chapter 19-blood vessels
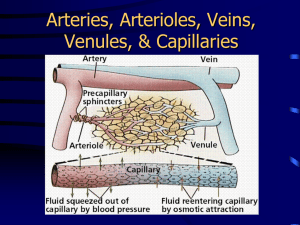
advertisement
CHAPTER 19-BLOOD VESSELS I. BLOOD VESSELS-are responsible for delivering blood to all parts of the human body. A. As the heart contracts it forces blood into arteries which branch into smaller arteries that branch to from smaller arterioles. Arterioles carry blood into capillaries (capillary beds) which carry blood into body tissues. B. Blood returning from the capillary beds empties into venules that merge to form veins. Veins ultimately empty into the heart. II. ARTERIES-carry blood away from the heart. A. In general, arteries carry oxygenated blood. B. Structure of the Wall of Arteries: 1. 3 Layers in arterial walls (are also known as tunics): a. Tunica interna-innermost layer. Also known as the tunica intima. 1) Surrounds a central blood-containing space known as the lumen. 2) Lined with endothelium (simple squamous epithelium). This tissue reduces friction as blood moves through the lumen. b. Tunica media-composed primarily of smooth muscle tissue and elastic tissue. 1) This smooth muscle is regulated by the autonomic nervous system and various chemicals. 2) Vasoconstriction (reduction in lumen diameter due to smooth muscle contraction) and Vasodilation (widening of the lumen due to smooth muscle relaxation) both occur in the tunica media. 3) This layer is typically the thickest layer in the walls of arteries. This layer also helps to regulate blood pressure and blood flow. c. Tunica externa (tunica adventitia)-outermost layer of the arterial wall. 1) Is primarily connective tissue in structure. 2) Vasa vasorum-tiny blood vessels that carry blood into the outer layers of the arterial walls (into the tunica externa). C. 3 Types of Arteries 1. Elastic (Conducting) Arteries-thick-walled; located near the heart. Includes the aorta and its branches. These are the largest arteries in the body. a. These are called conducting arteries since they carry blood away from the heart. 2. Muscular (Distributing) Arteries-deliver blood to specific body organs. a. They have the thickest tunica media of any of the blood vessels. b. These are actively involved in vasoconstriction and vasodilation. 3. Arterioles-smallest arteries, these carry blood into capillaries. a. When these constrict, they shut off blood to specific tissues. When they dilate, blood flow increases greatly into tissues. III. CAPILLARIES-microscopic blood vessels. Are the smallest vessels in the body. A. Their walls consist of only a tunica interna and their walls are typically only one cell layer thick. 1. Why is this important? B. Capillaries are the primary sites for the exchange of materials (gases, nutrients, hormones) between the blood and body tissues and interstitial fluid. C. Capillaries are arranged in thick networks known as capillary beds. D. 3 Types of Capillaries: 1. Continuous capillaries-their lining is not broken. 2. Fenestrated capillaries-have numerous pores in their lining. 3. Sinusoidal capillaries-very permeable; found in some organs. E. Capillary Beds-networks of capillaries. These regulate blood flow to/through organs. 1. On the opposite ends of arterioles, capillary beds unite to form venules. Venules then connect to form veins. IV. VEINS-carry deoxygenated blood back to the heart. A. Blood flow is sluggish at best in veins. B. Veins have 3 distinct tunics, but their walls are always thinner and their lumens larger than those of arteries. 1. Due to this, veins accommodate a large blood volume. They may store as much as 65% of total blood volume. C. Blood pressure is low in veins. Why is this so? D. Veins contain Valves along their tunica interna. These valves prevent the backflow of blood in the the veins of the body. The valves are most numerous in the veins of the limbs. E. Veins collapse when cut. F. Venous sinuses-specialized, flat veins. These serve as collection areas for blood and body fluids. G. Varicose veins-occur when veins dilate. Is usually caused by incompetent valves. 1. Prolonged standing, obesity, genetic factors all contribute to varicose veins. 2. Treatment often includes surgical removal of the veins. H. Hemorrhoids-occur when blood does not exit the veins of the anal canal. These veins fill with blood and swell. Causes include pregnancy, prolonged sitting. I. Phlebitis-inflammation or injury to a vein. Blood clots may form in the vein. J. Anastomoses-interconnections between 2 or more vessels (arteries or veins) supplying the same body region. These provide alternate routes for blood flow to a body region. K. As a rule, in adults, arteries carry oxygenated blood and veins carry deoxygenated blood. 1. Sole Exception in adults: pulmonary artery carries deoxygenated blood and the pulmonary vein carries oxygenated blood. V. PHYSIOLOGY OF CIRCULATION A. Blood must be kept circulating for us to survive. B. Key Terms Relating To Circulation: 1. Blood Flow-volume of blood flowing through a vessel or organ in a given period of time (ml/min). Is equivalent to cardiac output. 2. Blood Pressure (BP)-the force per unit area exerted on the wall of a blood vessel by its contained blood. Is expressed in mm Hg. 3. Resistance-the opposition to blood flow. This also includes any friction blood faces as it travels through the body. 4. Blood Viscosity-refers to the thickness of blood. C. Blood Pressure (BP)-is usually associated with arteries. Is measured with a sphygmomanometer. 1. Systolic Pressure-occurs when BP is highest against the wall of the aorta and other arteries. a. This is caused by ventricular contraction (or systole). b. This typically measures around 120 mmHg. c. This causes a great deal of stretching in arteries and along their walls. 2. Diastolic Pressure-the lowest blood pressure reading. a. This occurs during ventricular diastole (filling). b. Aortic pressure is low at this point. This is actually caused by the force of the elastic arteries returning to their original position. It usually measures 60-80 mmHg. 3. BP is expressed systolic/diastolic. For example: 120/80. 4. There is a wide variation in blood pressure in different individuals. a. Hypertension-high blood pressure. Occurs when BP is greater than 140/95 mmHg. 1) Causes include: atherosclerosis and kidney disease (the kidney releases renin which increases BP). 5. Factors That Influence Blood Pressure: a. Cardiac output b. Blood volume c. Peripheral resistance-resistance to blood flow caused by blood viscosity and/or the changing diameter of arterioles. 6. Controls that act to maintain normal blood pressure: a. Vasomotor center-in the medulla of the brain. Makes up part of the cardiovascular center. The vasomotor center regulates arteries. b. Baroreceptors-located in most large arteries. 1) These stretch when BP increases. When this happens, baroreceptors send impulses to the vasomotor center. These impulses inhibit the vasomotor center; therefore, vasodilation of arteries and arterioles occur and BP drops. c. Chemoreceptors-including carotid and aortic bodies 1) When O2 levels drop or CO2 levels increase in the blood, these receptors send impulses to the cardiovascular center. In response, the cardiovascular center increases cardiac output; thus causing vasoconstriction to occur. Due to this, BP increases. d. Chemicals-primarily hormones (norepinephrine, epinephrine). e. Higher brain centers-primarily the cerebrum (regulates BP during rage, anger). f. Autoregulation-local adjustments of blood flow in a given region of the body in response to local tissue needs. g. Kidney function-can increase or decrease water retention to influence blood pressure. The kidney can stimulate the adrenal gland to release aldosterone which increases sodium uptake in the kidney. Water follows sodium back into the blood. D. Pulse Pressure (Pulse)-waves of pressure along arteries caused by ejection of blood from the heart into the aorta. This is best felt in arteries over bones (as in the wrist). 1. Pulse provides information on the rate of heart beat. E. Blood flows from regions of higher pressure to regions of lower pressure. 1. BP falls from the aorta (100 mmHg) to arteries, to arterioles to the capillary bed (40 mmHg), to venules to veins (2 mmHg). 2. Obviously BP is low in veins. Blood flow is sluggish in veins. 3. Factors that aid Venous Return: a. Respiratory Pump-breathing creates pressure changes in the ventral body cavity. These pressure changes act to “suck” blood upward towards the heart. b. Skeletal Muscle Contractions-tighten around veins which helps to force blood towards the heart. c. Valves-on the inner walls of veins close to prevent blood from backflowing. d. Velocity of Blood Flow-blood leaves small capillaries and venules and enters larger veins. Veins offer less resistance to flow. F. Capillary Exchange 1. The movement of water and dissolved substances (except proteins) through capillaries is greatly affected by hydrostatic pressure and osmotic pressure. 2. Blood Hydrostatic Pressure (BHP)-the blood pressure in capillaries. This tends to move fluid out of a capillary. Is also known as Capillary Hydrostatic Pressure (HPc). 3. Interstitial Fluid Hydrostatic Pressure (HPif)-pressure of interstitial fluid against the cells of a tissue and cells on the outside of capillary walls. This moves fluid into capillaries. 4. Blood Osmotic Pressure (BOP) or Colloid Osmotic Pressure-pressure created by the presence of large plasma proteins in the blood. This tends to move fluids into capillaries via osmosis. 5. Interstitial Fluid Osmotic Pressure (IFOP)-pressure created by the presence of large plasma proteins in tissue (interstitial) fluid. This tends to move fluid out of capillaries. 6. Whether fluids exit or enter capillaries depends on how the above pressures relate to each other. If the pressures that move fluids out of capillaries are greater than the pressures that move fluids into capillaries, then fluid will move into tissue spaces. The opposite is also true. 7. Net Filtration Pressure (NFP)-is used to illustrate the direction of fluid movement in capillaries. a. NFP=(BHP + IFOP) - (HPif + BOP) 8. At the arterial end of a capillary, there is typically a positive NFP which forces fluid into tissue spaces. At the venous end of a capillary, there is a negative NFP which forces fluid into the capillary. 9. Not all fluids filtered at one end of a capillary are reabsorbed at the other end-this includes some types of lymph. However, the movement of fluid between plasma and interstitial fluid is in a state of near equilibrium at the arterial end and venous end of a capillary. That is, filtered fluid and reabsorbed fluid are nearly equal. This near equilibrium is known as Starling’s Law of the Capillaries. G. Blood Reservoirs 1. 59% of blood is in veins, venules and venous sinuses (thin-walled, enlarged veins). These structures serve as blood reservoirs or storage areas for blood. 2. This blood can be moved out of these areas to other parts of the body quickly under times of need (exercise, etc...). H. Circulatory Shock-any condition in which blood vessels are inadequately filled and blood cannot circulate properly. This results in inadequate blood flow and can lead to tissue death if it persists. VI. 3 MAJOR CIRCULATORY ROUTES IN THE BODY A. Systemic Circulation-oxygenated blood leaves the left ventricle through the aorta and travels to systemic arteries. Deoxygenated blood from the organs returns via systemic veins into the superior or inferior vena cava then into the right atrium. 1. 2 Specialized Circulatory Routes in the Systemic Circulation: a. Coronary Circulation-to myocardium of the heart. b. Hepatic Portal Circulation-blood flow to/from the liver. The liver regulates nutrients in the blood and it removes foreign debris from the blood. 1) In the hepatic portal circulation, the following events occur: a) Hepatic Portal Vein-carries blood from the GI tract to the liver. b) In the liver, the blood passes through enlarged venous areas known as hepatic sinusoids. c) Kupffer Cells in the sinusoids remove bacteria from the blood and enzymes in the sinusoids remove certain chemicals from the blood. 2. The Aorta-the largest artery in the body. It exits the left ventricle of the heart. a. 4 Portions of the Aorta: 1) Ascending Aorta-posterior and to the right of the pulmonary trunk. This runs from the left ventricle to the sternal angle. 2) Aortic Arch-begins and ends at the sternal angle. 3) Descending (Thoracic) Aorta-runs from T5 to T12 along the spine. It sends off many small arteries to the thorax and viscera before it runs through the diaphragm. 4) Abdominal Aorta-begins at the entrance of the abdominal cavity (T12 or diaphragm). It supplies viscera and the abdominal walls in the abdominal cavity. It ends at L4-where it branches. B. Pulmonary Circulation-carries deoxygenated blood from the right ventricle through the pulmonary artery to the lungs. In the lungs, this blood picks up oxygen and this oxygenated blood is then returned to the left atrium via the pulmonary veins. C. Fetal Circulation-exchange of materials between a fetus and the mother. 1. In a fetus, the lungs, kidneys and digestive tract are nonfunctional. 2. Placenta-cord that attaches to the wall of the mother’s uterus and to the fetus. a. Umbilical cord-carries oxygenated blood and nutrients from the mother to the fetus. 1) Most of this blood bypasses the fetal liver by flowing through the ductus venosus-a modification of the inferior vena cava. 2) 2 Umbilical Arteries carry deoxygenated blood (containing CO2 and wastes) from the fetus to the placenta. There is no mixing of maternal and fetal blood. a) All exchanges occur by diffusion across the placenta. b) The umbilical vein and the 2 umbilical arteries make up the umbilical cord which is shed at birth with the placenta. 3. In the fetal heart, there is no need for blood to be pumped to the lungs. There are 2 modifications in the fetal heart to allow blood to partially bypass the lungs: a. Foramen ovale-a hole in the interatrial septum. Blood can pass from the right atrium to the left atrium through this hole. Blood then moves on to the aorta. b. Ductus arteriosus-duct connecting the pulmonary artery with the arch of the aorta. Blood passes from the right atrium to the right ventricle through this duct. c. Both of these modifications close off shortly after birth. If they fail to close, then congenital heart defects can develop. VII. RELATED CLINICAL TERMS-at end of chapter. A. Aneurysm B. Angiogram C. Diuretic D. Phlebitis E. Phlebotomy F. Sclerotherapy G. Thrombophlebitis