姓名: 口:男 口:女
advertisement
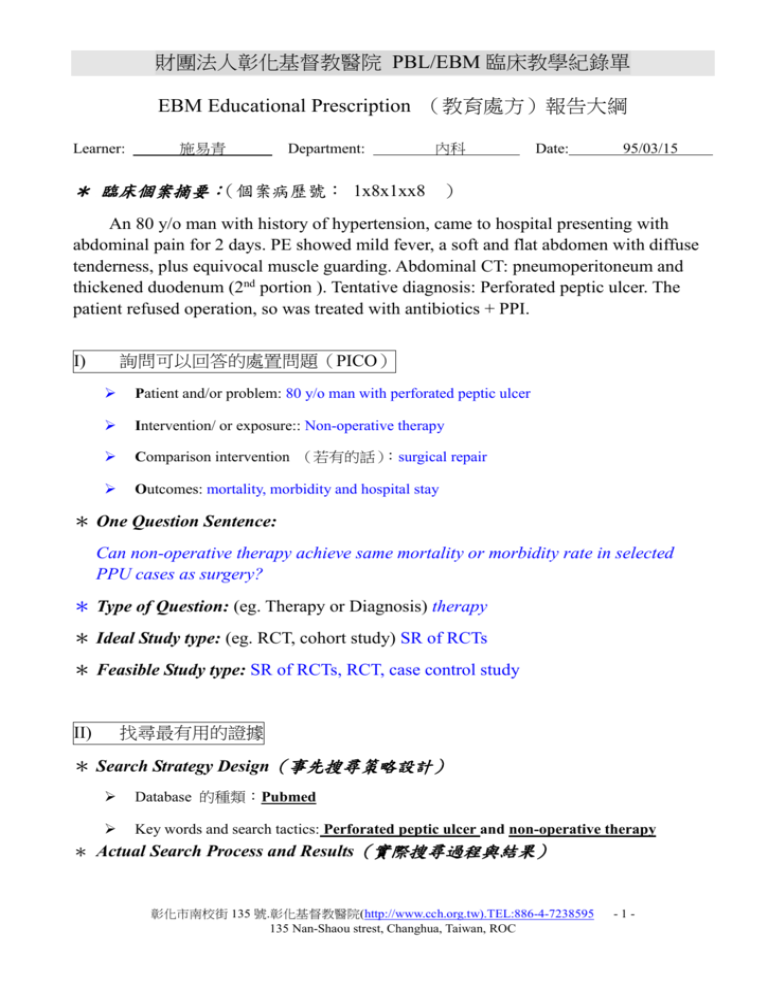
財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 EBM Educational Prescription (教育處方)報告大綱 Learner: 施易青 Department: 內科 Date: 95/03/15 * 臨床個案摘要:(個案病歷號: 1x8x1xx8 ) An 80 y/o man with history of hypertension, came to hospital presenting with abdominal pain for 2 days. PE showed mild fever, a soft and flat abdomen with diffuse tenderness, plus equivocal muscle guarding. Abdominal CT: pneumoperitoneum and thickened duodenum (2nd portion ). Tentative diagnosis: Perforated peptic ulcer. The patient refused operation, so was treated with antibiotics + PPI. 詢問可以回答的處置問題(PICO) I) Patient and/or problem: 80 y/o man with perforated peptic ulcer Intervention/ or exposure:: Non-operative therapy Comparison intervention (若有的話):surgical repair Outcomes: mortality, morbidity and hospital stay * One Question Sentence: Can non-operative therapy achieve same mortality or morbidity rate in selected PPU cases as surgery? * Type of Question: (eg. Therapy or Diagnosis) therapy * Ideal Study type: (eg. RCT, cohort study) SR of RCTs * Feasible Study type: SR of RCTs, RCT, case control study 找尋最有用的證據 II) * Search Strategy Design(事先搜尋策略設計) Database 的種類:Pubmed Key words and search tactics: Perforated peptic ulcer and non-operative therapy * Actual Search Process and Results(實際搜尋過程與結果) 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -1- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 #1 Search (perforated peptic ulcer OR perforation) AND (conservative OR nonsurgical OR nonoperative) 1137 #2 Search (perforated peptic ulcer ) AND (conservative OR nonsurgical OR nonoperative) 111 #3 Search (perforated peptic ulcer ) AND (conservative OR nonsurgical OR nonoperative) Field: All Fields, Limits: Publication Date from 1980 to 2006 81 #21 Select 11 document(s) 11 1: Clinical trail, level 5,對於哪些病人可使用非手術療法提出建議 Ann Chir. 2004 Dec;129(10):578-82. [Non operative treatment for perforated peptic ulcer: results of a prospective study] [Article in French] Songne B, Jean F, Foulatier O, Khalil H, Scotte M. BACKGROUND: The conservative management of perforated peptic ulcer has not gained widespread acceptance despite introduction of proton-pomp inhibitors because surgical procedures can achieve immediate closure by eventually using a laparoscopic approach. The aim of this prospective study was to evaluate the results of Taylor's method and to identify predictive factors of failure of medical treatment in patients presenting with perforated peptic ulcer. METHOD: Between 1990 and 2000, 82 consecutive patients, with diagnosis of perforated peptic ulcer were prospectively included in this study. They were initially treated with non-operative procedure (nasogastric suction and intravenous administration of H2-blockers or proton-pomp inhibitors). No clinical improvement after 24 hours required a surgical treatment. Predictive factors of failure of non-operative treatment were tested in univariate or multivariate analysis. RESULTS: Clinical improvement was obtained with non-operative treatment in 54% of the patients (44/82). The overall mortality rate was 1%. In univariate analysis, significant predictive factors of failure of non-operative treatment were: size of pneumoperitoneum, heart beat >94 bpm, abdominal meteorism, pain at digital rectal exam, and age >59 years. In multivariate analysis, the significant factors were the size of pneumoperitoneum, heart beat, and abdominal meteorism. The association of these criteria: size of pneumoperitoneum >size of the first lumbar vertebra, heart beat >94 bpm, pain at digital rectal exam and age > 59 years , led to surgical treatment in all cases. CONCLUSION: These results suggest that more than 50% of patients with perforated peptic ulcer respond to conservative treatment without surgery and that the association of few criteria (size of pneumoperitoneum, heart beat, pain at digital rectal exam and age) require emergency surgery. Levels of Evidence for Primary Research Question The Journal of Bone and Joint Surgery Levels of Evidence for Primary Research Question Types of Studies Therapeutic Studies—Investigating the Results of Treatment Prognostic Studies—Investigating the Effect of a Patient Diagnostic Studies—Investigating a Diagnostic Test Economic and Decision Analyses—Developing an Economic or Decision 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -2- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 Characteristic on the Outcome of Disease Level I High-quality randomized controlled trial with statistically significant difference or no statistically significant difference but narrow confidence intervals Systematic review2 of Level-I randomized controlled trials (studies were homogeneous) Level II Lesser-quality randomized controlled trial (e.g., <80% follow-up, no blinding, or improper randomization) Prospective4 comparative study5 Systematic review2 of Level-II studies or Level-I studies with inconsistent results Level III Case-control study7 High-quality prospective study4 (all patients were enrolled at the same point in their disease with ≥ 80% follow-up of enrolled patients) Systematic review2 of Level-I studies Retrospective6 study Untreated controls from a randomized controlled trial Lesser-quality prospective study (e.g., patients enrolled at different points in their disease or <80% follow-up) Case-control study7 Expert opinion Development of diagnostic criteria on basis of consecutive patients (with universally applied reference "gold" standard) Systematic review2 of Level-II studies Study of nonconsecutive patients (without consistently applied reference "gold" standard) Systematic review2 of Level-III studies Level V Systematic review2 of Level-I studies Sensible costs and alternatives; values obtained from many studies; multiway sensitivity analyses Systematic review2 of Level-I studies Sensible costs and alternatives; values obtained from limited studies; multiway sensitivity analyses Systematic review2 of Level-II studies Systematic review2 of Level-II studies Case series8 Testing of previously developed diagnostic criteria in series of consecutive patients (with universally applied reference "gold" standard) Retrospective6 comparative study5 Level IV Model Systematic review2 of Level-III studies Case series Expert opinion Case-control study Analyses based on limited alternatives and costs; poor estimates Systematic review2 of Level-III studies No sensitivity analyses Poor reference standard Expert opinion Expert opinion 1. A complete assessment of the quality of individual studies requires critical appraisal of all aspects of the study design. 2. A combination of results from two or more prior studies. 3. Studies provided consistent results. 4. Study was started before the first patient enrolled. 5. Patients treated one way (e.g., with cemented hip arthroplasty) compared with patients treated another way (e.g., with cementless hip arthroplasty) at the same institution. 6. Study was started after the first patient enrolled. 7. Patients identified for the study on the basis of their outcome (e.g., failed total hip arthroplasty), called "cases," are compared with those who did not have the outcome (e.g., had a successful total hip arthroplasty), called "controls." 8. Patients treated one way with no comparison group of patients treated another way. This chart was adapted from material published by the Centre for Evidence-Based Medicine, Oxford, UK. For more information, please see www.cebm.net. 外科有些分法比較適合外科例如下一篇可視為Retrospective6 comparative study5 2: Case report, level 4, level 3 也許可以算 Ceylon Med J. 2003 Jun;48(2):53-5. Experience of peptic ulcer perforation over a decade in a teaching hospital of southern Bangladesh. 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -3- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 Rahuman MM, Saha AK, Rahim A. OBJECTIVE: To determine disease characteristics, check the treatment status and compare outcome with other series. DESIGN AND SETTING: A retrospective study in a single unit of the Department of Surgery of Khulna Medical College Hospital, south west Bangladesh. PATIENTS AND METHODS: After diagnosis by clinical and radiological examination, 491 patients were treated during the period July 1992 to November 2002. Two options of treatment were carried out: simple closure and peritoneal lavage in 364 cases, and 127 patients managed by non-surgical methods. Main outcome measures: mortality and morbidities. RESULTS: Male:female ratio was 445:46, average age 43 years. Mortality in the surgical group was 6.8% and in the non-surgical group 0.02%. CONCLUSION: Perforated peptic ulcer is prevalent even after the wide use of H2 receptor antagonists. Strict case selection for surgical and non-surgical treatment has reduced mortality. These results support the case for non-operative treatment and for conservative surgery. 3: Review,原文為俄文,無法判斷是何種Review level of evidence 5 因為不是systematic review Voen Med Zh. 2000 Jul;321(7):24-9, 95. [Surgical treatment of perforated gastroduodenal ulcers in young persons] [Article in Russian] Efimenko NA, Briusov PG, Peregudov SI, Shafalinov VA. The knowledge of surgical tactics in treatment of ulcerous disease and its complications in young persons is of great practical importance for military health service. The problem of choice of surgical method in perforated gastroduodenal ulcers remains contradictory. Many authors draw attention to merits and demerits of both palliative and radical interventions. The long-term results of identical operations obtained by different authors often vary and not infrequently are quite opposite. The review of our and foreign literature concerning the surgical treatment of perforated gastroduodenal ulcers in the young patients shows that the unequivocal decision of this problem today is not available. Discussions about expediency to perform different interventions in the young patients are generally concentrated around the notions of "acute" and "chronic" ulcer. However both these categories are poorly defined because the criteria of their evaluation vary in different authors. Obviously the choice of surgical method in the young patients with perforated gastroduodenal ulcers should be based both on multi-factor analysis of anamnestic data, the patient's general state, intraoperative picture and on retrospective and prospective analysis of conservative treatment, its possibilities and efficiency, on the patient's opinion. The availability of technical possibilities to perform the operation and presence of the adequately trained surgeons are necessary. Publication Types: Review 4: Review, 但目的在比較simple closure和elective surgery,和我的設想不同 Langenbecks Arch Surg. 2000 Mar;385(2):84-96. 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -4- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 Surgical management of peptic ulcer disease today--indication, technique and outcome. Zittel TT, Jehle EC, Becker HD. MS: The current surgical management of peptic ulcer disease and its outcome have been reviewed. RESULTS: Today, surgery for peptic ulcer disease is largely restricted to the treatment of complications. In peptic ulcer perforation, a conservative treatment trial can be given in selected cases. If laparotomy is necessary, simple closure is sufficient in the large majority of cases, and definitive ulcer surgery to reduce gastric acid secretion is no longer justified in these patients. Laparoscopic surgery for perforated peptic ulcer has failed to prove to be a significant advantage over open surgery. In bleeding peptic ulcers, definitive hemostasis can be achieved by endoscopic treatment in more than 90% of cases. In 1-2% of cases, immediate emergency surgery is necessary. Some ulcers have a high risk of re-bleeding, and early elective surgery might be advisable. Surgical bleeding control can be achieved by direct suture and extraluminal ligation of the gastroduodenal artery or by gastric resection. Benign gastric outlet obstruction can be controlled by endoscopic balloon dilatation in 70% of cases, but gastrojejunostomy or gastric resection are necessary in about 30% of cases. CONCLUSIONS: Elective surgery for peptic ulcer disease has been largely abandoned, and bleeding or obstructing ulcers can be managed safely by endoscopic treatment in most cases. However, surgeons will continue to encounter patients with peptic ulcer disease for emergency surgery. Currently, laparoscopic surgery has no proven advantage in peptic ulcer surgery. Publication Types: Review 5: Review,與我的問題相關的只review了一個trial, 即下面第10篇的RCT World J Surg. 2000 Mar;24(3):299-306. Surgical treatment of complicated duodenal ulcers: controlled trials. Millat B, Fingerhut A, Borie F. Indications for surgery of duodenal ulcer (DU) have changed radically because of the efficacy of H(2)-antagonists, endoscopic procedures, and eradication of Helicobacter pylorus. The aim of this study was to analyze the current literature to determine if definitive surgery is still relevant for complicated DU (bleeding, perforation, gastric outlet obstruction). Two studies have compared early to late surgery in terms of bleeding. One recommended early surgery (significant reduction in mortality) in the elderly, but no statistically significant difference was found when analyzed with "intention to treat." In the other, mortality with early surgery was five times higher than with expectant therapy (when it was possible). Two studies comparing different surgical techniques for bleeding favored the radical procedure. Of at least 15 studies comparing endoscopic treatments, however, none has compared endoscopic therapy to surgical intervention for bleeding DU. One trial, comparing nonoperative to surgical treatment for perforation, found similar rates of morbidity, intraabdominal abscess, and mortality; but the hospital stay was longer (p < 0.001). Nonoperative treatment failed more often (p < 0.05) in patients over age 70. In three trials, postoperative morbidity (excepting wound 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -5- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 sepsis in one) was not significantly increased by definitive surgery, with less ulcer recurrence (p < 0.05) compared with simple closure. Laparoscopy (versus laparotomy) was shown to take longer (p < 0.001) but required less postoperative analgesics (p < 0.03); there were no statistically significant differences as concerns the duration of nasogastric aspiration, intravenous drips, hospital stay, time to resume normal diet, Visual Analogous Scale pain scores for the first 24 hours after surgery, morbidity, reoperation rate, or mortality. Of 48 laparoscopic patients, 11 (23%) underwent conversion to open surgery. Three surgical techniques [highly selective vagotomy (HSU) + gastrojejunostomy (group1), HSV + Jaboulay gastroduodenostomy (group 2), or selective vagotomy (group 3) + antrectomy) for gastric outlet obstruction (GOO)] showed that although postoperative results were similar (except wound sepsis in one trial), long-term Visick scores were significantly (p < 0.01) better in group 1 than in group 2, but not in group 3. Further studies are needed to determine the exact prevalence of Helicobacter pylori in complicated DU and to compare (1) definitive to minimal surgery (stop the bleeding or close the perforation) combined with antisecretory drugs and eradication of H. pylori; (2) surgery to endoscopic treatment combined with eradication of H. pylori; and (3) for GOO, surgery to balloon dilatation combined with eradication of H. pylori. Publication Types: Review 6: Case report, level 4 Schweiz Med Wochenschr Suppl. 1997;89:17S-19S. [Conservative treatment of gastroduodenal peptic ulcer perforations: indications and results] [Article in French] Alizadeh N, Buhler L, Huber O, Morel P. Surgery is the conventional form of treatment for perforated peptic ulcer. Conservative treatment has however been described, and is still used in rare situations. The present study analyzes the indications and results of conservative therapy in our hospital. Between 1978 and 1995, 332 patients were admitted for perforated peptic ulcer. Twelve (3.5%), with a mean age of 85 (67-93) years, underwent conservative treatment (gastric suction, H2-blockers and broad-spectrum antibiotics). The diagnosis was established on the basis of epigastric pain and the finding of a pleuriperitoneum on the plain film of the abdomen. The indication for conservative treatment was a prohibitive anesthesiological risk in 11 patients and absence of peritoneal sign in one. The evolution was favourable only in 4 patients, who were discharged after a median stay of 18 days. Mortality was 8/12 patients. In one of these, autopsy showed ischemic colonic perforation. Conservative treatment of perforated peptic ulcer is associated with very high mortality. The results suggest that frequent and careful clinical monitoring is essential during the first 24 hours. In the event of deterioration, surgery must be reconsidered. In addition, the diagnosis should be confirmed by ruling out perforation of another abdominal organ. 7: Case Reports, level 4 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -6- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 Khirurgiia (Sofiia). 1993;46(3):8-9. [Spontaneous recovery in perforated gastroduodenal ulcer. The indications for conservative treatment] [Article in Bulgarian] Two observations of patients, having perforated duodenal ulcer, not operated, where spontaneous recovery was achieved, have been reported. The said opportunity has been interpreted in connection with the accepted method for conservative treatment of gastroduodenal ulcer. The indications and the contraindications for the conservative treatment have been stated. Publication Types: Case Reports 8: Comment Lancet. 1990 Mar 17;335(8690):673. Conservative management of perforated peptic ulcer. Rigg KM, Stuart RC, Rosenberg IL. Publication Types: Comment 9: Case reports, level 4 Arch Surg. 1989 Jul;124(7):830-2. Nonoperative treatment of perforated duodenal ulcer. Berne TV, Donovan AJ. This report concerns 35 adult patients in whom perforation of a duodenal or prepyloric ulcer was treated nonoperatively between July 1979 and April 1988 at the Los Angeles County--University of Southern California Medical Center, Los Angeles. Each patient had pneumoperitoneum with clinical evidence of peritonitis, and a gastroduodenogram documented a sealed perforation. The ulcer was believed to be acute in 27 patients and chronic in 8. These 35 cases represent 12% of 294 cases of duodenal and prepyloric peptic ulcers with perforation treated during the same period. An intra-abdominal abscess developed in 1 of the 35 patients. Reperforation did not occur. The mortality rate for the 259 cases treated operatively during this period was 6.2%; the mortality rate of the 35 cases treated nonoperatively was 3%. Duodenal ulcer can be safely treated nonoperatively when a gastroduodenogram documents self-sealing. 10:Individual RCT, level 2b 個案數少 N Engl J Med. 1989 Apr 13;320(15):970-3. A randomized trial of nonoperative treatment for perforated peptic ulcer. Crofts TJ, Park KG, Steele RJ, Chung SS, Li AK. To determine whether surgery could be avoided in some patients with perforated peptic ulcer, we conducted a prospective randomized trial comparing the outcome of nonoperative treatment with that of emergency surgery in patients with a clinical diagnosis of perforated peptic ulcer. Of the 83 patients 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -7- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 entered in the study over a 13-month period, 40 were randomly assigned to conservative treatment, which consisted of resuscitation with intravenous fluids, institution of nasogastric suction, and intravenous administration of antibiotics (cefuroxime, ampicillin, and metronidazole) and ranitidine. Eleven of these patients (28 percent) had no clinical improvement after 12 hours and required an operation. Two of the 11 had a perforated gastric carcinoma, and 1 had a perforated sigmoid carcinoma. The other 43 patients were assigned to immediate laparotomy and repair of the perforation. One of these patients was found to have a perforated gastric carcinoma. The overall mortality rates in the two groups were similar (two deaths in each, 5 percent), and did not differ significantly in the morbidity (infection, cardiac failure, or renal failure) rates (40 percent in the surgical group and 50 percent in the nonsurgical group). The hospital stay was 35 percent longer in the group treated conservatively. Patients over 70 years old were less likely to respond to conservative treatment than younger patients (P less than 0.05). We conclude that in patients with perforated peptic ulcer, an initial period of nonoperative treatment with careful observation may be safely allowed except in patients over 70 years old, and that the use of such an observation period can obviate the need for emergency surgery in more than 70 percent of patients. Publication Types: Randomized Controlled Trial 11: Case reports, level 4 Acta Chir Scand. 1980;146(3):189-93. Conservative treatment of 155 cases of perforated peptic ulcer. Kristensen ES. During 23 years a total of 155 cases of verified perforated peptic ulcer were treated conservatively, according to the routine of the department, with a complication rate of 31%, and a mortality rate of 10%. Out of the 16 deaths, 4 patients were moribund at the admission, and 10 of the 12 remaining patients had a severe associated disease. Therefore, results of conservative treatment cannot be judged from results in this group. In fact, the overally mortality rate was not not higher in this material than usually reported after surgical intervention. Long-term results (mean 11 years) in 93 patients were satisfactory in 18 our of 28 patients with acute ulcer, and in 31 out of 65 patients with chronic ulcer. The reperforation rate was 9.7%.. * 描述自己如何從上述搜尋結果中,選出與問題相關之一些文獻,並將這些文獻 分出「初步證據等級」(請附上摘要),進而從中選一篇做為期刊閱讀的主要文 獻加以評判: 在此選擇第10篇的individual RCT來評判 III) 評判證據(critical appraisal) 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -8- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 請附上文獻全文,依據PICO問題的種類,選用適當之Users’ Guide,依照其設計 之問句,逐一回答,並標示出評判的重點處。以「Therapy」問題之文獻評論為例: * The validity of this evidence(證據之有效性) Were patients randomized ? yes Was randomization concealed? Yes, using sealed envelopes Were patients analyzes in the groups to which they were randomized? Yes, “intention to treat” principle Were patients in the Treatment and Control groups similar with respect to know prognostic factors? Yes, table 1 Were patients aware of group allocation? Yes, a surgery can’t be concealed Were Clinicians aware of group allocation? Yes, a surgery can’t be concealed Were outcome assessors aware of group allocation? Yes, a surgery can’t be concealed Aside from the experimental intervention, were groups treated equally? yes Were follow-up sufficiently long and complete? Yes, six weeks after discharge * The importance of this valid evidence (有效證據之重要性) How large was the treatment effect? With a careful observation period, nonoperative treatment did not lead to increased morbidity or mortality, except when the patient is over 70 years old. The hospital stay was longer in nonsurgical group, which may be due to a cautious attitude toward conservatively treated p’t rather than increased morbidity. How precise was the estimate of the treatment effect? Estimation of mortality was arguably imprecise due to the small case number and relatively low mortality rate (2 in each group). The morbidity rate, on the other hand, was more reliable. Discrepancy in the length of hospital stay was very precise (7.8 days vs 12.0 days). 沒有顯示CI只有P值。 IV) 如何應用到此臨床個案上 * Can this valid, important evidence be applied to your patient Were the study patients similar to the patient in my practice? Yes, they all have a firm clinical diagnosis of perforation. Were all clinically important outcomes considered? Pretty much so. Are the likely treatment benefits worth the potential harm and costs? Yes, but close monitoring of an experienced practitioner is needed. (應多描述一些,您的個案 80 歲,此研究好像 70 歲以上,不成功的機會較高,雖然 個案數不多,臨床上需考慮併發症) 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC -9- 財團法人彰化基督教醫院 PBL/EBM 臨床教學紀錄單 彰化市南校街 135 號.彰化基督教醫院(http://www.cch.org.tw).TEL:886-4-7238595 135 Nan-Shaou strest, Changhua, Taiwan, ROC - 10 -