Intra-operative and functional results of robotic
advertisement

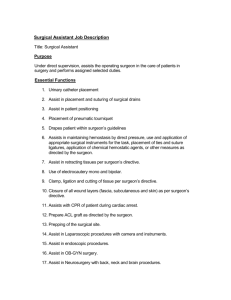
Intra-operative and functional results of robotic-assisted laparoscopic radical prostatectomy. Comparison of surgeons with different operative backgrounds Introduction & Objectives Robot-assisted laparoscopic radical prostatectomy (RALP) has gained increasing popularity in the latest years. Despite great interest, only few data is available on the impact of previous surgical background on the learning curve for the robotic approach. We hypothesized that the surgeon background (previous open or laparoscopic experience) may affect the intraoperative and functional results after RALP. Material & Methods The study included 354 consecutive patients treated with RALP between 2007 and 2010 at a single tertiary care referral center by 3 experienced surgeons. All patients had detailed data including PSA, clinical stage, biopsy Gleason sum, preoperative erectile function (EF) assessed by means of the IIEF and surgical margin (SM) status. Patients were divided into 2 pre-operative risk groups: low (PSA<10 ng/ml,cT1,biopsy Gleason sum ≤6) and intermediate risk (all the remaining patients). Patients at high risk high (cT3 or biopsy Gleason 8-10 or PSA >20 ng/ml) were excluded from the analyses. Patients were stratified according to surgical background of the operator: purely laparoscopic (Lap; n=82); purely open (Open; n=89) and mixed (Mixed; n=183).Logistic regression models were performed to evaluate the association between surgeon background and presence of positive SM at final pathology. Cox regression models tested the association between surgeon background and the rate of EF and urinary continence (UC) recovery after Rapport-op UC recovery was defined as the absence of any protection device (no pads), while EF recovery was defined as IIEF-EF≥22. Results The 3 groups did not differ in terms of age at surgery (p=0.5) and rate of patients with low and intermediate risk (p=0.2).Pre-op IIEF was significantly lower in the group of Mixed experience (p=0.008).The mean operative time was higher for the group of mixed experience (295 vs. 252 vs. 275 minutes for Mixed vs. Lap vs. Open, p=0.03). No differences in terms of number of nodes removed was noted between the groups (p=0.12) while blood loss was significantly higher in patients treated by the surgeon with Open experience (370 vs. 261 vs. 434cc for Mixed vs. Lap vs. Open, p<0.001). However, no difference was noted in terms of positive SM (20.3 vs. 31.7 vs. 21.3% for Mixed vs. Lap vs. Open, p=0.11).Post-op hospital stay was lower for the group treated by the Open surgeon (7.0 vs. 6.1 vs. 5.5 days for Mixed vs. Lap vs. Open, p<0.001). At multivariable analyses, after adjusting for pre-operative risk group and PSA values, the surgeon background did not impact on the rate of positive SM (p=0.1).Similarly, surgeon background was not a predictor of EF (p=0.8) and UC (p=0.4) recovery. Conclusions Surgeon background does not impact on either surgical margins or functional outcome of patients treated with RALP. These results need to be validated in larger series with longer follow-up.