Design of a Molecular Diagnostic Lab
advertisement
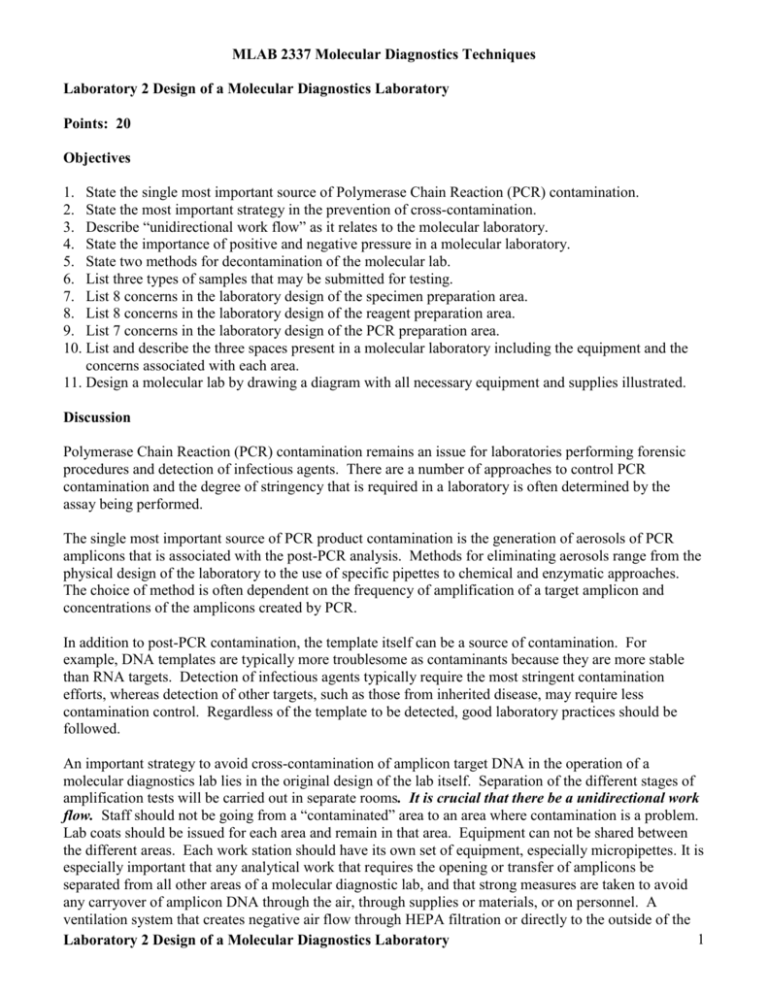
MLAB 2337 Molecular Diagnostics Techniques Laboratory 2 Design of a Molecular Diagnostics Laboratory Points: 20 Objectives 1. State the single most important source of Polymerase Chain Reaction (PCR) contamination. 2. State the most important strategy in the prevention of cross-contamination. 3. Describe “unidirectional work flow” as it relates to the molecular laboratory. 4. State the importance of positive and negative pressure in a molecular laboratory. 5. State two methods for decontamination of the molecular lab. 6. List three types of samples that may be submitted for testing. 7. List 8 concerns in the laboratory design of the specimen preparation area. 8. List 8 concerns in the laboratory design of the reagent preparation area. 9. List 7 concerns in the laboratory design of the PCR preparation area. 10. List and describe the three spaces present in a molecular laboratory including the equipment and the concerns associated with each area. 11. Design a molecular lab by drawing a diagram with all necessary equipment and supplies illustrated. Discussion Polymerase Chain Reaction (PCR) contamination remains an issue for laboratories performing forensic procedures and detection of infectious agents. There are a number of approaches to control PCR contamination and the degree of stringency that is required in a laboratory is often determined by the assay being performed. The single most important source of PCR product contamination is the generation of aerosols of PCR amplicons that is associated with the post-PCR analysis. Methods for eliminating aerosols range from the physical design of the laboratory to the use of specific pipettes to chemical and enzymatic approaches. The choice of method is often dependent on the frequency of amplification of a target amplicon and concentrations of the amplicons created by PCR. In addition to post-PCR contamination, the template itself can be a source of contamination. For example, DNA templates are typically more troublesome as contaminants because they are more stable than RNA targets. Detection of infectious agents typically require the most stringent contamination efforts, whereas detection of other targets, such as those from inherited disease, may require less contamination control. Regardless of the template to be detected, good laboratory practices should be followed. An important strategy to avoid cross-contamination of amplicon target DNA in the operation of a molecular diagnostics lab lies in the original design of the lab itself. Separation of the different stages of amplification tests will be carried out in separate rooms. It is crucial that there be a unidirectional work flow. Staff should not be going from a “contaminated” area to an area where contamination is a problem. Lab coats should be issued for each area and remain in that area. Equipment can not be shared between the different areas. Each work station should have its own set of equipment, especially micropipettes. It is especially important that any analytical work that requires the opening or transfer of amplicons be separated from all other areas of a molecular diagnostic lab, and that strong measures are taken to avoid any carryover of amplicon DNA through the air, through supplies or materials, or on personnel. A ventilation system that creates negative air flow through HEPA filtration or directly to the outside of the 1 Laboratory 2 Design of a Molecular Diagnostics Laboratory building will help to “quarantine” a PCR detection room. Disposable personal protective equipment (PPE) such as lab coats should be used by lab personnel and should not leave a PCR detection room. Any supplies, equipment, or materials should likewise not leave a PCR detection room without first being treated and/or contained. Chemical and physical decontamination measures should also be used: work areas can be treated with a 10% bleach solution followed by wipe down with deionized water, and ultraviolet lights to irradiate rooms overnight can also degrade amplicon DNA contamination. Scope of the Laboratory Exercise: In this lab exercise, you will work with a lab partner to design your ideal of a molecular diagnostic lab to prevent amplicon cross-contamination. You will also outfit your lab with necessary materials and equipment required in each of the rooms that you design, based on a general description of the steps that might be involved in conducting a PCR experiment that follows. DESIGNING THE SPACE FOR A MOLECULAR LABORATORY Airflow is crucial to prevent contamination. Some rooms require positive air pressure and others require negative air pressure. Positive pressure means the amount of supply air is greater than the exhaust which prevents the reversal of the direction of air movement, which keeps contaminants from entering the room. Negative pressure causes air to be removed at a higher rate than supplied so that the room is under negative pressure to surrounding rooms and corridors. This prevents air from migrating from the laboratory into adjacent areas. To maintain negative pressure doors must remain closed. The general rule of thumb is to use positive pressure to keep contaminants out of an area, and negative pressure to capture contaminants and keep them from contaminating surrounding areas. Laboratory Space Arrangement A molecular laboratory should be designed so that there is a minimal chance of contamination. This is achieved by creating separate areas for the different tasks involved in performing molecular testing and following strict guidelines when moving from one room to another. . Ideally a molecular laboratory should be divided into three physically separate rooms: reagent preparation, sample preparation and PCR. 1. Reagent preparation, using positive pressure to prevent the introduction of contaminants. 2. Sample preparation area using negative pressure to keep template nucleic acids in the room. 3. PCR room is used for amplification and product detection, using negative pressure to keep amplified nucleic acids in the room. Reagent preparation Here, master mix (amplification reagents) and primers are prepared along with controls. Prepared master mix and controls are then added to the PCR reaction tubes. The types of equipment needed in this area include refrigerators, computer, freezers, shelving for supplies, disinfectants, micropipettes and tips, balances, measuring devices such as beakers and pipettes, vortex, assorted racks, balances, ice machine, sinks microwave oven and PPE. Concerns: 1. This room should be kept as far away as possible from any room where PCR amplicons are detected or transferred. 2. If possible, this room should be separated into two spaces to separate work with controls and primers from the master mixes. Laboratory 2 Design of a Molecular Diagnostics Laboratory 2 3. Efforts should guard against any sharing of equipment, instruments, and supplies used in this room with other work areas. 4. All solutions should be prepared as freshly as possible for each PCR run, and all solutions should be kept cold until ready to load on the thermal cycler. Reaction tubes/plates should be capped/covered once prepared and ready to leave this work are. 5. Long-term storage of primer and control DNA should be at -80oC. 6. Shorter-term storage, from day to day, of primer and control DNA, as well as the components of the amplification master mix, should be stored in a manual defrost -20oC freezer. 7. PPE such as gloves and lab coats should be used by personnel working in this area at all times, but should not leave this area. 8. If UV lighting is used to maintain contamination-free work area, care must be taken to make sure that they are off when personnel are present. Specimen preparation Specimens are processed and undergo nucleic acid isolations by a number of methods, depending on the tissue. For example, fresh whole blood is centrifuged to remove red blood cells and to isolate the buffy coat for some assays, and plasma or serum will be used directly for other assays. Frozen solid tissue is thawed briefly, sampled, and refrozen immediately. Solid tissue sample is chopped before DNA isolation. Validated and quality checked DNA isolation kits are used to isolate nucleic acids, following the manufacturers’ protocols and specifications. The kit used depends on the tissue type and the requested test type. Some kits will use solid-phase extraction techniques in which a vacuum manifold or slow-speed microcentrifuge is required. Other kits use liquid extraction techniques in which a high speed microcentrifuge is required. Micropipettes and microcentrifuge tubes of all sizes are required for all isolations. DNA samples isolated from specimens can be added to the PCR master mix reaction tubes/microplate wells in this room. The types of equipment needed in this area include computer, micropipettes, transfer pipettes, serological pipettes, centrifuges, assorted racks, containers to transfer samples into, centrifuges, refrigerators and possibly freezers, biological cabinet with laminar-flow HEPA air filtration, dead-air box with an optional UV light, disinfectants, sinks, and PPE. Concerns: 1. Ventilation filters, and decontamination procedures must be used to minimize risk of crosscontamination between specimens. 2. Efforts should guard against any sharing of equipment, instruments, and supplies used in this room with other work areas. 3. Specimens should be stored separately from other reagents. 4. Dry baths are preferred over water baths since water baths can contaminate specimens through seepage into poorly stoppered tubes. 5. To avoid specimen-to-specimen contamination, plugged (aerosol-barrier) pipette tips or positivedisplacement tips should be used. 6. All solutions should be prepared as freshly as possible for each PCR run, and all solutions should be kept cold until ready to load on the thermal cycler. Reaction tubes/plates should be capped/covered once prepared and ready to leave this work are. 7. PPE such as gloves and lab coats should be used by personnel working in this area at all times, but should not leave this area. 8. If UV lighting is used to maintain contamination-free work area, care must be taken to make sure that they are off when personnel are present. Laboratory 2 Design of a Molecular Diagnostics Laboratory 3 PCR Amplification-ready reactions are added to the thermal cyclers here and the PCR products (amplicons) are detected. The PCR room should contain two functional work areas: a pre-amplification (pre-PCR) and post-amplification (post-PCR) area. These two areas would ideally be in totally separate rooms. If there is limited space then the creation of separate work stations is acceptable as long as the supplies and equipment are dedicated to each area and are NEVER interchanged between the two areas. A laminar flow hood should be used to perform clean preparations. The types of equipment needed in the PCR area include computer, micropipettes, microtubes, microcentrifuge, assorted racks, vortex, disinfectants, heat blocks, thermocyclers, ice machine, ice machine, electrophoresis equipment (gel boxes, power supplies, transilluminators), gel documentation system, sinks and PPE. Concerns: 1. This room should be divided into two work spaces (pre- and post-PCR), if possible, to minimize contamination of thermal cyclers from aerosols created where reaction tubes/microplate wells are opened following the PCR reaction for detection by gel electrophoresis. Note that if PCR analysis is real-time PCR, reaction tubes need not be opened except to validate or clarify a result with gel electrophoresis. 2. Reaction tubes/microplates should be kept chilled and sealed until ready to load into the thermal cycler. Seals should be tight enough to avoid evaporative losses during the high prolonged temperatures of the thermal cycling. 3. Ventilation and decontamination procedures must be used to minimize risk of contaminating the room and equipment with amplicon target DNA. 4. Efforts should guard against any sharing of equipment, instruments, and supplies used in this room with other work areas. 5. To avoid specimen-to-specimen contamination, plugged (aerosol-barrier) pipet tips or positivedisplacement tips should be used. 6. PEP such as gloves and lab coats should be used by personnel working in this area at all times, but should not leave this area. 7. If UV lighting is used to maintain contamination-free work area, care must be taken to make sure that they are off when personnel are present. Laboratory 2 Design of a Molecular Diagnostics Laboratory 4 PROCEDURE Students will design the layout and equipping of a molecular diagnostics lab to avoid cross-contamination of target DNA. 1. Carefully review documents in BlackBoard for setting up a molecular lab. DO NOT PRINT OUT unless you want a hard copy. Refer to section 2 General Guidelines in the PCR Application Manual. This document is 340 pages long. 2. Using a pencil, paper, and ruler OR using a computer, draw the layout of rooms in your ideal design of a molecular diagnostic lab. Be sure to indicate the direction of the work flow from room to room. 3. Arrange equipment and instruments in each of your rooms to meet the needs of each work area that you have designed, and label your drawing. You may want to consult a suggested check list below to make sure that all your equipment and instruments needs are adequately met. Check List of Instruments and Equipment for a Molecular Diagnostics Lab – You may also wish to refer to additional documents in BlackBoard Balance/scale Bench spaces Biological cabinet with laminar-flow HEPA air filtration Cabinets for storage of consumables and RT reagents. Centrifuge Computer Dead-air box with an optional UV light Electrophoresis equipment (apparatus and power supplies) Freezer Gel imaging/documentation system (transilluminator) Gloves (be sure to place in each room where needed) Heat blocks Ice machine Lab coats (be sure to place in each room where needed) Lab coat rack (be sure to place in each room where needed) Microcentrifuge Micropipettes (be sure to place in each room where needed) Microwave oven Plastic ware and disposables Refrigerators for storage of samples. Refrigerators for storage of reagents. Regular centrifuges for samples Sinks Test tube racks Thermal cyclers (routine and real-time PCR) Vortex Laboratory 2 Design of a Molecular Diagnostics Laboratory 5 Name ________________________________________ Date ___________________ MLAB 2337 Molecular Diagnostics Techniques Laboratory 2: Design of a Molecular Diagnostics Laboratory Laboratory Results Points: /20 1. On the following page submit a drawing of your “dream” lab. 2. In the space below explain the reasons or logic behind the design of your room layout. 3. In the space below explain the reasoning or logic behind your placement of equipment. Laboratory 2 Design of a Molecular Diagnostics Laboratory 6 Name ________________________________________ Date ___________________ MLAB 2337 Molecular Diagnostics Techniques Laboratory 2: Design of a Molecular Diagnostics Laboratory Laboratory Results Draw your dream lab. You may use the back of this page to get more room. IMPORTANT: All equipment listed on page 5 MUST be present in appropriate rooms. Laboratory 2 Design of a Molecular Diagnostics Laboratory 7 Name _____________________________________ Date ____________________ MLAB 2337 Molecular Diagnostics Techniques Laboratory 2: Design of a Molecular Diagnostics Laboratory Study Questions Points: 19 Instructions: Copy/paste the following study questions into word processing document. Answer the questions Save the file as “Lab2LabDesignYOUR NAME” Submit to “Assignments” in BlackBoard 1. State the single most important source of Polymerase Chain Reaction (PCR) contamination. (1 point) 2. State an important strategy in the prevention of cross-contamination. (1 point) 3. Describe what is meant by “unidirectional work flow” as it relates to a molecular laboratory. (1 point) 4. Describe positive and negative pressure as it relates to airflow (2 points): a. Positive b. Negative 5. What is the general rule of thumb used to describe positive and negative airflow? (2 points) 6. List and briefly describe the three rooms which, ideally, the molecular laboratory should be composed of? (3 points) a. b. c. 7. List 3 of the 8 concerns listed for the reagent preparation area that you believe are MOST important. (3 points) a. b. c. 8. List 3 of the 8 concerns listed for the specimen preparation area that you believe are MOST important. (3 points) a. b. c. 9. List 3 of the 7 concerns listed for the PCR area that you believe are MOST important. (3 points) a. b. c. Laboratory 2 Design of a Molecular Diagnostics Laboratory 8