Lions Eye Bank of Lexington
advertisement
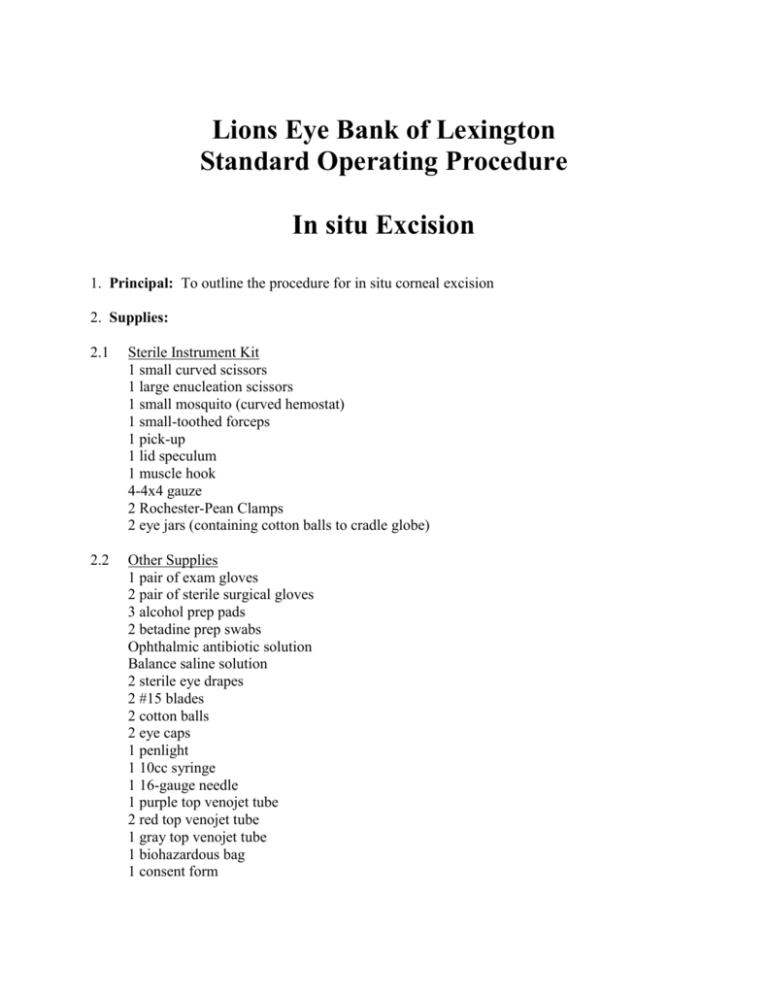
Lions Eye Bank of Lexington Standard Operating Procedure In situ Excision 1. Principal: To outline the procedure for in situ corneal excision 2. Supplies: 2.1 Sterile Instrument Kit 1 small curved scissors 1 large enucleation scissors 1 small mosquito (curved hemostat) 1 small-toothed forceps 1 pick-up 1 lid speculum 1 muscle hook 4-4x4 gauze 2 Rochester-Pean Clamps 2 eye jars (containing cotton balls to cradle globe) 2.2 Other Supplies 1 pair of exam gloves 2 pair of sterile surgical gloves 3 alcohol prep pads 2 betadine prep swabs Ophthalmic antibiotic solution Balance saline solution 2 sterile eye drapes 2 #15 blades 2 cotton balls 2 eye caps 1 penlight 1 10cc syringe 1 16-gauge needle 1 purple top venojet tube 2 red top venojet tube 1 gray top venojet tube 1 biohazardous bag 1 consent form 1 donor history form 1 tongue depressor 1 protective gown 2 pair of sterile sleeves 2 sterile OR towels 2 sterile corneal chambers 1 scrub brush 1 head cover 1 mask with face shield 1 clear plastic bag 2 cotton-tip applicators 1 Medical Examiner From 1 Enucleation Post-Op Form 1 Corneal Excision Post-Op Form 1 Yellow Toe Tag 3. Preparatory Steps 3.1 Verify consent 3.1.1 Verify the existence of a signed and properly completed consent form or documented telephonic consent. In the absence of an appropriate consent DO NOT PROCEED 3.2 Medical Chart 3.2.1 Review and copy the donor’s medical chart 3.3 Donor Identification 3.3.1 Identification should be verified by toe tag, wristband, or other hospital applied identification. In the absence of suitable identification DO NOT PROCEED until appropriate hospital personnel can make the identification. Document the name of the hospital staff member making the identification. 3.4 Protective Clothing 3.4.1 Don gown, cap and mask with face shield and exam glove. 3.5 Physical Assessment 3.5.1 The procurement technician will complete a thorough physical exam and document all findings on the Physical assessment Worksheet including all injuries, invasive tubes/lines, scars, etc. Physical evidence for risk of sexually transmitted diseases such as genital ulcerative diseases, herpes simplex, syphilis, chancroid; 3.5.2 3.5.3 3.5.4 3.5.5 Physical evidence of anal intercourse including perianal condyloma; Physical evidence of non-medical percutaneous drug use such as needle tracks; Disseminated lymphadenopathy; Oral thrush; Blue or purple spots consistent with Kaposi’s sarcoma; Needle tracks, including examination of tattoos which may be covering needle tracks; Unexplained jaundice, hepatomegaly or icterus; or If the body was rejected for routine autopsy due to infectious criteria or if the autopsy was done in an infectious disease control room or under any special precautions and the reasons for these procedures. If any of the above signs are observed on the physical assessment and are deemed to be an indication of either high-risk behavior or an indication of HIV or hepatitis infection then the tissue should be rejected. The procurement technician will perform a pen light exam on the donor and document any findings on the Physical Assessment Form The donor’s weight shall be documented on IV Infusion/Transfusion Worksheet Document the date and time the donor was refrigerated if applicable on the Donor History Form 3.6 Blood Sample 3.6.1 Verify the donor’s transfusion history and document whether a pretransfusion sample is required. 3.6.1.1 21 CFR Part 1270 states that tissue shall be determined to be unsuitable for transplantation if transfusion or infusion has been sufficient to affect test results. Transfusion or infusion in the absence of blood loss should not normally be sufficient to affect test results. However, when: blood loss is known or suspected to have occurred, the potential tissue donor was transfused or infused and no adequate per-transfusion/infusion sample is available for infectious disease testing; then an algorithm should be used to determine that there has not been plasma dilution sufficient to affect test results. For adults if administration of: more than 2000 milliliters of whole blood, reconstituted blood, red blood cells (RBC) and/or colloid occurs within 48 hours immediately preceding the collection of a blood sample for testing; or administration of more that 2000 milliliters of crystalloid within the one hour preceding the taking of a blood sample for testing; or a combination of more that 2000 milliliters of the above occurs, and there is no pre-transfused/infused blood sample, then the algorithm defined in the SOP should be applied. NOTE: If a donor is 12 years of age or under and there is no pre-transfusion sample, then an algorithm should be applied when any transfusion or infusion has occurred to determine that there has not been plasma dilution sufficient to affect test results. 3.6.2 Draw a sample of blood from the subclavian, femoral, or jugular areas. 3.6.2.1 Locate the appropriate anatomical landmarks. Insert the 16-gauge needle full length to the hub of the syringe and pull back the plunger. Blood will enter the syringe when the vessel is entered. If blood does not enter the syringe pull the needle slightly back at a different angle until you see blood return in the syringe. Draw 10cc of blood. 3.6.2.2 Carefully insert the needle into the red top tube, taking extreme care to avoid a needle stick. When the red top tube is full, pull the needle from the tube and with the same precautions insert the needle into the purple top tube with the remaining blood. 3.6.2.3 Using Universal Precautions, discard the needle and syringe in a sharps container. 3.6.2.4 If the donor is bleeding from the puncture site apply pressure over the site and gently rub the skin to close the puncture and sop the bleeding. 3.6.2.5 Label the blood tube with the appropriate Id number/donor name. 3.6.2.6 Package the blood in a biohazardous bag provided in the kit. 4. Prepare the Donor 4.1 Elevate the donor’s head 4.2 Irrigate both eyes with copious amounts of balanced saline solution 4.3 Apply about 5 drops of ophthalmic antibiotic solution to each eye and close lids. 4.4 Clean the orbital area with alcohol making sure to go over the bridge of the nose and above the eyebrows. Allow the alcohol to dry. 4.5 Using the betadine prep swabs, apply the betadine beginning at the upper medial canthus and working outward, around and below the lid, over the bridge of the nose and above the eyebrows. 4.6 Remove prep gloves and dispose of them in a biohazardous waste bag. 5. Prepare Sterile Field 1.1 Sterile Field 1.1.1 Prepare the sterile field by first placing the sterile instrument tray on your prepared work surface. 1.1.2 Remove the plastic dust cover. 1.1.3 Before opening he sterile kit, verify that the instrument kit is sterile by checking the expiration date and integrity of the wrap. 1.1.4 Carefully open the outer and inner wraps. 1.1.5 Open additional sterile supplies onto the sterile field such as blades, eye drapes, cotton-tip applicators, and corneal chambers. 1.2 Sterile Sleeves & Gloves 1.2.1 Open outside packages of sterile sleeves, gloves, and towels. 1.2.2 Scrub utilizing the Brush-Stroke Method. 1.2.2.1 Wet hands and arms. 1.2.2.2 Wash hands and arms to 2 inches above the elbows with an antiseptic agent. 1.2.2.3 With hands held under running water, clean under fingernails with disposable nail cleaner; discard after use. 1.2.2.4 Rinse hands thoroughly under running water, keeping hands up and allowing water to drip from elbows. 1.2.2.5 Take sterile brush/sponge impregnated with antiseptic from package. 1.2.2.6 Scrub nail of on hand 30 strokes; each side of each finger, starting with the thumb, 20 strokes; the back of the hand 20 strokes; the palm of the hand 20 strokes; the arm 20 strokes for each 3rd and each side to 2 inches above the elbow. 1.2.2.7 Repeat steps for the other hand and arm. 1.2.2.8 Rinse hands and arms thoroughly. 1.2.3 Drying 1.2.3.1 Reach down and lift towel from package, being careful not to drip water on the package. Bend forward slightly to avoid letting the towel touch your attire. 1.2.3.2 Dry both hands independently. Dry one arm holding towel in opposite hand and using an oscillation motion of the arm. 1.2.3.3 Draw the towel up to the elbow 1.2.3.4 Carefully reverse the towel, holding it away from the body. 1.2.3.5 Dry the opposite arm on the unused, now uppermost end of the towel. 1.2.4 Donning Sterile Gloves and Sterile Sleeves 1.2.4.1 Gloving using Open Glove Technique without a gown. This method of gloving skin-to-skin, glove-to-glove technique. . The hand, although scrubbed, is not sterile and must not contact the exterior of the sterile gloves. The everted cuff on the gloves exposes the inner surface. The first glove is put on with skin-to-skin technique, bare hand to inside cuff. The sterile fingers of that gloved hand then may touch the sterile exterior of the second glove, that is, glove-to-glove technique. 1.2.4.2 With the left hand, grasp the cuff of the right glove on the fold. Pick up the glove and step back from the table. 1.2.4.3 Insert the right hand into the glove and pull it on, leaving the cuff turned well down over the hand. 1.2.4.4 Slip the fingers of the gloved right hand under the everted cuff of the left glove. Pick up the glove and step back. 1.2.4.5 Insert the hand into the left glove and pull it on, leaving the cuff turned down over the hand. 1.2.4.6 With the fingers of the right hand, pull the cuff of the left glove up and avoid touching the bare wrist. 1.2.4.7 Repeat step 5 for the right cuff, using the left hand, and thereby completely gloving the right hand. 1.2.5 Donning sterile sleeves. 1.2.5.1 Reach down to the sterile package and slide gloved hand under folded upper portion of sleeve. Step back from the table and let the sleeve unfold. 1.2.5.2 Being careful to keep gloved hand protected by the fold in the sleeve, slide opposite hand into sleeve and pull through the cuff. 1.2.5.3 Pull the sleeve to wrist level only. 1.2.5.4 Do not push glove all the way through the sleeve. 1.2.5.5 Pull upper portion of sleeve to 2 inches above elbow. Again, being careful to protect sterile, gloved hand with folded upper cuff. 1.2.5.6 Once you have pulled sleeve to above elbow, do not return to that area with the gloved hand again. 1.2.5.7 Repeat, using opposite hand and sleeve. 1.2.6 Don the second pair of sterile gloves using open glove technique as described above. 6. Excision 1.1 Check the instruments to be sure none are missing 1.2 Apply sterile drapes to donor lids 1.3 Using a cotton-tipped applicator, gently open the upper lid by pulling towards the top of the head, insert the closed lid speculum under the upper and lower lids. Take care not to abrade the cornea with the speculum 1.4 Grasp the conjunctiva with the forceps near the limbus. Cut and dissect the conjunctiva using the small curved scissors 360’ around the cornea. Remove any remaining conjunctiva by carefully scraping down from the limbus with a scalpel blade (#15) 1.5 Isolate the instruments and scalpel used to scrape the conjunctiva from the other instruments on the sterile field. Use these only for the same purpose on the opposite eye. 1.6 Make an incision through the sclera 2-4 mm from the limbus using a second scalpel blade (#15). If you need to steady the eye this can be accomplished by using a muscle hook or hemostat to grasp a muscle. Be careful not to perforate the choroid. 1.7 Insert the blades of the Castroveijo or Wescott scissors through the scleral incision into the suprachoroidal space. Perform a periotomy to complete the scleral incision 360’ around the cornea. Keep the incision parallel to the limbus to produce an even scleral rim. 1.8 After the incision is complete, the cornea may be removed by using one pair of small toothed forceps to grasp the scleral rim and the back of a scalpel blade or forceps to push the ciliary body down and away from the corneoscleral button. 1.9 Separate the remaining adhesions by working from side to side taking care not to pull on the cornea. The corneoscleral button should never be allowed to drop back down wile making the separation. 1.10After separating the corneoscleral button from the eye, hold the corneoscleral button with the small forceps and transfer to a corneal chamber containing Optisol-GS. 1.11Examine the posterior chamber for crystalline lens. 1.12Remove top pair of gloves and repeat steps 6.1 through 6.9 on the other eye. 7. Concluding steps 7.1. Remove drapes 7.2. Leave head elevated 7.3. Place an eye cap over the posterior chamber and pull the upper and lower lids shut. 7.4. Place the lids on both corneal chamber and label each chamber. Ocular tissue is put in a Ziploc bag and placed on wet ice for transport. Upon return to the eye bank ocular tissue shall be placed in the section marked Quarantined of the Jewett Refrigerator. 7.5. Clean off any remaining debris (i.e., betadine, blood) using balanced saline solution and gauze. 7.6. Complete a toe tag and affix to the body and rewrap the donor body in the body bag or shroud and return it to the storage area from which it was removed. 7.7. Follow steps described in Exposure Control (Section 10) below. 7.8. Call the hospital contact person and the funeral home to inform them that the procedure is completed and the body may be picked up. 8. Documentation 8.1 Document the date and time of enucleation and the media used on the Donor History Form. 8.2 Complete an Eye Enucleation Post Operative Form if the enucleation was performed in the hospital. Leave one copy with the hospital and return the other to the eye bank to be retained in the donor file. 9. Autopsy 1.1 If an autopsy is to be performed by the Medical Examiner the technician will draw a vitreous sample after the enucleation procedure and prior to the excision. Place the vitreous sample in the gray top tube provided in the kit. The tube shall be labeled with the donor’s name, date & time the sample was drawn. The tube should then be taped to the donor’s chest. 1.2 The technician will then fill out the Eye Evaluation Form for Coroner/Medical Examiners and leave it with the body. 1.3 Document on the Donor History From the date & time and where the autopsy will be performed. 10. Exposure Control 10.1 Discard all sharps in the appropriate Biohazardous sharps container. 10.2Dispose of all personal protective clothing and equipment in appropriate Biohazardous waste containers 10.3Wash hands thoroughly before leaving the work area. 11. References 11.1EBAA Medical Standards; November 1998 11.2EBAA Procedures Manual; October 1996, (E1.000 & E1.200) 12. Effective Date March 1, 1999 13. Approvals 13.1______________________________________________________________ Director of Technical Services Date 13.2______________________________________________________________ Executive Director Date 13.3______________________________________________________________ Medical Director Date