CLINICAL INDICATIONS:
advertisement
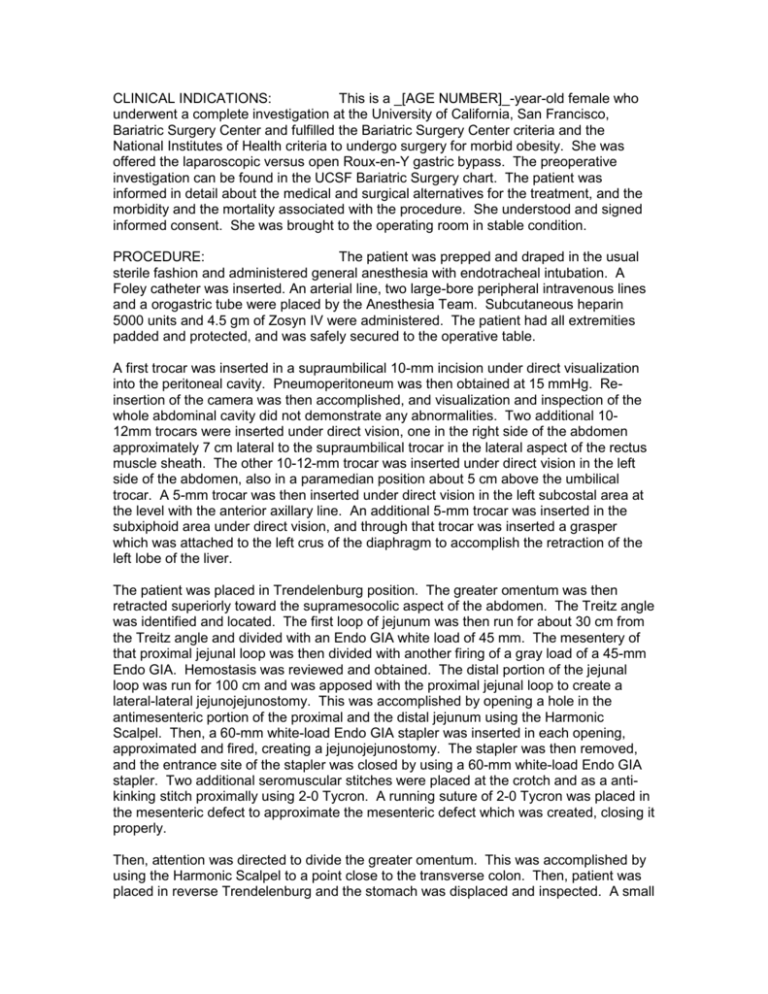
CLINICAL INDICATIONS: This is a _[AGE NUMBER]_-year-old female who underwent a complete investigation at the University of California, San Francisco, Bariatric Surgery Center and fulfilled the Bariatric Surgery Center criteria and the National Institutes of Health criteria to undergo surgery for morbid obesity. She was offered the laparoscopic versus open Roux-en-Y gastric bypass. The preoperative investigation can be found in the UCSF Bariatric Surgery chart. The patient was informed in detail about the medical and surgical alternatives for the treatment, and the morbidity and the mortality associated with the procedure. She understood and signed informed consent. She was brought to the operating room in stable condition. PROCEDURE: The patient was prepped and draped in the usual sterile fashion and administered general anesthesia with endotracheal intubation. A Foley catheter was inserted. An arterial line, two large-bore peripheral intravenous lines and a orogastric tube were placed by the Anesthesia Team. Subcutaneous heparin 5000 units and 4.5 gm of Zosyn IV were administered. The patient had all extremities padded and protected, and was safely secured to the operative table. A first trocar was inserted in a supraumbilical 10-mm incision under direct visualization into the peritoneal cavity. Pneumoperitoneum was then obtained at 15 mmHg. Reinsertion of the camera was then accomplished, and visualization and inspection of the whole abdominal cavity did not demonstrate any abnormalities. Two additional 1012mm trocars were inserted under direct vision, one in the right side of the abdomen approximately 7 cm lateral to the supraumbilical trocar in the lateral aspect of the rectus muscle sheath. The other 10-12-mm trocar was inserted under direct vision in the left side of the abdomen, also in a paramedian position about 5 cm above the umbilical trocar. A 5-mm trocar was then inserted under direct vision in the left subcostal area at the level with the anterior axillary line. An additional 5-mm trocar was inserted in the subxiphoid area under direct vision, and through that trocar was inserted a grasper which was attached to the left crus of the diaphragm to accomplish the retraction of the left lobe of the liver. The patient was placed in Trendelenburg position. The greater omentum was then retracted superiorly toward the supramesocolic aspect of the abdomen. The Treitz angle was identified and located. The first loop of jejunum was then run for about 30 cm from the Treitz angle and divided with an Endo GIA white load of 45 mm. The mesentery of that proximal jejunal loop was then divided with another firing of a gray load of a 45-mm Endo GIA. Hemostasis was reviewed and obtained. The distal portion of the jejunal loop was run for 100 cm and was apposed with the proximal jejunal loop to create a lateral-lateral jejunojejunostomy. This was accomplished by opening a hole in the antimesenteric portion of the proximal and the distal jejunum using the Harmonic Scalpel. Then, a 60-mm white-load Endo GIA stapler was inserted in each opening, approximated and fired, creating a jejunojejunostomy. The stapler was then removed, and the entrance site of the stapler was closed by using a 60-mm white-load Endo GIA stapler. Two additional seromuscular stitches were placed at the crotch and as a antikinking stitch proximally using 2-0 Tycron. A running suture of 2-0 Tycron was placed in the mesenteric defect to approximate the mesenteric defect which was created, closing it properly. Then, attention was directed to divide the greater omentum. This was accomplished by using the Harmonic Scalpel to a point close to the transverse colon. Then, patient was placed in reverse Trendelenburg and the stomach was displaced and inspected. A small window at just above the level of the incisura angularis was created to access the lesser sac by using the Harmonic Scalpel. Then, an Endo GIA 45-mm blue load was inserted in that window, and the stomach was transected approximately 7 cm from the gastroesophageal junction horizontally. Then, two loads of a 60-mm stapler blue-load Endo GIA were inserted to create a small gastric pouch and divide the stomach vertically, after the stomach pouch had been calibrated with a 32-French chest tube that had been passed by the anesthesiologist through the patient's mouth. Complete division of the His angle was inspected and was accomplished by firing an additional 45-mm blue-load Endo GIA stapler. The anesthesiologist then removed the chest tube that had been inserted to calibrate the creation of the gastric pouch. Hemostasis was reviewed and obtained. We then brought the Roux loop in an antecolic fashion through the greater omentum window created previously and placed sutures between the posterior aspect of that loop in the seromuscular to the lateral vertical portion of the gastric pouch in a running fashion, to create a posterior seromuscular row for the gastrojejunostomy. The posterior row was approximately 4 cm in length. We then inserted a Harmonic Scalpel to create two small openings, one in the gastric pouch and one in antimesenteric portion of the Roux loop. We inserted an Endo GIA 45-mm blue load into the jejunum and into the stomach to create a gastrojejunostomy, by firing it inside the stomach and the jejunum for approximately 20 mm. The stapler was removed. The opening entrance of the stapler to create the gastrojejunostomy was closed by using a continuous suture of 2-0 Tycron. Five additional seromuscular sutures were placed in the crotch of the gastrojejunostomy and on top of the staple line and on top of the running suture that was used to close the stapler insertion site. Hemostasis was reviewed and obtained. The anesthesiologist then inserted an orogastric tube that was positioned at the level of the gastrojejunostomy. We clamped the jejunum just distal to the gastrojejunostomy and inflated the gastric pouch and the gastrojejunostomy with 60 cc of methylene blue in increments of 10 cc. No leaks or extravasation was noted after careful inspection of all aspects of the anastomosis and gastric pouch. The anesthesiologist then suctioned out the methylene blue solution and removed the orogastric tube. We then placed 5 cc of fibrin glue in the posterior and anterior aspect of the gastrojejunal anastomosis and gastric pouch staple line. We then inserted a 19 Blake drain in the superior portion of the abdomen, exteriorizing it through the left upper quadrant. All the trocars were then removed under direct vision. The pneumoperitoneum was deflated. The skin was closed using staples. A dressing was applied. The drain was sutured to the abdominal wall with a 2-0 nylon suture. At the end of the procedure the sponge, instrument and needle count was correct. The patient was then extubated, awakened from anesthesia, and transported to the recovery room in stable condition.