Module_3_Evaluation
advertisement
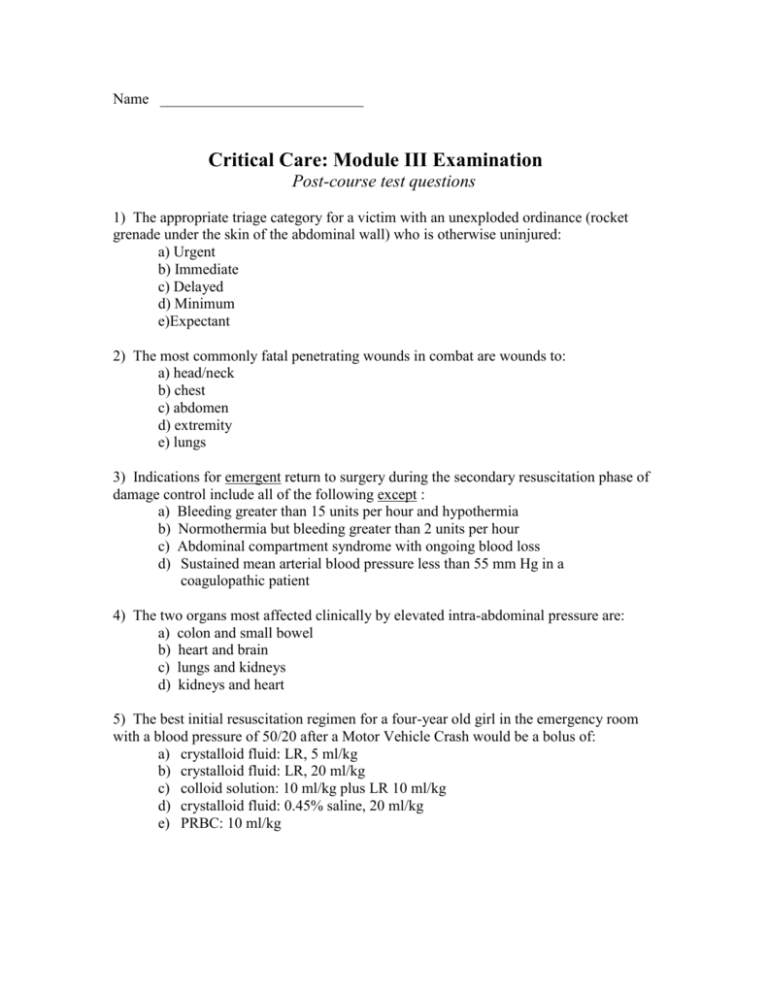
Name ___________________________ Critical Care: Module III Examination Post-course test questions 1) The appropriate triage category for a victim with an unexploded ordinance (rocket grenade under the skin of the abdominal wall) who is otherwise uninjured: a) Urgent b) Immediate c) Delayed d) Minimum e)Expectant 2) The most commonly fatal penetrating wounds in combat are wounds to: a) head/neck b) chest c) abdomen d) extremity e) lungs 3) Indications for emergent return to surgery during the secondary resuscitation phase of damage control include all of the following except : a) Bleeding greater than 15 units per hour and hypothermia b) Normothermia but bleeding greater than 2 units per hour c) Abdominal compartment syndrome with ongoing blood loss d) Sustained mean arterial blood pressure less than 55 mm Hg in a coagulopathic patient 4) The two organs most affected clinically by elevated intra-abdominal pressure are: a) colon and small bowel b) heart and brain c) lungs and kidneys d) kidneys and heart 5) The best initial resuscitation regimen for a four-year old girl in the emergency room with a blood pressure of 50/20 after a Motor Vehicle Crash would be a bolus of: a) crystalloid fluid: LR, 5 ml/kg b) crystalloid fluid: LR, 20 ml/kg c) colloid solution: 10 ml/kg plus LR 10 ml/kg d) crystalloid fluid: 0.45% saline, 20 ml/kg e) PRBC: 10 ml/kg 6) With regards to the clinical implications of shock, which of the following is NOT correct: a. Tachycardia and a narrowed pulse pressure may be the first signs of significant blood loss. b. Patients who only transiently improve with 2L of initial crystalloid resuscitation are likely to require blood transfusion and may need operative control of hemorrhage. c. Colloid resuscitation has consistently been shown to be superior to crystalloid. d. Shock is a clinical condition marked by inadequate organ perfusion and tissue oxygenation. 7) A patient is brought from the battlefield. He is yelling inappropriately and thrashing on the stretcher. He opens his eyes only when he is stimulated by pain but will reach for the painful stimulus. He does not follow any commands. What is his GCS? a. 5 b. 7 c. 10 d. 13 8) All of the following statements are true except: a. Burr holes are primarily used to evacuate acute subdural hematomas b. Brain abscess is a complication of penetrating head injury c. Hypoxia and hypotension in head injury are associated with a poorer outcome d. Hemotympanum is a sign of a basilar skull fracture 9) Eyelid tissue which appears devitalized should be debrided before repair: a) always b) sometimes c) never 10) A patient with unilateral, penetrating eye trauma receives the following Air-Evac priority during wartime: a) this issue is not addressed in the NATO manual b) this issue is addressed in the NATO manual c) eye trauma ranks right after preservation of life and limb in priority d) b and c are correct e) a and c are correct 11) Correct statements regarding oromaxillofacial trauma include: a. Associated CNS injury is rare. b. Prompt NG tube placement is required to prevent aspiration. c. Extensive facial lacerations require a Plastic Surgeon’s expertise for management d. Tamponade is an effective means for controlling hemorrhage. 12) Mandibular fractures: a. May result in airway compromise b. Should be treated in the field with open reduction / internal fixation c. Should be considered a true emergency d. Usually involve a single fracture site 13) Drains for esophageal injury: a. Should not be necessary with proper technique b. Should be removed as soon as the output is below 20cc c. Should not be removed until a swallow study is negative for a leak and no drain output occurs with oral intake d. Are only necessary when combined injuries are present 14) Laryngeal injury: a. Rarely requires a surgical airway b. Can be managed safely with standard orotracheal intubation in almost all instances c. Is asymptomatic in 50% d. Can be temporized with jet insufflation 15) The earliest and therefore the most important finding in patients with a compartment syndrome is a. Paresthesia b. Paralysis c. Pulselessness d. Pain out of proportion to injury 16) The appropriate location for a bridging knee external fixator is a. Lateral b. Anterior c. Medial d. External fixators should never cross a joint 17) Techniques to be used for splenic preservation include all of the following except: a) coagulation b) suture c) lobar artery ligation d) absorbable mesh wrapping e) autotransplantation 18) Active duty personnel who require trauma splenectomy do not need special vaccination because of the military vaccination program. a) true b) false 19) If the packing technique is utilized for a case of liver trauma, the packs must be removed within 24 hours in order to avoid sepsis: a) true b) false 20) Recent studies of colonic trauma have shown: a. Despite earlier work, intra-abdominal suture line dehiscence is shown to be a significant problem when primary resection and repair is attempted. b. Although primary repair in academic trauma centers has had success, even selective repair in field settings is doomed to failure. c. Five days of prophylactic antibiotic coverage has been shown to be superior to 24 hours. d. Intra-abdominal complications are not increased in patients who undergo primary colonic repair. 21) In blunt trauma to a hollow viscus: a. Associated injuries to the spine, aorta, or solid organs are very common. b. “Blow-out” injuries can almost always be repaired with direct suture closure; resection and anastomosis is rarely indicated. c. Serosal tears mandate resection regardless of whether the underlying mucosa is disrupted. d. Mesenteric injury is not often seen in conjunction with blunt injury to the bowel. 22) The most commonly injured portion of the duodenum is? a. 1st b. 2nd c. 3rd d. 4th 23) A circumferential duodenal laceration of the 3rd portion is best repaired how? a. resection with end to end anastomosis b. Whipple resection c. duodeno-jejunostomy d. pyloric exclusion 24) The best clinical guide for resuscitating a patient with thermal injury is: a. Lactated Ringer’s at 4 ml/kg/% total body surface area burn (Parkland Formula) b. Lactated Ringer’s at 8 ml/kg/% total body surface area burn (Lentz Formula) c. Lactated Ringer’s at 2 ml/kg/% total body surface area burn (Brooke Formula) d. Administration of Lactated Ringer’s to achieve a urine output of 30 - 50 ml/hour (Next 2 questions) A driver of an armored personnel carrier hits a land mine and sustains deep burns to his head, neck, chest and back and both arms and hands. He arrives screaming after a prolonged extrication. He has singed nasal hair and is hoarse. 25) The first step in the initial management of this patient is: a. Check a carboxyhemoglobin level b. Start I.V. LR at about 1000 - 1500 ml/ hour c. Perform arm escharotomies d. Intubate the patient 26) The patient is on mechanical ventilation for 4 hours and develops sudden respiratory distress. He has a RR of 30 and elevated airway pressures. Initial management includes all of the following. 1) Check endotracheal tube position 2) Obtain a chest x-ray 3) Perform pulmonary toilet maneuvers 4) Perform chest wall escharotomies. a. 1, 2, 3 b. 2 and 4 c. 4 only d. all of the above 27) Vascular access in the hemodynamically unstable pediatric blunt trauma patient is best handled by: 1. limiting peripheral percutaneous attempts to 60 seconds. 2. placement of an intraosseous device in the proximal tibia. 3. placement of a saphenous vein catheter by performance of a cutdown procedure in the groin. 4. immediate insertion of a subclavian trauma catheter using the Seldinger technique. a. 1, 2, and 3 are correct b. 1 and 3 are correct c. 2 and 4 are correct d. only 4 is correct e. all are correct 28) Important anatomic/physiologic differences between the adult and pediatric trauma patient include: 1. a child’s mediastinum and retroperitonum are more mobile than in an adult. 2. pediatric trauma patients show hemodynamic signs of acute blood loss earlier than their adult counterparts 3. major blunt force is more likely to produce internal thoracic or abdominal injuries without skeletal fracture in the child compared to the adult. 4. the child’s bladder is almost entirely extraperitoneal, which lends to a higher rate of successful conservative management of bladder injuries in children when compared to adults. a. 1, 2, and 3 are correct b. 1 and 3 are correct c. 2 and 4 are correct d. only 4 is correct e. all are correct 29) Concerning extraperitoneal bladder injuries . . . a. One may treat the injury non-operatively provided adequate bladder drainage is maintained. b. A one shot cystogram is adequate to rule out the injury. c. They are managed in the same manner as intraperitoneal injuries. d. These are typically seen in a patient who has a full bladder and sustains blunt abdominal trauma. 30) A patient has a mid-ureteral injury from penetrating trauma from a high velocity projectile. You are in a battlefield scenario. He has a large liver laceration and a colon injury. Acceptable methods of initial surgical management include all of the following, EXCEPT... a. Temporary cutaneous ureterostomy and ureteral stenting b. Ureteral ligation c. Transureteroureterostomy d. Tension-free spatulated repair with stenting and retroperitoneal drainage 31) Regarding abdominal primary blast injuries, the following are true: 1) The hollow organs are the most susceptible to primary blast injury 2) Solid abdominal organ (liver/spleen) injuries are more often caused by primary blast effect than by secondary and tertiary blast effect 3) Intestinal primary blast injuries not uncommonly present days after the explosion 4) Potential pulmonary primary blast injuries need not be considered when selecting anesthetic options and operating for abdominal primary blast injuries more than 48 hours after the blast a. 1, 3 are correct b. 2, 4 are correct c. 1, 2, 3 are correct d. 4 only 32) When pulmonary primary blast injury is suspected, which of the following is recommended in the initial treatment plan? 1) Administering supplemental oxygen 2) Aggressive diuresis to achieve a "dry" (hypovolemic) patient 3) Keeping the patient supine in the left lateral decubitus position with the head down (if the injury is equivalent in each hemithorax) to decrease risk of air embolus 4) Immediate intubation and positive pressure ventilation a. 1, 3 are correct b. 2, 4 are correct c. 1, 2, 3 are correct d. 4 only 33) Altitude restriction to sea level during an air evacuation is very rarely indicated. a. True. b. False. 34) The future trend in air evacuation is towards transport of critically ill and fresh postop patients to 4th or 5th echelon hospitals for their definitive care. a. True b. False 35) All of the following are possible modes of transportation for a Mobile Field Surgical Team except: a. C-130 b. Chevy Suburban c. Blackhawk helicopter d. HMMWV ambulance e. All are possible. 36) The Mobile Field Surgical Team is designed to address the following type(s) of injury(ies), including surgery if necessary: a. Thorax b. Abdomen c. Major extremity injuries, including vascular injury d. All of the above 37) The “ramp up” phase of a medical deployment is: a. Preparation time, just before casualties arrive at the facility b. The time during which only surgical interns care for the patients (wedge = man’s simplest tool) c. The early period of a deployment, before medical assets are fully established 38) Victims of depleted uranium (DU) munitions: a. Should have their care delayed until they can be decontaminated b. Have no related toxicity from the heavy metal properties of the DU c. Pose no radiation hazard to medical personnel, and therefore, should not have their care delayed d. Require special precautions in addition to standard universal precautions 39) Which of the following agents used to neutralize the effects of chemical weapons requires corps or division command direction prior to its use? a. Atropine b. Pyridostigmine bromide c. 2-PAM chloride d. Diazepam 40) Management of patients with illness secondary to chemical weapons can be challenging because: a. The non-specific symptoms of some agents can confound the diagnosis b. Rapid diagnosis is essential c. The clinical presentation after the exposure may be delayed d. All of the above.