Guidelines on Consent Forms
advertisement
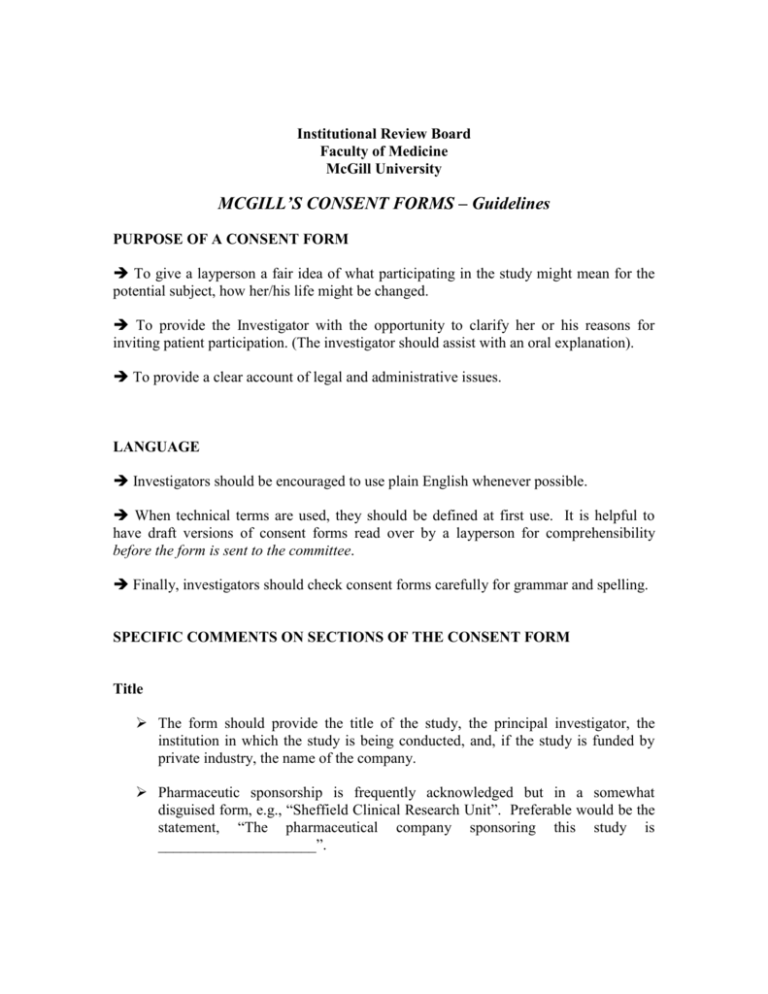
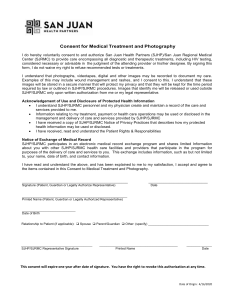
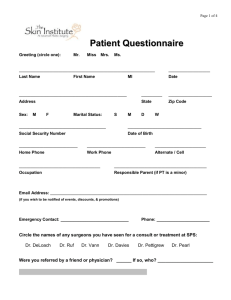
Institutional Review Board Faculty of Medicine McGill University MCGILL’S CONSENT FORMS – Guidelines PURPOSE OF A CONSENT FORM To give a layperson a fair idea of what participating in the study might mean for the potential subject, how her/his life might be changed. To provide the Investigator with the opportunity to clarify her or his reasons for inviting patient participation. (The investigator should assist with an oral explanation). To provide a clear account of legal and administrative issues. LANGUAGE Investigators should be encouraged to use plain English whenever possible. When technical terms are used, they should be defined at first use. It is helpful to have draft versions of consent forms read over by a layperson for comprehensibility before the form is sent to the committee. Finally, investigators should check consent forms carefully for grammar and spelling. SPECIFIC COMMENTS ON SECTIONS OF THE CONSENT FORM Title The form should provide the title of the study, the principal investigator, the institution in which the study is being conducted, and, if the study is funded by private industry, the name of the company. Pharmaceutic sponsorship is frequently acknowledged but in a somewhat disguised form, e.g., “Sheffield Clinical Research Unit”. Preferable would be the statement, “The pharmaceutical company sponsoring this study is _____________________”. Introduction State clearly what disease is being studied and why the subject is being approached. Explain, as appropriate, how the condition is usually treated and why this particular study is being done. If the study involves adding a particular experimental treatment to standard therapy, e.g., testing whether the addition of radiation therapy to standard chemotherapy is of benefit, the introduction should explain the following: ־ ־ ־ how the disease is usually treated what procedures are involved in standard treatment what the risks and benefits of standard treatment are why the study is adding an experimental treatment on top of standard treatment (e.g., “despite the observed efficacy of chemotherapy, many patients experience local recurrences post-treatment”) Subjects should be given some information on the testing experience with the new treatment date, including the number of patients treated and the response rate observed. The last sentence of the introduction should clearly and honestly state the purpose of the study. If the study is looking at the benefit of adding a treatment to standard therapy, this should be reflected in the statement of purpose (e.g., “The purpose of this study is to see if the risks of adding radiation therapy to standard treatment are outweighed by the benefits”). Investigators should be careful to ensure that statement of purpose is accurate. If the purpose of the trial (and this means the primary outcome of the study) is to measure toxicity or costeffectiveness, this must be clearly stated. In phase I trials, the consent needs to be cohort specific, i.e., the subject needs to be informed what dose level she/he is being entered in and, in more general terms, about the relationship between dose and benefits / side effects. Study Procedures Since procedures relating to standard therapy, if applicable, will have been explained above, the study procedures section should clearly describe the therapeutic and non-therapeutic experimental procedures involved in the study. There must be a clear indication of which procedures are being done for therapeutic reasons and which are non-therapeutic, that is, done to answer the research questions rather than treat the patient. In most cases, it will be clearest to provide subjects with a chronological account of the procedures involved. It is important for the procedures to be sufficiently explained so that a layperson can have some idea of what is involved. How much time will each treatment take? Non-therapeutic procedures (including additional blood draws, x-rays, and questionnaires) should be set out in a separate paragraph. The form should clearly state how many of these procedures are involved and why they are being done. If the study places restrictions on other treatments that the patient may receive (concomitant treatments such as steroids, antiemetics, and growth factors), these restrictions must be clearly stated and justified. Benefits and Risks The anticipated benefits of study participation should be stated in an even-handed manner; both excessive pessimism and undue optimism are to be avoided. For example, if the hoped-for benefit is a reduction in the probability of a local recurrence, this should be plainly stated. If there are no benefits for the individual participant, hoped-for benefits to others afflicted with the disease may be pointed out. The law requires that risks to research subjects be fully disclosed. The risks in the consent form should mirror the risks disclosed in the protocol. When a study involves a component of standard therapy, the risks of that therapy ought to have been disclosed in the introduction. The risks section should focus on the incremental risks associated with study participation. In the example of a study looking at adding radiation therapy to standard chemotherapy, the risks associated with radiation therapy ought to be detailed here plus the risks association with combining two therapies (i.e., the risk of additive toxicity). A “drop in blood counts” does not constitute a fully disclosed risk; what this means for the patient must be explained. It is helpful to divide risks quantitatively, e.g., ־ ־ ־ ־ rare risks (less than 2%) uncommon risks (2-10%) frequent risks (11-30%) expected risks (31%+) If there is little experience with a new treatment or a new combination of treatments, it is important to state this and that unexpected side-effects may be seen. Side-effects that may not be reversible must be clearly identified as such. Subjects should be warned to look out for early symptoms and signs of serious or life threatening side effects (e.g. mouth sores or fever in the context of chemotherapy) and be told to immediately report these to the investigator. Withdrawal from Study If applicable, the conditions under which a subject may be withdrawn from a study ought to be clearly laid out. Alternative Treatments It is rare indeed for a consent form to provide an adequate explanation of alternative treatments. A statement that “your doctor will explain other treatments available” is unacceptable; so, too, a statement of the form, “other treatments for your disease include surgery, chemotherapy and radiation therapy”, is never sufficient. Patients should be clearly told what the standard treatment or treatments for their condition is. It would be helpful to provide some idea of what the basic difference between these treatments are. If the patient has advanced cancer, the option of supportive care, including details on comfort control measures, must be detailed. Cost / Insurance If there are any costs to the research participants, these should be clearly outlined. Some studies, particularly those funded by drug companies, have no-fault insurance coverage. If the study has such a policy, it should be briefly explained. If no such policy exists, the section should be left out. Compensation Details regarding compensation should not be listed under study benefits. Subjects should be informed of the amount of compensation and how this has been calculated. Subjects who withdraw early may not be penalized for doing so and must receive compensation proportionate to their time in the study. Subject Rights Detail the rights of research subjects, including ־ the right to ask questions at any time ־ the fact that study participation is voluntary ־ the fact that refusal to participate will involve no penalty or loss of benefits to which the subject is otherwise entitled ־ the right to discontinue participation at any time without penalty or loss of benefits to which the subject is otherwise entitled. Confidentiality Subjects should be told who will have access to their medical information, including Therapeutic Products Directorate (TPD) or the Food and Drug Administration (FDA). Steps taken to protect the confidentiality of the subjects’ medical information should be briefly described. Contact The subject should be told who to contact regarding their rights (e.g., patient representative). The subjects should be told who to contact in the event of an adverse event (e.g., the study investigator). Signature The final portion of the form should include a statement to the effect of “The study has been explained to me and my questions have been answered to my satisfaction. I agree to participate in this study. I do not waive any of my rights by signing this consent.” The phrase “I understand” is to be avoided. Subjects should be told that they will be given a copy of the form. The signature should be witnessed by someone not directly associated with the study who has witnessed the consent negotiation.