MAKING A MEDICAL DIAGNOSIS
advertisement
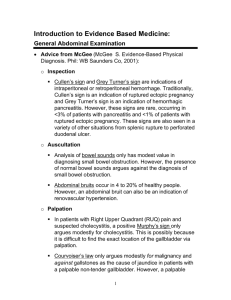
MAKING A MEDICAL DIAGNOSIS Bates, Barbara, A Guide to Physical Examination and History Taking, J.B. Lippincott Company, Philadelphia, PA, 1995. A person experiencing serious symptoms usually seeks professional help and thereby becomes a patient. The clinician, whether a nurse, physician, or emergency medical technician, must determine the need for medical care on the basis of observation and assessment of the patient’s symptoms and signs. This is the process of diagnosis: the identification of a pathological process by its characteristic symptoms and signs. Diagnosis is a lot like assembling a jigsaw puzzle. The more pieces (clues) available, the more complete the picture will be. The process of diagnosis is one of deduction and follows an orderly sequence of steps: 1. Obtain the patient’s medical history. The medical history is a concise summary of the present illness, past medical disorders, the health of the patient’s family, the psychosocial history, and general factors that may affect the function of body systems. The examiner gains information about the person’s concerns by asking specific questions and using good listening skills. Physical assessment begins here, and this is the time for unspoken questions such as, “Is this person moving, speaking, and thinking normally?” The answers will later be integrated with the results of more-precise observations. 2. Perform a physical examination. The physical examination is a basic but vital part of the diagnostic process. The common techniques used in physical examination include inspection (vision), palpation (touch), percussion (tapping and listening), and auscultation (listening). Certain vital functions are also checked. 3. If necessary, perform diagnostic procedures. The physical examination alone may not provide enough information to permit a precise diagnosis. Diagnostic procedures can then be used to focus on abnormalities revealed by the physical examination. For example, if the chief complaint is knee pain after a fall and the physical examination reveals swelling and localized, acute pain on palpation, the preliminary diagnosis may be a torn cartilage. An X-ray or MRI scan or both may be performed to ensure that there are no torn ligaments. With the information the diagnostic procedure provides, the final diagnosis can be made with reasonable confidence. Diagnostic procedures thus extend, rather than replace, the physical examination. COMPREHENSIVE HISTORY Patient Name: Date of History: Identifying Data: age, sex, race, place of birth, marital status, occupation, religion. Source of Referral: if any, and the purpose of it. Source of History: such as the patient, a relative, a friend, the patient’s medical record, or a referral letter. Reliability: if relevant. (of patient interview, often based on level of coherence) Chief Complaint: when possible, in the patient’s own words. Present Illness: A clear, chronological account of the problems for which the patient is seeking care. Should include the onset of the problem, the setting in which it developed, its symptoms, and any treatments. Principal symptoms should be described in terms of 1) location, 2) quality, 3) quantity or severity, 4) timing (i.e., onset, duration, and frequency), 5) the setting in which they occur, 6) factors that have aggravated or relieved them, and 7) associated manifestations. Also significant negatives (the absence of certain symptoms that will aid in a differential diagnosis). A present illness should also include patients’ responses to their own symptoms and incapacities. What does the patient think has caused the problem? What are the underlying worries that have led to seeking professional attention? (“I think I may have appendicitis.”) And why is that a worry? (“My Uncle Charlie died of a ruptured appendix.”) Further, what effects has the illness had on the patient’s life? This question is especially important in understanding a patient with chronic illness. “What can’t you do now that you could do before? How has the backache, shortness of breath, or whatever, affected your ability to work?...your life at home?...your social activities?...your role as a parent?...your role as a husband, or wife?...the way you feel about yourself as a man or woman?” PAST HISTORY General State of Health: as the patient perceives it. Childhood Illnesses: such as measles, rubella, mumps, whooping cough, chickenpox, rheumatic fever, scarlet fever, polio. Adult Illnesses Psychiatric Illnesses Accidents and Injuries Operations Hospitalizations not already described Current Health Status Current Medications Allergies Tobacco, Alcohol, Drugs, and Related Substances: including type, amount, duration of use, e.g., cigarettes, a pack a day for 12 years. Diet: including usual daily intake and any dietary restrictions or supplements. Ask about coffee, tea, cola drinks, and other caffeine-containing beverages. Screening Tests: appropriate to the patient, such as TB tests, Pap smears, mammograms, stools for occult blood, and cholesterol tests, together with the results and the dates they were last performed. Immunizations: such as tetanus, pertussis, diphtheria, polio, measles, rubella, mumps, influenza, hepatitis B, pneumoccal vaccine. Sleep Patterns: including times that the person goes to bed and awakens, daytime naps, and any difficulties in falling asleep or staying asleep. Exercise and Leisure Activities: Environmental Hazards: including those in the home school, and workplace Use of Safety Measures: such as seat belts, smoke detectors, and other devices related to specific hazards. FAMILY HISTORY The age and health, or age and cause of death, of each immediate family member. The occurrence within the family of any of the following conditions: diabetes, heart disease, hypercholesterolemia, high blood pressure, stroke, kidney disease, tuberculosis, cancer, arthritis, anemia, allergies, asthma, headaches, epilepsy, mental illness, alcoholism, drug addiction, and symptoms like those of the patient. PSYCHOSOCIAL HISTORY Captures important and relevant information about the patient as a person. Home Situation and Significant Others Daily Life Important Experiences: including upbringing, schooling, military service, job history, financial situation, marriage, recreation, retirement. Religious Beliefs: relevant to perceptions of health, illness, and treatment. The Patient’s Outlook: on the present and on the future REVIEW OF SYSTEMS General: Usual weight, recent weight change, any clothes that fit tighter or looser than before. Weakness, fatigue, fever. Skin: Rashes, lumps, sores, itching, dryness, color change, changes in hair or nails Head: Headache, head injury Eyes: Vision, glasses or contact lenses, last eye examination, pain, redness, excessive tearing, double vision, blurred vision, spots, specks, flashing lights, glaucoma, cataracts Ears: Hearing, tinnitus, vertigo, earaches, infection, discharge. If hearing is decreased, used of hearing aids Nose & Sinuses: Frequent colds; nasal stuffiness, discharge, or itching; hay fever, nosebleeds, sinus trouble Mouth & Throat: Condition of teeth and gums, bleeding gums, dentures, if any, and how they fit, last dental examination, sore tongue, dry mouth, frequent sore throats, hoarseness Neck: Lumps, “swollen glands,” goiter, pain or stiffness in the neck Breasts: Lumps, pain or discomfort, nipple discharge, self-examination Respiratory: Cough, sputum (color, quantity), hemoptysis, wheezing, asthma, bronchitis, emphysema, pneumonia, tuberculosis, pleurisy; last chest x-ray film Cardiac: Heart trouble, high blood pressure, rheumatic fever, heart murmurs; chest pain or discomfort, palpitations; dyspnea, orthopnea, paroxysmal nocturnal dyspnea, edema; past electrocardiogram or other heart test results Gastrointestinal: Trouble swallowing, heartburn, appetite, nausea, vomiting, regurgitation, vomiting of blood, indigestion. Frequency of bowel movements, color and size of stools, change in bowel habits, rectal bleeding or black tarry stools, hemorrhoids, constipation, diarrhea. Abdominal pain, food intolerance, excessive belching or passing gas. Jaundice, liver or gallbladder trouble, hepatitis Urinary: Frequency of urination, polyuria, nocturia, burning or pain on urination, hematuria, urgency, reduced caliber or force of the urinary stream, hesitancy, dribbling, incontinence; urinary infections, stones Genital Male: Hernias, discharge from or sores on the penis, testicular pain or masses, history of sexually transmitted diseases and their treatments. Sexual preference, interest, function, satisfaction, and problems Female: Age at menarche; regularity, frequency, and duration of periods; amount of bleeding, bleeding between periods or after intercourse, last menstrual period; dysmenorrheal, premenstrual tension; age at menopause, menopausal symptoms, postmenopausal bleeding. Discharge, itching, sores, lumps, sexually transmitted diseases and their treatments. Number of pregnancies, number of deliveries, number of abortions (spontaneous and induced); complications of pregnancy; birth control methods. Sexual preference, interest, function, satisfaction; any problems, including dysparenia Peripheral Vascular: Intermittent claudication, leg cramps, varicose veins, past clots in the veins Musculoskeletal: Muscle or joint pains, stiffness, arthritis, gout, backache. If present, describe location and symptoms (e.g., swelling, redness, pain, tenderness, stiffness, weakness, limitation of motion or activity). Neurologic: Fainting, blackouts, seizures, weakness, paralysis, numbness or loss of sensation, tingling or “pins and needles,” tremors or other involuntary movements Hematologic: Anemia, easy bruising or bleeding, past transfusions and any reactions to them Endocrine: Thyroid trouble, heat or cold intolerance, excessive sweating; diabetes, excessive thirst or hunger, polyuria Psychiatric: Nervousness, tension, mood including depression; memory PHYSICAL EXAMINATION Inspection is careful observation. A general inspection involves examining body proportions, posture, and patterns of movements. Local inspection is the examination of sites or regions of suspected disease. Of the four components of the physical exam, inspection is often the most important because it provides the largest amount of useful information. Many diagnostic conclusions can be made on the basis of inspection alone; most skin conditions, for example, are identified in this way. A number of endocrine problems and inherited metabolic disorders can produce subtle changes in body proportions that can be detected by the trained eye. Inspection can allow for identification of any deformities, asymmetry, or inflammation. In palpation, the clinician uses hands and fingers to feel the body. This procedure provides information on skin texture and temperature, the presence of abnormal tissue masses, the pattern of the pulse, and the location of tender spots. Once again, the procedure relies on an understanding of normal anatomy. In one spot, a small, soft, lumpy mass is a salivary gland; in another location it could be a tumor. A tender spot is important in diagnosis only if the observer knows what organs lie beneath it. Palpation can help determine the borders of the heart, as well as the presence of an enlarged liver, spleen, or kidney. Percussion is tapping with the fingers or hand to obtain information about the densities of underlying tissues. Percussion helps to determine whether the underlying tissues are air-filled, fluid-filled, or solid. For example, when tapped, the chest normally produces a hollow sound, because the lungs are filled with air. That sound changes in pneumonia, when the lungs contain large amounts of fluid. To get the clearest chest percussion, the fingers must of course be placed in the right spots. Percussion techniques are also use to determine the borders of various organs (such as the spleen and liver). Flat (most dense), dull, resonant, hyperresonant, and tympanic (least dense) are the percussion “notes”. An example location (if you would like to test these sounds) for “flatness” is the thigh; dullness—the liver; resonance—the normal lung; hyperresonance—none normally (but present in cases of emphysema and pneumothorax); and tympany— gastric air bubble or puffed-out cheek. In a physical examination, the clinician may percuss the abdomen lightly in all four quadrants to assess the distribution of tympany and dullness. Tympany usually predominates because of gas in the gastrointestinal tract, but scattered areas of dullness due to fluid and feces there are also typical. Large dull area in the abdomen may indication the presence of an underlying mass or an enlarged organ, and this observation would help guide with a subsequent palpation. Auscultation is listening to body sounds, typically using a stethoscope. This technique is particularly useful for checking the condition of the lungs during breathing. The wheezing sound heard in people with asthma is caused by constriction of the airways, and pneumonia produces a gurgling sound, indicating that fluid has accumulated in the lungs. Auscultation is also important in diagnosing heart conditions. Many cardiac problems affect the sound of the heartbeat or produce abnormal swirling sounds during blood flow. Every examination also includes measurements of certain vital body functions, including body temperature, blood pressure, respiratory rate and heart (pulse) rate. The results, called vital signs, are recorded on the patient’s chart. As we noted earlier, each of these values can vary over a normal range that differs according to the age, gender, and general condition of the individual. The table below indicates the representative ranges for vital signs in infants children and adults. Normal Range of Values for Resting Vital Sign Infant (3 months) 90/50 Blood Pressure (mm/hg) 30-50 Respiratory Rate (per minute) 70-170 Pulse Rate (per minute) Individuals by Age Child (10 years) 125/60 Group Adult 95/60 to 140/90 18-30 8-18 70-110 50-95 DIAGNOSTIC PROCEDURES There are two general categories of diagnostic procedures: 1. Tests performed on the individual, generally within a hospital facility. A. Visualize internal structures (endoscopy, X-rays, scanning procedures, ultrasonography, mammography) B. Monitor physiological processes (EEG, ECG, PET, RAI, pulmonary function tests) C. Assess the patient’s homeostatic responses (stress testing, skin tests) 2. Tests performed in a clinical laboratory on tissue samples, body fluids, or other materials collected from the patient.