compliance is a measure of the magnitude of change in lung volume accomplished by a given change in the transmural pressure gradient, the force that stretches the lungs. The lower the compliance of the lungs, the larger the transmural pressure gradient that must be created during inspiration to produce normal lung expansion. 3 Compliance is diminished by any factor that (1) reduces the natural resilience of the lungs, such as fibrosis, (2) blocks the bronchi or smaller respiratory, since this reduces alveolar ventilation, or (3) impairs the flexibility of the thoracic cage. Can be causes by: ossification of costal cartilages (old age), paralysis of the intercostal muscles because they hinder thoracic expansion. GAS EXCHANGE: Introduction: 1. The ultimate purpose of breathing is to provide a continual supply of fresh O 2 for pickup by the blood and to constantly remove CO2 unloaded from the blood (Products of cellular respiration). The blood acts as a transport system for O2 and CO2 between the lungs and tissues, with the tissue cells extracting O2 from the blood and eliminating CO2 into it. 2. Gas exchange at both the pulmonary capillary and tissue capillary levels involves simple passive diffusion of O2 and CO2 down partial pressure gradients (H L) There are no active transport mechanisms for these gases. Remember occurs at the alveolar level Occurs during inspiration and expiration. 3. Let’s see what partial pressure gradients are and how they are established. Atmospheric Air is a mixture of gases that contains 79% nitrogen and 21% oxygen, and almost negligible amounts of CO 2, H2O, other gases, and pollutants. 1. 2. 3. 4. 5. The total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture. Further, the pressure exerted by each gas, its partial pressure is directly proportional to its percentage in the total gas mixture. Every gas molecule, no matter what its size, exerts the same amount of pressure. N2 exerts same amount of pressure as O2. Gases dissolved in liquid or plasma also exert a partial pressure. When a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure and its solubility in the liquid. When equilibrium is achieved, the gas partial pressure in both phases is equal. CO2 is most soluble in plasma, with a solubility coeff. of 0.57 O2 is least soluble in plasma, with a solubility coeff. of 0.012 Partial Pressure gradients: 1. The PO2 of pulmonary blood = 40 mmHg, The PO2 in alveoli = 104 mmHg. Est. a large pressure gradient and O2 diffuses rapidly from the alveoli into the pulmonary capillary blood. Equilibrium occurs in 0.25s. Note the alveolar walls are very thin. Alveoli have a large surface area. 2. CO2 moves in the opposite direction along a much less steep partial pressure gradient of about 5 mmHg (45mmHg to 40mmHg). Notice that even though the pressure gradient for oxygen is much steeper than that for CO2, equal amounts of these gases are exchanged because carbon dioxide solubility in plasma and alveolar fluid is 20 times greater than that of O2. 3. The factors promoting gas exchanges between the systemic capillaries and the tissue cells are essentially identical to those acting in the lungs. AS the tissue cells continuously use oxygen for their metabolic activities, they produce equal amount so carbon dioxide (cellular respiration). The PO2 in the tissues is always lower than that in the systemic arterial blood (40 vs. 104 mmHg). Consequently oxygen moves rapidly from the blood into the tissues until equilibrium is reached, and carbon dioxide moves quickly along it partial pressure gradient into the blood. As a result, venous blood draining the capillary beds of the tissues and returning to the heart has a PO 2 of 40 mmHg and a PCO2 of 45mmHg. In SUMMARY: The gas exchanges that occur between the blood and the alveoli on the one hand and between the blood and the tissue cells on the other take place by simple diffusion and depend on partial pressure gradients of oxygen and carbon dioxide that exist on the opposite side of the exchange membranes. OXYGEN TRANSPORT: 1. Since only about 1.5% of the body’s oxygen is carried dissolved in plasma, the RBC’s and hemoglobin function to carry oxygen to the tissues. 2. O2 molecules bind to the 1 of 4 polypeptide chains in the Hb molecule 1-3 molecules are bound = partially saturated 4 = fully saturated 3. Unloading and loading of O2 from Hb are affected by PO2 , temp, and 2,3-DPG (diphosphoglycerate) enhances release. 4 CARBON DIOXIDE TRANSPORT: 1. CO2 is transported dissolved in the plasma (7-8%) , chemically bound to Hb (20%), and (primarily) as the bicarbonate ion (HCO3-) in plasma (70%). When release from tissues into the blood, CO2 enters into the plasma and the RBC’s When combined with Hb forms carbmino hemoglobin. When combined with water, CO2 forms carbonic acid (H2CO3), which quickly dissociates into HCO3- and H+. Reaction occurs in the plasma and is facilitated by carbonic anhydrase (enzyme) in RBC’s, HCO3 then diffuses to plasma by chloride shift = Chlorine ion rush in to RBC’s to counter act the net positive charge left by the negative outward flux of HCO3-. Carried to Lungs where process is reversed, HCO3 reenters RBC’s and bind with hydrogen ion to form carbonic acid, which is then split by carbonic anhydrase to release CO2 and H2O. CO2 then diffuses along its partial pressure gradient from the blood into the alveoli. CONTROL OF RESPIRATION: 1. 2. 3. The pace setter of respiratory rhythm is the inspiratory center (nuclei = dorsal respiratory group) in the medulla oblongata. When firing, stimulates diaphragm and external intercostals via the phrenic nerve and intercostal nerves. When not firing, allows them to relax. 12-15 breaths/min = normal. Can be suppressed completely by alcohol, sleeping pills, or morphine. The expiratory center stimulates inspiratory muscles and expiratory muscles. It maintains the inspiratory muscles in a state of partial contraction during normal quiet breathing When the demand for oxygen is increased (exercise) it does stimulate the inspiratory muscles, but stimulates abdominal and internal intercostals to promote vigorous ventilation. The pons produces smooth transitions from inspiration to expiration, and vice versa, if connection to medulla is severed breaths become abnormal and occur in gasps. pneumotaxic center transmits inhibitory impulses to the inspiratory center of the medulla. It fine tunes breathing and prevents lung over-inflation, cuts off inspiration. apneustic center provides inspriatory drive by continuously stimulating the medullary inspiratory center. It prolongs inspiration or to cause breath holding in the inspiratory phase. Factors Influencing the Rate and Depth of Breathing: Intro: Both the depth and rate of breathing can be modified in response to changing body demands. Both the medulla and pons are sensitive to many different stimuli, some excitatory, some inhibitory. Hering-Breuer Reflex: 1. Stretch receptors in the visceral pleurae and conducting passages in the lungs are stimulated when the lungs become over-inflated and excessively stretched. Inhibitory impulses are then sent to the medullary inspiratory center and to the apneustic center of the pons, allowing expiration to occur. Thought to be a protective mechanism rather than an important regulator or normal respiration. Hypothalamic Controls: 1. Strong emotions and pain acting through the limbic system of the brain activate hypothalamic sympathetic nervous system centers which can send modulation signal to the respiratory centers. EX: Gasping when exposed to cold water: EX: Gasping when frightened. Cortical Controls: 1. Although breathing is normally regulated involuntarily by brain stem centers, connections between the cortical centers and the brains stem allow us to consciously alter our pattern of respiration. During swallowing, singing, talking, etc... breath control is extremely important. However, voluntary controls of breathing are limited, and the respiratory centers will simply ignore messages from the cortex and will escape from voluntary controls when the PCO2 in the blood reaches certain critical levels. As a result breathing resumes automatically. EX: Child holding his breath! Chemical Factors: 5 1. 2. Although many factor can modify the baseline respiratory rate and depth, the most important factors are changing levels of carbon dioxide, oxygen, and hydrogen ions in the arterial blood. Sensor responding to such chemical fluctuations, called chemoreceptors, are found in 2 major body locations: The central chemoreceptors are located in the medulla; the peripheral chemoreceptors are found within the great vessels of the neck. Influence of PCO2: 1. Although every cell in the body must have oxygen to live, the body’s need to rid itself of CO 2 is the most important stimulus for breathing in a healthy person. 2. Rising CO2 partial pressures are the most powerful respiratory stimulant. As CO2 is hydrated in CSF (carbonic acids dissociates giving off H+), liberated H+ acts directly on the central receptors causing a reflexive increase in breathing rate and depth. Low CO2 levels depress ventilation: EX hyperventilating before swimming underwater. Influence of PO2: 1. The main O2 sensors are found in the carotid bodies. 2. Under normal conditions, the effect of declining PO2 on alveolar ventilation is very slight and mostly limited to enhancing the sensitivity of central receptors to CO 2. Arterial PO2 must drop substantially before oxygen levels become a major stimulus for increased ventilation. Why? Huge reservoir of O2 bound to Hb and Hb remains almost entirely saturated with oxygen unless or until the PO2 of alveolar gas and arterial blood fall to 60mmHg or below. 3. When arterial PO2 drops below 60 mmHg, it becomes the major stimulus for respiration, and ventilation is increased via reflexes initiated by peripheral chemoreceptor activation. Changes in arterial pH resulting from CO2 retention or metabolic factors act indirectly through the peripheral chemoreceptors to promote changes in ventilation, which in turn modify arterial PCO2 and pH. EFFECTS OF HEIGHTS AND DEPTHS ON THE BODY: 1. 2. At high altitudes, where the atmosphere is less influenced by gravitational pull, all partial pressure values of gases in the atmosphere decline in direct proportion to the decline in atmospheric pressure. 18000ft (PO2 drops from 159 mmHg at sea level to 80mmHg). Below sea level atmospheric pressure increases by 1 atmosphere for each 33ft. of descent. Thus at 99 feet below sea level, the total pressure on the body is equivalent to 3 atmospheres, or 2280mmHg. High Altitudes: 1. At high altitudes, the lower PO2 which causes less oxygen available to be loaded and resultant lower than normal Hb saturation levels. It is not because there is less oxygen available. All gases exist in the same proportion at all atmospheres. 2. Above 10,000ft (ascended rapidly) Causes hyperventilation and Hypoxia (inadequate O2 at cellular level). Experience dizziness, fatigue, nausea, loss of appetite, rapid heart rate, ultimately nerve dysfunction, characterized by poor judgment, and uncoordination. Acute mountain sickness. 3. Can become acclimatized to these conditions, by increased RBC production which increase the O2 carrying capacity of the blood, O2 is also unloaded easier by increased production of DPG, increased capillary production. Can be dangerous = polycythemia Low Altitudes (Below sea level). 1. Recall that below sea level atmospheric pressure increases by 1 atmosphere for each 33ft. of descent. Thus at 99 feet below sea level, the total pressure on the body is equivalent to 3 atmospheres, or 2280mmHg. 2. Divers use a combination of gases to breathe under water (increase levels of O 2 can be toxic). 3. Although N2 accounts for nearly 80% of the gases in air, it ordinarily has little effect on body functions because it is so insoluble in blood. 4. However, when a deep-sea diver breathes under high pressure conditions, the partial pressure of all gases in the mixture increase dramatically As a result, much more N gas is forced into solution in the blood and causes nitrogen narcosis= believed to be caused by a reduction in the excitability of neurons due to the highly lipid soluble N 2 dissolving in their lipid membranes At 150 ft divers experience a feeling of euphoria, giddiness and become drowsy (like drink “buzz”). At lower depths divers become weak and clumsy, and at 350-400 ft lose consciousness Because of this it is also called rapture of the deep. 6 5. As long as a diver ascends to the surface gradually or by gradual decompression in decompression, dissolved N2 gas can be eliminated by the lungs without problems. But if ascent is rapid, the PN2 decreases abruptly, and the poorly soluble N2 gas appears to boil out of solution in the body fluids forming large gas bubbles = decompression sickness or bends the latter because the person “bends” over in pain. Gas bubbles in blood represent life-threatening emboli, and those formed within tissues can causes excruciating pain and may impair the normal function of any organ, including the brain. “Benefits of Smoking” 1. emphysema 2. lung fibrosis 3. chronic bronchitis 4. lung cancer 5. physical deformity 6. excessive mucous production 7. chronic coughing 8. cyanosis blue throat