Benign Paroxysmal Positional Vertigo (BPPV)
advertisement

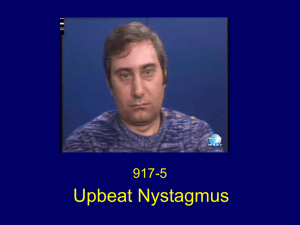
Benign Paroxysmal Positional Vertigo (BPPV) Diagnostic Worksheet Dolores Umapathy dolores.umapathy@bolton.nhs.uk Endorsed by BAAP Audit group Clinical Features BPPV is a benign inner ear condition. It is generally sudden in onset with paroxysmal and positional symptoms triggered by head position. The main symptom is vertigo having the following features 1) Triggered by rapid change in head position-characteristically lying down/turning in bed, sitting up from supine, bending over and neck extension 2) Duration usually few seconds to rarely over a minute 3) Latent period prior to onset of symptoms in provoking position generally between 1 and 40 seconds 4) Vertigo is described generally as being intense and brief, with a complaint of light headedness and imbalance persisting for a short duration with a few complaining of the symptoms persisting for several days after the vertigo 5) Nystagmus may be described by others but patient is usually unaware of it 6) Often associated with autonomic symptoms like nausea and sweating. Vomiting is rare. Diarrhoea is less common 7) In between attacks there may be no symptoms if there is no other vestibular pathology 8) Clusters of attacks may last for a couple of days upto several months Diagnosis –Hallpike Manoeuvre Before Manoeuvre Explain procedure and possible side effects such as temporary dizziness. Sit patient on couch such that when lying down the shoulders will be level with end of couch. Instruct patient to fix eyes on a point directly in front (eg. Clinician’s forehead). Start with the affected ear Absolute Contraindications Musculo-skeletal: Recent history of neck surgery, recent vertebral disc prolapse, cervical spine fracture or trauma particularly if it restricts rotation or extension of neck, Instability of atlanto-axial and occipito-atlantal joints Neurological: Cervical myelopathy or radiculopathy Vascular: Dissection of carotid or vertebral artery Nb: A history of posterior circulation ischaemia or a neck bruit is not an absolute contraindication. Caution exercised in following conditions: Cervical involvement of Rheumatoid arthritis, carotid sinus hypersensitivity, cardiac surgery within 3 months, severe back pain, severe orthopnoea Technique Hold patient’s head in both hands and turn 450 towards the test ear. Support neck and maintaining torsion along with fixed gaze, move head rapidly backwards to head hanging position, 30 – 450 (optimally) below horizontal as rapidly as possible. Maintain the head hanging position for 30 –60 seconds and observe patient’s eyes. If nystagmus is present note the latent period, magnitude and direction of rotation of the fast phase. Maintain position for about 1 minute after onset to determine if nystagmus adapts, changes direction or alters. Return patient to upright position while maintaining 450 neck rotation and observe for reversal of nystagmus. Wait till patient is settled and then repeat on same side to assess fatigability. Proceed to opposite side if no nystagmus is seen on the first side or when the patient has settled from the first test. Positive response Posterior canal BPPV is the commonest and the type of nystagmus seen would indicate the canal involved Posterior canal BPPV: Geotropic torsional nystagmus (towards undermost ear) Anterior canal BPPV: Geotropic torsional nystagmus with downbeat component Horizontal canal BPPV: Horizontal nystagmus (geotropic if canalithiasis, ageotropic if cupulolithiasis) Nb: Hallpike test is not the ideal test of horizontal canal BPPV Modification to the Hallpike Test Anterior canal BPPV can sometimes be better elucidated by making the patient lie supine with the head extended in the primary position i.e. straight back or ‘Rose’ position. Torsional nystagmus with a major downbeat component is seen. The side is indicated by the torsional element beating towards the affected side Horizontal BPPV is best seen on the roll test. The patient is made to lie on a couch with the head position raised to 300(Caloric position). The head is then rolled quickly from one side to the other. Horizontal nystagmus is seen on both sides but the side in which the nystagmus is more marked determines the side affected. Differential Diagnosis Main differential diagnosis is from a central positional nystagmus where the nystagmus is usually downbeat but could be in any direction and there is no latency, adaptability or fatigability. Vertigo is generally absent or mild. Investigations No investigations are generally required unless other co-existing vestibular or audiological pathology is suspected. Video-oculography can be used to document the nystagmus for teaching or research purposes. References 1. Baloh RW, Honrubia V, Jacobson K; Benign Positional Vertigo: clnical and oculographic features in 240 cases. Neurol 1987; 37: 371-8 2. Honrubia V, Baloh RW, Harris MR, Jacobson KM. Paroxysmal Positional Vertigo Syndrome. Am J Otology 1999. 20: 465-470 3. Norre ME. Diagnostic problems in patients with Benign Paroxysmal Positional Vertigo. Laryngoscope 1994, 104, 11: 1385- 1389 4. Steddin S, Brandt T. Unilateral mimicking bilateral Benign Paroxysmal Positional Vertigo. Arch Otolaryngol Head Neck Surg. 1994;120: 1339-1341. 5. Smouha EE, Roussos C. Atypical forms of paroxysmal positional nystagmus. Ear Nose Throat Journal 1995,74, (9), pp649-656 6. Pollak l, Davies RA, Luxon LM. Effectiveness of the particle repositioning manoeuvre in benign paroxysmal positional vertigo with and without additional vestibular pathology. 7. Bertholon P, Bronstein AM, Davies RA, Rudge P, Thilo KV. Positional downbeating nystagmus in 50 patients: Cerebellar disorders and possible anterion semicircular canal lithiasis. J Neurol Neurosurg Psychiatry. 2002; 72: 366-372 8. Dix R, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann otol Rhinol Laryngol. 1952;6 987-1016 9. Barany R: diagnose von Krankheitserscheinungen im Bereiche des otolithenapparates. Acta otolaryngol (Stockh) 2:434-437, 1921