Robotic radical prostatectomy: perioperative, pathologic and
advertisement
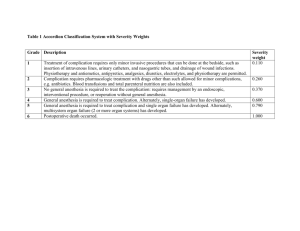
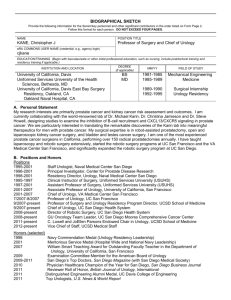
Robotic radical prostatectomy: perioperative, pathologic and functional outcomes in a low volume center Gianluca D'Elia, Paolo Emiliozzi, Gianfranco Ortolani, Antonio Iannello, Ospedale San Giovanni, Roma, Italy Reports of high-volume centers with robotic radical prostatectomy are readily available. However, evaluation of functional and oncological outcome as well as complications from low-caseload centers is lacking. We report on our experience in a community setting low-volume center (less than 85 procedures / year). A total of 282 patients underwent robotic radical prostatectomy during a 42-month period. Two surgeons performed all the procedures. The senior surgeon proctored the junior surgeon after the first 50 cases utilizing a step-by-step approach. Perioperative data and functional and pathological results were prospectively collected. Perioperative outcome measures included: operative time, estimated blood loss, transfusion rate, complication rate according to modified Clavien system, median hospital stay, mean catheterization time. Pathologic outcome measures encompassed positive surgical margin rate and biochemical recurrence free survival (PSA < 0.2). Perioperative and pathologic outcomes were also analyzed using prostate weight as a continuous variable by multivariate regression. Return of continence was evaluated at 1, 3, 6 and 12 months (continent 0 pads; incontinent 1 or more pads). Return of potency was evaluated at 1, 3, 6 and 12 months with IIEF-5 scores in 178 patients who underwent a nerve-sparing procedure (mean age 61 years; range 47 - 67). Mean age was 64.2 years. Mean body mass index (BMI) was 26.6. Median preoperative PSA level was 7.6 ng/ml. Mean operative time was 158 minutes. Mean estimated blood loss was 180 cc. Blood transfusion was needed in 3 patients. Median hospital stay was 4 days, mean catheterization time was 8.4 days. According to the modified Clavien system, grade III complication rate was 2.6 %, whereas minor complication rate was 22%. Positive surgical margin rate was 9.8 % for pT2 disease and 29 % for pT3 disease. Mean prostate weight was 53 g. No correlation between prostate weight, perioperative outcomes and positive margins was found at the multivariate regression analysis (p > 0,5). Overall biochemical recurrence free survival is 95% at mean follow up of 10.9 months. Complete continence (pad free) at 1, 3, 6, and 12 months was 57%, 88%, 94% and 98%, respectively. At 1, 3, 6 and 12 months return of potency (IIEF-5 > 21) with or without the use of oral medications was achieved in 6%, 22%, 51% and 68%, respectively. Robotic radical prostatectomy has a low perioperative complication rate and acceptable pathologic and functional outcomes despite a limited caseload. Two surgeons accomplished their learning curve within 100 cases without posing outcomes at risk. Perioperative and pathologic outcomes seem to be unrelated to prostate weight. Finanziamento No Conflitto d'Interesse No Argomento Oncologia Prostata