Diabetes Mellitus and Increased Postoperative Risk of Acute Renal
advertisement
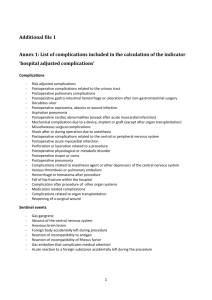
Diabetes Mellitus and Increased Postoperative Risk of Acute Renal Failure After Hepatectomy for Hepatocellular Carcinoma: A Nationwide Population-Based Study Ming-Shian Tsai, MD1, Cheng-Li Lin, MSc2,3, Shih-Ni Chang, MSc4, Po-Huang Lee, MD1, and Chia-Hung Kao, MD5,6 Diabetes mellitus (DM) is a common chronic disease that causes widespread disability and death and can be associated with hepatocellular carcinoma (HCC), coexisting chronic liver disease, and cirrhosis.1–4 Previous studies have demonstrated that DM can negatively affect the long-term prognosis of patients with HCC.1,5–7 However, other studies had not observed any differences in the long-term survival of HCC patients with and without DM.8 DM is proposed to be an independent determinant of increased risk of perioperative complications and mortality in cardiovascular and noncardiac surgeries.9–11 However, the effects of DM on the risk of perioperative morbidity and mortality after hepatectomy remain controversial. In colorectal liver metastasis, DM is associated with an increased risk of mortality after liver resection.12 DM also reportedly increases the risk of postoperative complications after resection for HCC.13 However, in Poon et al.,14 postoperative mortality and morbidity were similar in patients with and without DM. Several of the previous studies investigating surgical risk in DM patients were limited by a relatively small sample size and single-institution experience.12–14 According to our research, no study has evaluated the risk of perioperative mortality and complications after hepatectomy for HCC in DM patients by using a populationbased cohort study. Therefore, we conducted a retrospective case-matched study to determine the effects of DM on the risk of surgical mortality and morbidity in patients undergoing hepatectomy for HCC by using data from the Taiwan National Health Insurance Research Database (NHIRD). We also investigated the effects of coexisting medical conditions and diabetes-related comorbidities on postoperative 30-day mortality in patients with DM. METHODS Data Sources In March 1995, the Taiwanese government implemented the National Health Insurance program, which provides universal health insurance coverage to 99 % of the population in Taiwan. The data analyzed in this study were retrieved from the Taiwan NHIRD, which is managed by the National Health Research Institute (NHRI) in Taiwan. 15 The NHRI compiled all inpatient and outpatient medical benefit claims in the National Health Insurance program and permitted access to the database for research purposes from 1996 to 2010. The NHRI encrypts the personal information of patients for privacy protection and provides researchers with anonymous identification numbers associated with the relevant claims information, which includes patient sex, date of birth, registry of medical services, medication prescriptions, and diagnostic codes in the format of the International Classification of Disease, Revision 9, Clinical Modification (ICD-9-CM). In this study, inpatient claims and diabetes claims (diabetes registry for all patients) data on the entire population in Taiwan were analyzed. Patient consent is not required for accessing the NHIRD or the Longitudinal Health Insurance Database. This study was approved by the Institutional Review Board of China Medical University in Central Taiwan (CMU-REC-101–012). The details of the claims files have been described previously.15 Study Patients By using the inpatient claim dataset, all hospitalized patients who were admitted with a diagnosis of primary carcinoma of the liver (ICD-9-CM 155.0) and who received hepatectomy (ICD-9-OP 50.22 for partial hepatectomy and 50.3 for lobectomy) between January 1, 2000, and December 31, 2010, were identified, and we also excluded patients receiving ablation (ICD-9-OP 50.23–50.26). The diagnostic accuracy of primary carcinoma of the liver was confirmed by the specific admission ICD-9 codes and inclusion in the Registry for Catastrophic Illness Patient Database. The Catastrophic Illness Patient Database is a subsection of the NHIRD, and surgical pathologic and histologic confirmation of liver carcinoma is required for patient registration in the Registry for Catastrophic Illness Patient Database. Patients with at least one hospital admission or at least 3 outpatient visits for DM (ICD-9-CM 250) were defined as the DM case group. One patient without DM was matched to every DM patient by calculating their propensity scores. A propensity score was calculated by using logistics regression to estimate the probabilities of assigning a patient to the DM group by considering several background variables, including age, sex, income, occupation, and other comorbidities, such as hypertension (ICD-9-CM 401–405), mental disorder (ICD9-CM 290–319), ischemic heart disease (ICD-9-CM 410–414), chronic obstructive pulmonary disease (ICD-9CM 490–496), stroke (ICD-9-CM 430–438), hyperlipidemia (ICD-9-CM 272), liver cirrhosis (ICD-9-CM 571.2, 571.5, and 571.6), alcoholic liver disease (ICD-9-CM 571.0, 571.1, and 571.3), chronic kidney disease (ICD-9CM 585), hepatitis B virus (ICD-9-CM V02.61, 070.2, 070.22, 070.3, 070.32), and hepatitis C virus (ICD-9-CM V02.62, 070.41, 070.44, 070.51, 070.54). Outcome Measurements and Comorbidities Postoperative complications were defined as a diagnosis of complications and mortality within 30 days of the index admission date. The complications included septicemia (ICD-9-CM 038 and 998.5), pneumonia (ICD-9-CM 480–486), stroke (ICD-9-CM 430–438), acute renal failure (ARF) (ICD-9-CM 584), acute myocardial infarction (ICD9-CM 410), and wound infection (ICD-9-CM 998.51 and 998.59). For other comorbid conditions, a search was performed to determine the presence of DM-related diseases, such as ketoacidosis (ICD-9-CM 250.1), coma (ICD-9-CM 205.2 and 250.3), renal manifestations (ICD-9-CM 250.4), eye involvement (ICD-9-CM 250.5), and peripheral circulatory disorder (ICD-9-CM 250.7). Statistical Analysis Baseline characteristics were compared between the DM group and the non-DM control group by using the v2 test. Multivariate logistics regression was used to evaluate the effects of DM on the risk of 30-day complications and 30-day mortality, as indicated by the odds ratios (ORs) and 95 % confidence intervals (CIs). To determine the independent risk factors for 30-day postoperative mortality, multivariable analyses and stratified analyses were performed by using a logistics regression model. A 2-tailed p value\0.05 was considered statistically significant. All statistical analyses were performed with SAS statistical software (version 9.2 for Windows; SAS Institute, Inc., Cary, NC). RESULTS Using data from the NHIRD, we identified 2962 DM patients and 2,962 non-DM patients who underwent hepatectomy for HCC during the study period. Table 1 lists the baseline characteristics of these patients. At the time of admission for hepatectomy, approximately 42 % of the patients were aged [65 years, and 72 % of the patients were men. Among the 2,962 DM patients, several patients had previously been hospitalized for hypertension (18.6 %), mental disorder (1.69 %), ischemic heart disease (1.65 %), chronic obstructive pulmonary disease (1.32 %), stroke (1.15 %), hyperlipidemia (1.38 %), liver cirrhosis (33.4 %), alcoholic liver disease (33.0 %), chronic kidney disease (1.42 %), hepatitis B virus (31.0 %), or hepatitis C virus (25.4 %; Table 1). We observed no significant differences in the distributions of age, sex, socioeconomic status, and coexisting medical diseases between the 2 cohorts. However, slightly fewer DM patients underwent major hepatectomy (lobectomy) compared with the nonDM cohort (18.1 vs. 20.4 %; p = 0.02). Table 2 displays the ORs of the postoperative complications associated with DM. The DM patients were significantly associated with an increased risk of septicemia (OR 1.45, 95 % CI 1.06–2.00) in comparison with the non-DM patients. The DM patients were associated with a significantly higher risk of ARF than the non-DM patients (OR 1.70, 95 % CI 1.01–2.84), but not other postoperative complications, including pneumonia (OR 1.02, 95 % CI 0.68–1.53), stroke (OR 0.83, 95 % CI 0.25–2.73), acute myocardial infarction (OR 2.00, 95 % CI 0.37–10.9), and wound infection (OR 1.21, 95 % CI 0.79–1.84). Interestingly, we also observed that hepatectomy extent was related to the risks of septicemia and ARF (Table 3). Compared with non-DM patients undergoing partial hepatectomy, the risk of septicemia was significantly higher in patients receiving lobectomy. Similarly, DM patients undergoing lobectomy exhibited a higher risk of postoperative ARF than non-DM patients undergoing partial hepatectomy (OR 8.53, 95 % CI 1.63–44.5). Subsequently, we investigated the effects of DM-related variables on the risk of postoperative mortality. We observed that the DM group was not significantly associated with an increased risk of 30-day postoperative mortality in all stratified analyses, including risks for DMrelated eye involvement (OR 3.00, 95 % CI 0.61–14.9), DM-related peripheral circulatory disorder (OR 1.67, 95 % CI 0.40–6.97), and DM-related renal manifestations (OR 1.83, 95 % CI 0.68–4.96; Table 4). Finally, we aimed to analyzed whether the risk of postoperative mortality is related to other comorbidities in DM patients. In comparison with the non-DM patients, the DM patients with comorbidities were not significantly associated with 30-day postoperative mortality, including hypertension (OR 0.60, 95 % CI 0.14–2.51), liver cirrhosis (OR 1.00, 95 % CI 0.38–2.66), alcoholic liver disease (OR 1.13, 95 % CI 0.43–2.92), chronic kidney disease (OR 2.00, 95 % CI 0.18–22.1), hepatitis B virus (OR 0.64, 95 % CI 0.25–1.64), and hepatitis C virus (OR 0.82, 95 % CI 0.34–1.97; Table 5). DISCUSSION According to our research, this study is the first nationwide population-based study to investigate the effects of DM on the risk of surgical mortality and morbidity in patients undergoing resection for HCC. We observed that the DM patients were associated with an increased risk of postoperative septicemia and ARF in comparison with non-DM patients. However, they did not exhibit an increased risk of postoperative mortality or other major complications, including pneumonia, stroke, and myocardial infarction. Patients with preoperative DMrelated complications were nonsignificantly associated with an increased risk of postoperative mortality after hepatectomy. The study results indicate that DM should not be considered as a contraindication for surgical treatment for HCC. However, special attention should be devoted to the perioperative monitoring and preservation of renal function in DM patients undergoing hepatectomy. Septicemia is not an uncommon complication after hepatectomy. The severe postoperative infection can be due to pneumonia, bloodstream infection related to a central line, urinary tract infection, infected intraabdominal fluid accumulation, and biliary tract infection.16 DM patients are susceptible to infection, and previous studies have proposed DM is a prognostic factor of postoperative infection events, which was in line with our data.16–18 Better glycemic control may be helpful to reduce the risk of postoperative septicemia.19 Few studies have reported the incidence and risk factors of ARF after hepatectomy, despite ARF being a substantial clinical problem in patients with liver failure and after liver transplantation.20,21 Depending on the definition of ARF, the incidence of ARF varies across studies, in the range of 1–30 % after cardiac bypass surgery.22 Previous studies have reported the incidence of acute kidney injury as ranging from 5.8 to 6.7 % after noncardiac surgery.23,24 In this study, the incidence of ARF after hepatectomy was 0.78 % in the control cohort and 1.32 % in the DM cohort. Several factors can contribute to the development of postoperative ARF, including hemodynamic instability, surgery-related inflammation, use of vasoactive or nephrotoxic agents, and ischemic reperfusion injury to the liver.25,26 DM has been proposed as a risk factor for ARF development, and the possible underlying pathophysiologic mechanisms include renal hemodynamic instability, endothelial cell injury, and inflammatory processes.27–29 Approximately 70–90 % of patients with HCC suffer from chronic liver diseases and cirrhosis, which could result from viral hepatitis, alcoholic liver disease, nonalcoholic steatohepatitis, autoimmune hepatitis, or toxin exposure.4 Most HCC patients are associated with a degree of liver impairment; therefore, postoperative liver failure represents one of the major causes of mortality after hepatectomy. 30 Shirabe et al.31 proposed that major hepatectomy should be avoided for patients with DM and an expected remnant liver volume\250 mL/m2 to prevent postoperative liver failure. Although animal studies have demonstrated that diabetes can impair liver regeneration, the clinical effects of DM on the severity of liver cirrhosis and liver function recovery remain controversial.8,32–34 Studies have also indicated that diabetes is a negative prognostic factor for long-term survival in patients with cirrhosis and that death in these patients is predominantly caused by impaired liver function and not DM-related cardiovascular diseases.35,36 However, Schlichting et al.37 suggested that DM was a nonsignificant risk factor for mortality in a large series of patients with cirrhosis. Therefore, the association between DM and liver function warrants further investigation. Whether DM is a predisposing factor for surgical complications after hepatectomy remains unclear.14,38,39 Previous studies have suggested that DM does not increase the risk of postoperative morbidity, whereas other studies have demonstrated that DM increases the risk of postoperative complications, especially in patients aged [70 years and patients undergoing major hepatectomy (right hepatectomy and expected small remnant liver volume). 14,29,30,37,39 DM patients can experience endothelial dysfunction, impaired wound repair, and infection, all of which could contribute to postoperative complications after hepatectomy.28,40,41 However, the results of this study indicated no differences in the rate of complications between the DM and non-DM cohorts. In addition, the surgical morbidity rates of the patients with DM-related complications exhibited no significant differences compared with those of the non-DM patients. Our observations could be partially explained by improvements in perioperative care and hepatectomy techniques. However, this hypothesis should be validated in future well-designed studies. This study has several limitations that must be addressed. First, the insurance dataset does not provide detailed information on patient smoking habits, alcohol consumption, liver function, blood loss, and method of liver resection, which are all potential confounding factors relevant to this study. Second, unlike prospective studies, a retrospective cohort study design is subject to biases related to the adjustment for confounders. Despite the use of adequate controls, potential bias remained in the analyses because of unmeasured or unknown confounders. Additional studies using animal models could be feasible for further evaluating the effects of DM on liver function recovery after hepatectomy in normal and cirrhotic livers. Third, we could not validate the diagnoses of DM, HCC, and complications by reviewing charts. ARF is usually coded when the patient shows oliguria and the retention of urea and other nitrogenous waste products, especially in the setting requiring renal replacement therapy. Therefore, the diagnoses should be accurate because the data were derived from an inpatient database in which diagnoses were strictly audited for the purpose of reimbursement. Fourth, the study patients were identified based on initial inpatient admission in the NHRID, which could have led to potential selection bias toward a population with severe diseases or increased access to hospital care. For example, patients with mild DM and patients lacking access to hospital care might have been excluded from the analyses. However, although these scenarios could have caused the underestimation or overestimation of the association between DM and the risk of postoperative complications, they should not have seriously biased the study results based on the universal health insurance data used. In summary, we determined that DM is associated with an increased postoperative risk of septicemia and ARF after hepatectomy for HCC. However, the results also indicated that DM is not associated with increased postoperative mortality in patients undergoing hepatectomy for HCC. The mechanisms underlying these observations warrant further investigation.