Caesarean Section1846
advertisement
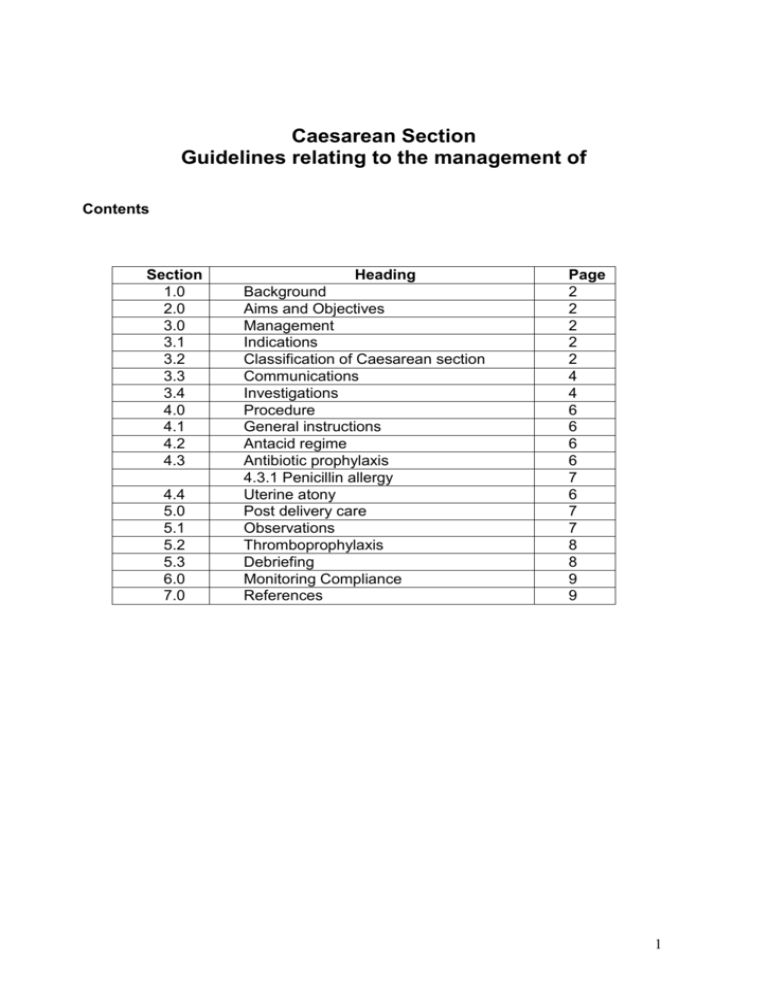
Caesarean Section Guidelines relating to the management of Contents Section 1.0 2.0 3.0 3.1 3.2 3.3 3.4 4.0 4.1 4.2 4.3 4.4 5.0 5.1 5.2 5.3 6.0 7.0 Heading Background Aims and Objectives Management Indications Classification of Caesarean section Communications Investigations Procedure General instructions Antacid regime Antibiotic prophylaxis 4.3.1 Penicillin allergy Uterine atony Post delivery care Observations Thromboprophylaxis Debriefing Monitoring Compliance References Page 2 2 2 2 2 4 4 6 6 6 6 7 6 7 7 8 8 9 9 1 1.0 BACKGROUND Caesarean Section is one of the commonest obstetric interventions. Approximately 20% of all deliveries at LTHT are Caesarean sections with 10% elective and 10% being performed in the emergency situation. 2.0 AIMS AND OBJECTIVES The aim of the guideline is to ensure the correct procedures are used, staffs are aware of their individual roles and that there is a team approach to optimise the safety of the mother and her baby. 3.0 MANAGEMENT 3.1 Indications 3.1.1 The commonest indications for elective Caesarean section are as follows. Most routine elective Caesarean sections should be performed at 39 weeks. Breech presentation Previous Caesarean section Placenta praevia (often delivered at 38 weeks) Multiple pregnancy when twin 1 breech (delivery 37-38 weeks depending on chorionicity) 3.1.2 The commonest indications to perform an emergency Caesarean section are as follows (list not exhaustive): Fetal distress – abnormal CTG in early labour, abnormal fetal blood sample, fetal bradycardia that does not recover, cord prolapse Failure to progress in first or second stage Failed instrumental delivery Malpresentation most commonly undiagnosed breech in labour Second twin Antepartum haemorrhage e.g. abruption with evidence of fetal compromise and/or maternal compromise, placenta praevia with active bleeding Pre-eclampsia/eclampsia where there has been a senior decision to deliver by emergency Caesarean section Planned caesarean section that presents in labour. All Caesarean sections must be discussed with a consultant and this decision must be documented in the notes. 3.2 Classification of Caesarean section When an emergency Caesarean section is necessary, it is important to minimise delays in order to optimise the outcome for both mother and baby. By adopting the classification described by Lucas et al (1) there will be a clear understanding of the urgency of delivery. Appropriate management should then take place in order to minimise the interval from decision to delivery while providing a safe anaesthetic. It is therefore vital that all members of the team, particularly the anaesthetist are informed as early in the process as possible. This communication must state the category of the 2 Caesarean section and the reason for it. The classification and examples are outlined below. The reason for performing the caesarean section and the category should be clearly stated on the operation proforma and documented in the birth record by the person making the decision. The time of decision will be when verbal consent is obtained. This time needs to be recorded in the clinical notes. Any reason for delay in undertaking the caesarean section should clearly be documented in the birth record. The decision to delivery interval (DDI) from Category 1 to 4 should be viewed as a ‘continuum of urgency’ rather than discrete categories. For example whilst the team may aim to deliver a baby in 30 minutes when there is a pH less than 7.20, a baby with an acute bradycardia will need to be delivered in a shorter DDI. It is also to be remembered that the category of urgency may change after the decision is made - a category 2 may become a category 1 or vice versa. Failure to progress in labour when there is no maternal or fetal compromise is a Category 3 Caesarean section according to NICE. It must however be remembered that significant delay will increase the risk of maternal and fetal morbidity for example bleeding secondary to uterine atony, maternal pyrexia, fetal compromise, and should be performed at the earliest opportunity for the theatre team. The woman does not need to be fasted in this situation. It is of vital importance that there continues to be clear communication between the obstetric / midwifery and anaesthetic staff at all times. Timings Table Category Definition Interpretation Examples (1) Emergency Immediate threat to life of mother, fetus’ or both Deliver in shortest possible time (may be under GA) Cord prolapse Major antepartum haemorrhage Ruptured uterus Prolonged bradycardia Second twin FBS Ph < 7.2 or STAN event when delivery is indicated Failure to progress with fetal or maternal compromise Antepartum haemorrhage with fetal and /or maternal compromise DDI 30 minutes (2) Urgent Threat to life of mother or fetus but not immediate (3)a Semiurgent No threat to life of mother or fetus but early delivery required No threat to life of mother or fetus but early delivery required No concerns over time of delivery (3)b Scheduled (4) Elective Call for senior anaesthetist help early, if difficulties encountered with regional anaesthesia DDI 45 minutes Generally woman in labour DDI 90 minutes Consider when entire team available and /or when fasted DDI 6 hours Delivery timed to suit woman and clinicians Failure to progress with no fetal or maternal compromise Planned C/S with SROM Failed IOL Fetal problems e.g. IUGR Maternal problems e.g. PET Breech presentation Previous C/S x2 All Category 1 Caesarean sections are subject to continuous audit and an audit form must be completed at the time of inputting delivery information onto MATSYS. 3 3.3 Communication & Documentation There must be a clear discussion with the woman and her partner regarding the indications for intervention. The reason for performing Category 1 or 2 Caesarean section must be documented in the birth records by the person making the decision. Options, if appropriate must be clearly documented in the notes. If there are language barriers, efforts must be made by the midwife to involve an interpreter for the consent process . The consent should be written, apart from situations where there is maternal compromise or fetal indications such as a pre-terminal bradycardia, where delivery must be as swift as possible. In such cases verbal consent must be obtained. It must be documented clearly in the clinical notes the reasons for it not being appropriate to gain written consent. Written consent for emergency Caesarean section must include the relevant indications. The risks of the procedure are as for elective procedures, namely, haemorrhage (sometimes requiring a blood transfusion), thrombo-embolic diseases, infection, and damage to bowel or bladder and also include the risk of fetal laceration. Where the indication for Caesarean section is placenta praevia or abruption, consideration must be given to include hysterectomy in the consent process. The decision to perform a Caesarean section will usually be taken by an Obstetrician of ST3 or above. The decision MUST be discussed with a senior obstetrician including the Consultant (i.e. Consultant + / - ST5 or above). This discussion must be documented in hand held records and/or the birth record. For emergency caesarean sections, In the event that delay would be life threatening to mother or baby, it is acceptable for the delivery suite coordinator to inform the Consultant of the need to perform an Emergency Caesarean Section. There must be clear communication between midwifery and medical staff - obstetric and anaesthetic, together with the theatre team. It is vital that the urgency and the category of the Caesarean section are clearly discussed between obstetric and anaesthetic team. The team performing the Caesarean section should work effectively. See Appendix 1 for cascade of information and the roles that should be taken by the team members. Consideration must be given to the potential difficulty of surgery and consideration for the presence of a senior obstetrician (ST5 or above) to be present although this should not delay the start of a category 1 section. Obstetric Consultants MUST be present when the indication is placenta praevia or for LSCS for second twin. Other examples when it may be appropriate to involve a senior obstetrician are preterm deliveries (under 32 weeks), known previous difficulty at surgery, previous abdominal surgery with known adhesions, and significant risk of bleeding associated with abruption. 4 3.4 Investigations and planning 3.4.1 Elective Caesarean section The indication and timing of delivery must be documented in the hand held maternity records. It is important to consider factors that may influence timing and the day of surgery. For example it is imperative that both a consultant anaesthetist and consultant obstetrician be available for a placenta praevia and this may therefore influence the day of surgery. If there are considered to be significant surgical difficulties then it may be appropriate to ensure a general surgeon is available. This should be the decision of the obstetric consultant in charge and discussed with the consultant obstetrician whose hot week it is. Any significant anaesthetic issues should also be raised with the anaesthetic team. Some women will have already been seen in the anaesthetic clinic. Pre-assessment Visit Woman should have a pre-assessment visit at 36 weeks or as soon as possible if the Caesarean section is booked after 36 weeks. All women must have MRSA screening prior to elective CS. This should be arranged in the antenatal clinic. Please refer to separate MRSA guideline and policy for those who screen positive. However, decolonisation will be required for a minimum of 5 days to finish on the day prior to surgery. Prophylactic antibiotics prescribed should be those with MRSA activity (see section 4.3). The woman should be offered a patient information leaflet on Caesarean section and on Consent. Informed consent should be obtained and the woman offered a copy of the consent form. The obstetrician should prescribe the prophylactic antibiotics (see section 4.3) A group and save is not necessary for all women having an elective Caesarean section. There are certain groups in which a group and save should be obtained in the week prior to the planned surgery i.e. those with an increased risk of blood loss. These will include previous postpartum haemorrhage, previous blood transfusion (may have irregular antibodies), multiple pregnancy, polyhydramnios and high BMI >40, previous difficult surgery. Blood will need to be available for the day of surgery in cases of placenta praevia (6 units should be cross matched). Consideration should also be given to arranging cell saver with the anaesthetic department with cases of placenta praevia and those women who would refuse blood products. Women having a planned Caesarean section prior to 38+6 weeks should be offered a course of antenatal corticosteroids to reduce the chances of respiratory morbidity in the neonate (see preterm birth guidelines for more details) Admission The majority of women will be admitted on the day of surgery to the postnatal ward. Diabetics and a small number of other women e.g. maternal infection, will need admission the night before so that treatment or additional observations can be performed. They should be admitted to the antenatal ward. All women should have a full set of observations documented on a MOEWs chart prior to surgery. 3.4.2 Emergency Caesarean section 5 The obstetrician is responsible for prescribing the prophylactic antibiotics (see section 4.3). All women should have a full blood count and Group and Save sent to the appropriate laboratory. Other cases with an increased risk of bleeding will require cross matched blood be requested – for example placenta praevia, abruption and known maternal coagulopathy. Consideration must be given for other blood products where there has been a significant haemorrhage antepartum or risk of coagulopathy. Please refer to guidance on patients who decline blood products if indicated. Swabs should be taken for MRSA screening (refer to separate MRSA guideline and policy for those who screen positive). Ideally this would be done prior to surgery but in an emergency situation it can be done prior to transfer to the recovery area. If delivery does not occur for more than 45 minutes in a woman in labour, the CTG should be categorised in order to detect any emerging fetal compromise. If the category has changed, the obstetric team should be informed and review requested. 4.0 PROCEDURE 4.1 General Instructions An operative proforma should be completed including clear documentation of the indication, category and time of decision and delivery Care should be given especially for the level of the uterine incision when being performed at full dilatation Paired cord blood samples should be taken in all emergency cases Consideration should be given to leaving a pelvic drain in situ where there has been difficulty achieving haemostasis or in the presence of thrombocytopenia or maternal conditions such as HELLP. 4.2 Antacid regime Those women requiring a Caesarean section, who are not fasted, should be considered for antacid prophylaxis which can be administered in the anaesthetic room. This applies even in women delivered by regional anaesthesia. For high risk labour where there is a high likelihood of Caesarean section, lanzoprazole 30mg orally should be given prophylactically. 4.3 Antibiotic prophylaxis It is the responsibility of the obstetrician to ensure that the correct antibiotics are prescribed and given. All women undergoing caesarean section, whether elective or as an emergency, should be given a single dose of antibiotics (see table below) prior to the start of sugery administered by the anaesthetist. There is good evidence to show that this reduces maternal morbidity, in particular the risk of endometritis is reduced by 66-75%2 and thus the use of antibiotic prophylaxis is compulsory. 4.3.1 Penicillin allergy Before administering antibiotics, a history of any allergy, but particularly with respect to penicillin should be checked. Some women will report nausea and vomiting or general reaction to antibiotics. A true allergy would be confirmed by skin rashes, breathing difficulty, urticaria, facial swelling, etc. 6 Cefuroxime is contraindicated only where there is a serious penicillin allergy i.e. anaphylaxis, breathing difficulty, facial swelling, urticarial rash or other major skin reaction. Procedure Standard prophylaxis Caesarean section (all categories) Co-amoxiclav 1.2g single dose IV MRSA Risk Penicillin Allergy Co-amoxiclav IV 1.2g & Teicoplanin 400mg IV Clindamycin 600mg IV over 30 minutes plus gentamicin 2mg/kgIV both single dose IV If antibiotics have been given in labour for maternal pyrexia, they should be continued until there has been no pyrexia for 24 hours. 4.4 Uterine atony A number of women requiring Caesarean section are at increased risk of uterine atony and postpartum haemorrhage. These include: Multiple pregnancy Prolonged labour on oxytocin infusion Large baby Following failed trial of instrumental delivery Antepartum haemorrhage Placenta praevia Consideration should therefore be given to prevention by commencing an oxytocin infusion in addition to the routine oxytocin bolus in the third stage of labour. The infusion will normally be requested by the Obstetrician. The regime is 40 units oxytocin diluted in 500mls 0.9% sodium chloride infused over 4 hours. Should the uterus fail to respond to first line uterotonics, consideration should be given to the use of ergometrine, misoprostol (800 micrograms given rectally) or haemabate (250 micrograms given as an intramuscular or intramyometrial injection) as described in the guidelines on postpartum haemorrhage. 5.0 CARE OF MOTHER IN FIRST 24 HOURS POST PARTUM Following delivery the surgeon should clearly document a post-operative care plan in the birth record which as a minimum should include: - how long the syntocinon infusion is required (if applicable) When to remove the drain (if applicable) When to remove the urinary catheter Timing of suture removal (if applicable) Thromboprophylaxis assessment Analgesics prescribed Need for postnatal follow up 5.1 Observations Depending on the indication for Caesarean section the woman will be transferred to either the recovery or high dependency area or back to her delivery room. She should not be left unattended during the immediate recovery period especially if they have had a general anaesthetic (see recovery guidelines). Women recovering from a GA should 7 have their oxygen saturations monitored and receive supplemental oxygen until they go to the ward and /or no longer using a PCAS. The following observations should be performed when the woman arrives in the recovery/HDU area and every 15 minutes thereafter: MOEWS (Modified Obstetric Early Warning Scoring) score. The midwife in charge needs to be informed of the MOEWS or if there are any concerns about the woman. The duty anaesthetist and obstetric registrar should be informed if MOEWS score shows one RED or Two YELLOW or if there are any concerns about the woman (see MOEWs information file for more detail) If oxygen saturations less than 95% the patient must receive oxygen 4 litres per minute via face mask. All patients who have had general anaesthesia will have oxygen automatically Ensure patient is alert and rousable In addition the following should be noted for women in recovery: Assess pain , nausea and treat as per instructions Checking of wound site, drain, lochia Check catheter drainage and urine output every hour Monitor oral intake with a fluid balance chart Check rate of infusion of intravenous fluids and cannula site Check medication and administer if required Apply TED stockings If blood products are to be given check and administer in line with blood product protocol Pressure areas should be noted and treated appropriately. In general, if observations are stable for 2 hours then transfer to the postnatal ward will take place. Following transfer to the postnatal ward the minimum observations would be: 1 hourly for 2 hours then 2 hourly for 2 hours then 4 hourly for 24 hours then Twice daily until discharge unless deviations from normal identified in which case medical review should be sought and a plan of care documented All observations should be documented on the MOEWs chart Any deviations from normal must be reported to the Obstetric and /or Anaesthetic staff 5.2 Thromboprophylaxis A thromboprophylaxis risk assessment should be carried out for all Caesarean sections and tinzaparin prescribed as necessary. For full details see Thromboprophylaxis in Pregnancy and the Puerperium. 5.3 Debriefing & Advice regarding future pregnancies It is good practice for the surgeon involved in delivery to see the woman post delivery to offer a chance to discuss intrapartum care. It is good practice to involve the consultant who was either responsible for antenatal care or who was involved intrapartum. Advice should be given before discharge about the implications for future pregnancies, particularly the mode of delivery (there are few absolute indications for a repeat 8 Caesarean section in a future pregnancy) and a patient information leaflet should be given. Details of these discussions should be documented in the birth record. It is also a good opportunity to offer advice in future pregnancies where interventions may be appropriate to reduce risk of recurrence of a particular problem. Whilst the majority of women will be seen for their postnatal check in the community, it may be appropriate to offer certain groups of women the opportunity of a consultant postnatal appointment. This should be discussed with the appropriate consultant and an appointment made with the consultant by the ward staff: Poor neonatal outcome or stillbirth Severely growth restricted baby or pre-eclampsia less than 34 weeks, consider screening for inherited thrombophilia Advice regarding prophylactic aspirin where indication for delivery has been severe pre-eclampsia Screening in a future pregnancy where there has been a preterm delivery (< 34 weeks gestation) – consider cervical screening, screening for infection, elective cervical stitch Staff debriefing may be appropriate especially where there has been a difficult delivery or unexpected complications. 6.0 MONITORING COMPLIANCE An audit will be carried out in accordance with the Maternity Services Audit Plan. Auditable standards include: - Indication for CS Grading of urgency of CS (classification) Involvement of Consultant in decision making process Time from decision to delivery and reason for delay if any Whether paired cord blood samples were taken as indicated Use of antibiotic prophylaxis and thromboprophylaxis Care of mother within first 24 hours Documented discussion with woman re implications for future pregnancies A continuous audit will be carried out on all category one caesarean sections whereby the delivery is entered onto a log kept on delivery suite. Every 24 hours, the coordinating midwife and the Consultant will review the notes and ensure that an audit form has been completed. If there was a delay in the decision to delivery interval or there are any adverse outcomes (e.g. low cord pH, unplanned admission to NNU etc) then the incident should be reported via the clinical incident reporting process (DATIX) and the case reviewed at the weekly risk management meeting. The Consultant and Co-ordinator are responsible for any immediate actions which should be documented on on DATIX Audit results will be presented twice a year at the Clinical Governance and Audit meeting and an action plan developed as necessary. A lead will be appointed to monitor the action plan and progress and updates of the action plan will be presented quarterly to the Women’s Services Clinical Governance and Risk Management forum. Results of the audit will be included in the quarterly Risk Management report and any subsequent changes will be disseminated via the Maternity Services Forum, Women’s Services Clinical Governance and Risk Management Forum, Team Leaders Forum and Supervisor of midwives Forum. 9 7.0 REFERENCES (1) NICE Clinical Guideline 13. Caesarean Section. April 2004. National Institute for Clinical Excellence. (2) ACOG Committee on Obstetric Practice. Obstet Gynecol. 2002 Apr;99(4):679-80. (3) Kieser KE, Baskett TF. A 10-year population-based study of uterine ruure. Obstet Gynecol. 2002 Oct;100(4):749-53. 7.0 PROVENANCE 7.1 Author(s): Tracey Glanville Consultant Obstetrician . 7.2 Objectives: The improve the provision of care for women undergoing emergency Caesarean section within the Leeds Teaching Hospitals NHS Trust. 7.3 Target Patient Group: All women undergoing emergency Caesarean section within the Leeds Teaching Hospitals NHS Trust. 7.4 Target Professional Group: All professionals undertaking maternity care at the Leeds Teaching Hospitals NHS trust 7.5 Person responsible for review: T Glanville (Consultant Obstetrician) 10 Protocol relating to the management of Caesarean section Author(s) T Glanville (Consultant Obstetrician SJUH) Contact name T Glanville (Consultant Obstetrician SJUH) Approval process for amendments Maternity Services Forum First Issue Date August 2008 Version no: 3.2 Review Date: August 2015 Clinical Guidelines Committee December 2009 (LHP version 1.0) Amendments approved by MSF 27/07/2012 (version 3.2) Ratified by Consultation Process Maternity Services Guideline Group / Maternity Services Forum, Maternity Services Clinical Governance and Risk Management Forum / Obstetricians / Team Leaders / Supervisors of Midwives Scope of guidance Clinical condition Patient Group Professional Group Distribution List All All pregnant women booked to deliver within the Leeds teaching Hospitals NHS Trust All Health Care Professionals involved in the provision of maternity care within the Leeds Teaching Hospitals NHS Trust All Obstetricians within the Women and Children's Division. Lead Clinician (Midwifery and Neonates) Head of Midwifery Matrons (midwifery and neonatal) Clinical Midwifery Team Leaders (for distribution to midwives within their areas) Dissemination Via Risk Management Midwife Audit and Monitoring Will be carried out in accordance with Maternity Services Audit Plan Broad Recommendations All pregnant women should be offered a high standard of care based on the best available evidence Equity and Diversity Leeds Teaching Hospitals NHS Trust believes in fairness, equity and above all values diversity in all dealings, both as providers of health services and employers of people. The Trust is committed to eliminating discrimination on the basis of gender, age, disability, race, religion, sexuality or social class. We aim to provide accessible services, delivered in a way that respects the needs of each individual and does not exclude anyone. By demonstrating these beliefs the Trust aims to ensure that it develops a healthcare workforce that is diverse, non discriminatory and appropriate to deliver modern healthcare. 11