CHIEF COMPLAINT: Evaluation of right shoulder pain and
advertisement
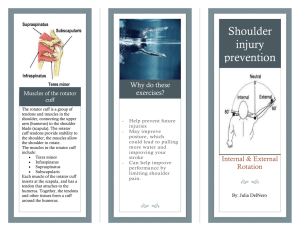
CHIEF COMPLAINT: Evaluation of right shoulder pain and consultation regarding right shoulder pain from Dominique Quincy, M.D. HISTORY OF PRESENT ILLNESS: Mrs. Xxxxx is a 52-year-old right-hand-dominant CPA who has been having problems with right shoulder pain and loss of range of motion since 11/2004. She has been followed by Dr. Quincy for this and she has had some pain so severe that she had to urgent care for this a couple weeks ago. She was given some narcotic pain meds for this and that really did not help her that much. She has been taking Tylenol, has not been taking the ibuprofen which she has along with the Tylenol she has been given. She has no specific history of injury to her shoulder. She used to be active playing tennis many years ago but now her only exercise is walking about 30 minutes four times per week. She does not describe any numbness in her hands. She notes some swelling in her hands. She has severe pain in her shoulder when sleeping on it. She is having trouble sleeping. She started to sleep flat on her back now because any time she rolls onto her shoulder it hurts her. ALLERGIES TO MEDICATIONS: None. SURGERIES: Include cesarean section in 1985 and cosmetic surgery in 1998. HABITS: Occasional alcohol. Quit smoking 25 years ago. CURRENT MEDICATIONS: Estrogen for perimenopausal symptoms. CURRENT MEDICAL CONDITIONS: None. SERIOUS ILLNESSES: None. REVIEW OF SYSTEMS: Review of 14 systems positive for excess fatigue, glasses. Otherwise unremarkable. FAMILY HISTORY: Noted for cancer. SOCIAL HISTORY: She is married, lives with her husband in Atherton. PHYSICAL EXAMINATION: This is a well appearing middle-aged woman accompanied by her husband. HT 5'6", WT 130 lb. Examination of right and left shoulder demonstrates 100 degrees of total elevation on the right, 180 degrees on the left, external rotation on the right is 10 degrees, external rotation on the left is _______ degrees, internal rotation on right is to the side, internal rotation on the left is to T12. There is no tenderness over the AC joint on the right or left. There is some pain to direct palpation over the rotator cuff. There is intact elbow flexion, extension, intact sensory motor exam on the forearm, intact pronation, supination in the hand, no significant swelling noted on the hand, no erythema or redness about the shoulder. RADIOGRAPHS: The patient has previously had MRI, radiographs and these are available for my review. The radiographs from 2/8/2005 demonstrate no significant evidence of glenohumeral arthrosis. There is a type I acromion without any significant spurs. The AC joint is not prominent. MRI from 2/15/2005 was also available for my review and there is a radiologist's report along with it. I concur with the radiologist that there is no evidence of complete rotator cuff tear. There is some question of rotator cuff tendinosis. There is some fluid around the biceps tendon but to me not an unusual amount. There are very minimal glenohumeral joint changes suggested by cysts in the humeral head. IMPRESSION: Right shoulder rotator cuff tendinosis with secondary frozen shoulder. RECOMMENDATIONS: The patient is advised that I think that her underlying symptomatology is a rotator cuff tendonitis followed by a secondary frozen shoulder. I think she needs a rotator cuff stretching and strengthening program with a therapist to regain her motion. She may be a candidate for subacromial bursectomy if she does not resolve her pain and possibly a candidate for arthroscopic capsular release if she does not get back her motion but at this point I think the mainstay of her treatment is going to be therapy. Because of the significant pain she is having I think a subacromial cortisone injection is reasonable. Therefore after adequate prepping with alcohol injection of lidocaine, Marcaine and Kenalog is made in the subacromial space with almost complete relief of the patient's shoulder pain. She is given a referral for therapy and we have selected a therapist for her in Menlo Park. I have asked her to go two to three times a week for the next four to six weeks for working on range of motion and stretching. I think she should take an anti-inflammatory and have transmitted Feldene 20 mg one p.o. daily to her pharmacy and I would like her to take this on a regular basis. She may take Extra Strength Tylenol in addition to this. I would like her to recheck in six weeks' time for a recheck and I have asked her to follow up with Dr. Andrew Haskell who might be more suitable for performing a subacromial arthroscopic surgery if she does need this.