High-Tech Diagnostic Tools for the Modern Optometrist
advertisement

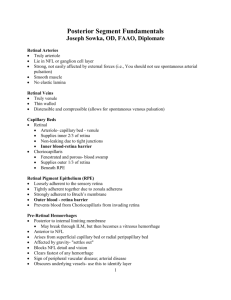
High-Tech Diagnostic Tools for the Optometrist Sherry J. Bass, OD, FAAO Jerome Sherman, OD, FAAO Scanning Laser Tomography (HRT) • • • • • Uses a confocal laser scanning system – 670 nm diode laser Objects are scanned sequentially in two dimensions (optic sections) Sections are imaged layer by layer to form a three-dimensional image Provides three-dimensional imaging of the optic nerve head Provides objective information about macular thickening -Useful in the objective detection of CSME and in edema secondary to vaso-occlusive disease HRT • • • • The series begins with the focal plane located in the vitreous Focal plane moves posteriorly through the optic nerve head until it reaches the retina 32 confocal 2-D images are obtained in 1.6 sec. A matrix is constructed consisting of 256X256 (65,536) height measurements (measuring points) • Each height is represented as a color – bright=excavated areas (cup) – dark= elevated areas (retina) Applications of Optic Nerve Head Topography • • Quantitative description and classification at first visit and change over time Stereometric parameters – disk area – cup and rim area and volume – mean and maximum cup depth – cup shape-the more negative value the better – RNFL thickness (along the edge of disk) Optical Coherence Tomography (OCT), Humphrey Instruments • Principles – Infrared light (850 nm) from a diode is directed into the retina – Backscattered light is detected and resolved using Low Coherence Interferometry to produce high resolution cross sections of the retina – looks like a histological slide section of the retina OCT • • • • Non-contact, non-invasive Operates like a slit lamp Images aquired in 2.5 sec. Quantifiable results OCT • Clinical Applications – Increases in retinal thickness secondary to vascular disease and veno-occlusive disease – Retinal elevations (serous retinal detachment) – Detection and assessment of macular hole, macular cyst, CME, CSME – Juxtapapillary nerve fiber layer loss or thinning (3.4mm circular scan) Scanning Laser Polarimetry (GDx), Laser Diagnostic, Inc • Principles – Uses birefringence or polarization to measure the thickness of the nerve fiber layer – Birefringent (layered) structures in eye • cornea (lamellae) • lens • retina (NFL) – To isolate NFL birefringence, GDx uses a corneal compensator; lens has minimal birerefringence Scanning Laser Polarimetry (GDx) • Measures the thickness of the retinal NFL (65,536 points) in an area 15 degrees X 15 degrees around the optic nerve head by measuring the degree of birerefringence or polarization (retardation) – the thicker and more robust the NFL, the greater the birefringence GDx: Screening for NFL Loss • • Images acquired in 0.7 sec.;pupil dilation NOT necessary Sensitivity-96%; Specificity-93% – Hans Lemij,MD • Total chair time: 3 minutes • Thickness Map – Bright colors: thicker areas of NFL • superior and inferior to ONH – Dark colors: thinner areas of NFL • • nasal and temporal to ONH defects in NFL sup/inf Parameters Most Effective for Differentiation of Normal vs Gl • • • • • Symmetry of various quadrant ratios – sup/temp ratio vs. inf/temp ratio NFL integral, or total area NFL thickness above the blood vessels Absolute thickness of all 65,536 points Total volume of the NFL GDx: The “Number” • NFL mesaurements are assigned a “number” between 0 and 100 • The number is assigned by looking at many of the values obtained when an image is aquired. • General Categories: – 0-30: Normal 31-60: Gl suspect 62-100: Gl • The number is a guide but one also needs to look at subtle changes in the fundus image-similar to focal defects in VF when mean deviation is normal GDx: Analyses • Glaucoma Analysis – fundus image, thickness map, TSNIT curve of one eye and one exam • Symmetry Analysis – prints both eyes on one page • Serial Analysis – displays up to 4 images per eye on one page-for follow-up • Sector Analysis – Evaluates thickness measurements in 36 sectors around the optic nerve head Pulsatile Ocular Blood Flow • Ocular blood flow analysis is now recognized as an important diagnostic tool in the detection and monitoring of glaucoma – Studies have demonstrated • a vascular etiology of normotensive glaucoma • a relationship between pulsatile ocular blood flow (POBF) and visual field loss – Most of the circulation to the ONH is supplied by the short posterior ciliary arteries (SPCA’s) Non-Invasive Clinical Methods of Assessing Ocular Blood Flow • Flowmetry (Heidelberg Retinal Flowmeter) – – – Measures flow rate and number of moving corpuscles, volume and velocity in the retinal and ONH capillary beds Uses principle of laser Doppler frequency shifts to measure the amount and velocity of moving red blood cells in a two-dimensional array Produces perfusion “maps” Non-Invasive Clinical Methods of Assessing Ocular Blood Flow • Ocular pulsatility (The Ocular Blood Flow Tonometer) – measures pulsatile inflow volume in microliters/sec- predominantly choroidal flow – uses as a basis of measurement IOP variation during the cardiac cycle When is Blood Flow Measurement Indicated? • On an initial visit of a patient with normal IOPs, abnormal cupping and visual field defect • On an initial visit of a patient with normal IOP and asymmetric cupping • To follow the normotensive glaucoma patient or suspect over time • Research is currently addressing which glaucoma drugs are best for regulating blood flow to the ONH