Antibiotic Resistant Organisms (ARO) in the Community
advertisement
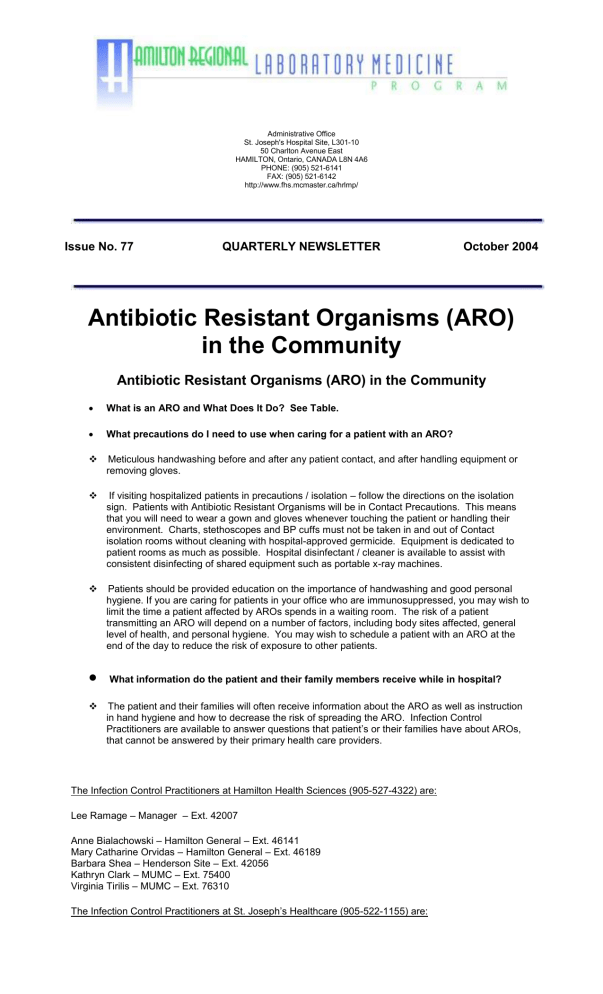
Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 77 QUARTERLY NEWSLETTER October 2004 Antibiotic Resistant Organisms (ARO) in the Community Antibiotic Resistant Organisms (ARO) in the Community What is an ARO and What Does It Do? See Table. What precautions do I need to use when caring for a patient with an ARO? Meticulous handwashing before and after any patient contact, and after handling equipment or removing gloves. If visiting hospitalized patients in precautions / isolation – follow the directions on the isolation sign. Patients with Antibiotic Resistant Organisms will be in Contact Precautions. This means that you will need to wear a gown and gloves whenever touching the patient or handling their environment. Charts, stethoscopes and BP cuffs must not be taken in and out of Contact isolation rooms without cleaning with hospital-approved germicide. Equipment is dedicated to patient rooms as much as possible. Hospital disinfectant / cleaner is available to assist with consistent disinfecting of shared equipment such as portable x-ray machines. Patients should be provided education on the importance of handwashing and good personal hygiene. If you are caring for patients in your office who are immunosuppressed, you may wish to limit the time a patient affected by AROs spends in a waiting room. The risk of a patient transmitting an ARO will depend on a number of factors, including body sites affected, general level of health, and personal hygiene. You may wish to schedule a patient with an ARO at the end of the day to reduce the risk of exposure to other patients. What information do the patient and their family members receive while in hospital? The patient and their families will often receive information about the ARO as well as instruction in hand hygiene and how to decrease the risk of spreading the ARO. Infection Control Practitioners are available to answer questions that patient’s or their families have about AROs, that cannot be answered by their primary health care providers. The Infection Control Practitioners at Hamilton Health Sciences (905-527-4322) are: Lee Ramage – Manager – Ext. 42007 Anne Bialachowski – Hamilton General – Ext. 46141 Mary Catharine Orvidas – Hamilton General – Ext. 46189 Barbara Shea – Henderson Site – Ext. 42056 Kathryn Clark – MUMC – Ext. 75400 Virginia Tirilis – MUMC – Ext. 76310 The Infection Control Practitioners at St. Joseph’s Healthcare (905-522-1155) are: Ruth Stevenson – Manager – Ext. 3347 May Griffiths-Turner Ext. 3385 Stephanie Trowbridge Ext. 3595 Barb Lang Ext. 6362 The Infection Control Practitioner at St. Peter’s Hospital is: Suzanne Martin 905-777-3837 Ext. 12429 DETAILS METHICILLIN RESISTANT STAPHYLOCOCCUS AUREUS (MRSA) VANCOMYCIN RESISTANT ENTEROCOCCUS (VRE) MULTIRESISTANT PSEUDOMONAS AERUGINOSA (MRPA) What is it? Strain of Staphylococcus aureus resistant to the most commonly used antibiotics including Cloxacillin and the Cephalosporins Strain of Enterococcus resistant to all antibiotics including Vancomycin. These are strains of Pseudomonas that are resistant to many of the antibiotics normally used to treat them, including Ciprofloxacin. These are plasmid-mediated enzymes carried in gram-negative bacteria that are capable of breaking down broadspectrum ß lactam antibiotics such as cefotaxime, ceftriaxone, and ceftazidime. Where is it found? Colonizes skin but can spread to all body sites, particularly invasive devices such as indwelling urinary catheters, IV and central lines, Endotracheal tubes and decubiti, post-operative wounds and blood. Enterococcus is normal bowel flora. VRE is readily detected upon rectal swabs. VRE can colonize a patient at other sites including indwelling catheters, decubiti, post-operative wounds and invasive sites Pseudomonas is a bacterium that is found naturally in soil, water and plants. It is often found in the throat and feces of people and animals. It is able to grow and survive in standing water and some solutions. Most common organisms with these enzymes are What types of infections are associated with these organisms? MRSA usually colonizes a patient, however, up to 50% of colonized patients may develop infections. MRSA has the ability to cause the same type of infections as Staph. aureus such as boils, post-operative wound infections, cellulitis, bacteremia, and toxic-shock syndrome. VRE usually colonizes a patient but can cause infection depending on patient’s condition and site of infection. Patients with Clostridium difficle may be colonized with VRE. Multi-resistant pseudomonas can be a colonizer, but can also cause respiratory tract infections, ear, wound infections and urinary tract infections. ESBL’s can be colonizers but they have also been implicated in infections. They can cause infections at sites affected by E. coli or Klebsiella species such as urinary tract, bloodstream, and respiratory tract. What is the treatment? DECOLONIZATION THERAPY: Is controversial and should be individually assessed to determine if they are a candidate, and if they can tolerate therapy. Consultation with Infectious Disease Physician may be beneficial. Colonization with VRE does not require treatment. Colonization with Multiresistant pseudomonas does not require treatment. If the patient has an infection, consultation with an ID physician is recommended. Cephalosporins will not be effective but are the most commonly used group of antibiotics used to treat patients with serious infections before the causative organism is known. Consultation with an Infectious Disease Physician may be beneficial. It is believed that Multiresistant pseudomonas is spread in the same manner as VRE and MRSA (on the hands of personnel from infected or colonized patients). It is believed that ESBLs are spread in the same manner as VRE and MRSA (on the hands of personnel from infected or colonized patients). CLINICAL INFECTIONS: If the patient is clinically infected, Vancomycin is the drug of choice. Vancomycin will NOT eradicate the colonization state, therefore, should only be used when a patient is clinically infected. How is it spread? BATHS: Antimicrobial soaps containing Chlorhexidine or Triclosan may be beneficial for 7-10 days. These are available at most drug stores. Direct contact from touching a patient colonized with MRSA and/or their environment. Hands are the most common source of transmission. If a patient has a VRE infection, they may benefit from a combination of antibiotics, and an Infectious Disease Physician should be consulted. Direct contact with the patient and/or their environment. Hands are the most common source of transmission. Lee Ramage, Mark Loeb, Cheryl Main and David Groves HRLMP Discipline of Microbiology Hamilton Regional Laboratory Medicine Program EXTENDED- SPECTRUM BETALACTAMASE PRODUCING ORGANISM (ESBL) E. coli and Klebsiella species, which are part of the normal intestinal flora.