Orbital Diseases, Differential Diagnosis, and Management
advertisement
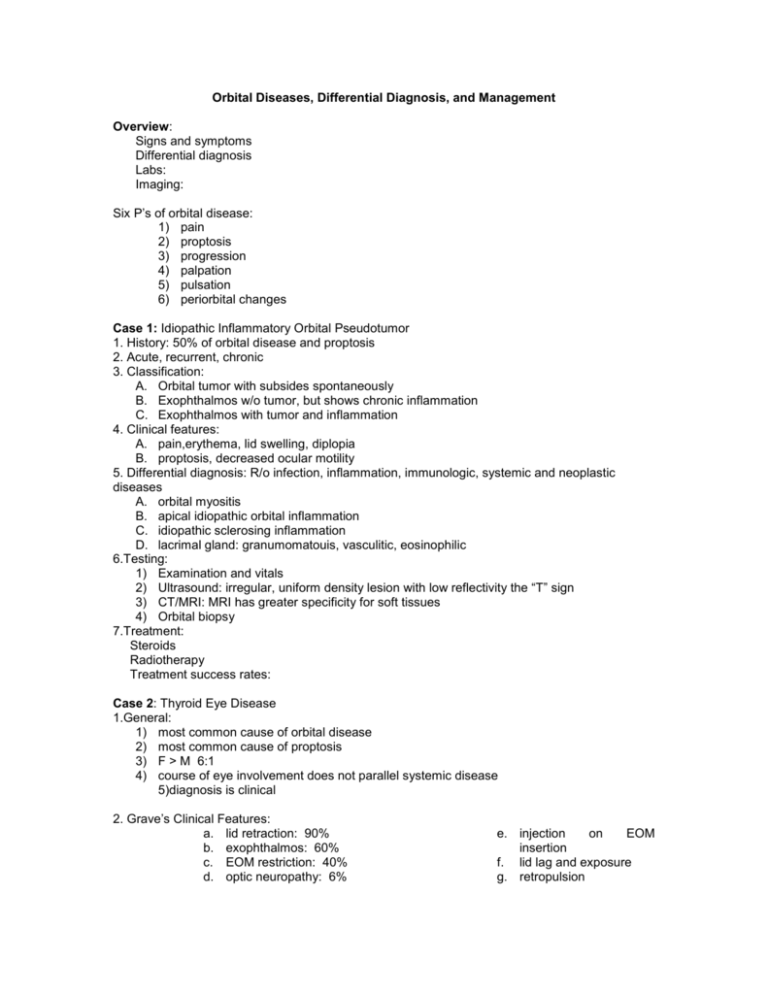
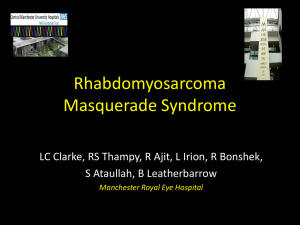
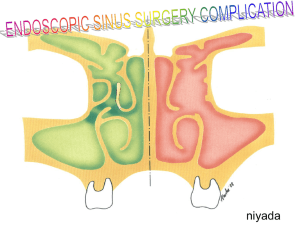
Orbital Diseases, Differential Diagnosis, and Management Overview: Signs and symptoms Differential diagnosis Labs: Imaging: Six P’s of orbital disease: 1) pain 2) proptosis 3) progression 4) palpation 5) pulsation 6) periorbital changes Case 1: Idiopathic Inflammatory Orbital Pseudotumor 1. History: 50% of orbital disease and proptosis 2. Acute, recurrent, chronic 3. Classification: A. Orbital tumor with subsides spontaneously B. Exophthalmos w/o tumor, but shows chronic inflammation C. Exophthalmos with tumor and inflammation 4. Clinical features: A. pain,erythema, lid swelling, diplopia B. proptosis, decreased ocular motility 5. Differential diagnosis: R/o infection, inflammation, immunologic, systemic and neoplastic diseases A. orbital myositis B. apical idiopathic orbital inflammation C. idiopathic sclerosing inflammation D. lacrimal gland: granumomatouis, vasculitic, eosinophilic 6.Testing: 1) Examination and vitals 2) Ultrasound: irregular, uniform density lesion with low reflectivity the “T” sign 3) CT/MRI: MRI has greater specificity for soft tissues 4) Orbital biopsy 7.Treatment: Steroids Radiotherapy Treatment success rates: Case 2: Thyroid Eye Disease 1.General: 1) most common cause of orbital disease 2) most common cause of proptosis 3) F > M 6:1 4) course of eye involvement does not parallel systemic disease 5)diagnosis is clinical 2. Grave’s Clinical Features: a. lid retraction: 90% b. exophthalmos: 60% c. EOM restriction: 40% d. optic neuropathy: 6% e. injection on EOM insertion f. lid lag and exposure g. retropulsion h. asymmetric, slowly progressive disease i. painless, prominent eyes j. k. l. pain and discomfort: 30% diplopia: 17% blurryvision:7.5% 3. Mechanism: » unknown immune response » circulating T-cells and antigen on thyroid follicular cells 4. Systemic Disease: » Hyperthyroidism: 90%, 75% develop eye findings » Primary Hypothyroidism: 1% » Hashimoto’s Thyroiditis: 3% » Euthyroid: 6% » Myasthenia Gravis: 1% 5. Classification: NO SPECS: N (0) = no signs or symptoms O (1) = only signs, no symptoms S (2) = soft tissue involvement only P (3) = proptosis E (4) = EOM restriction C (5) = corneal involvement S (6) = sight loss 6.Testing a) Ancillary testing: b) Labs: T3, T4, TSH , others; TSH, TRH or TSH-IRMA, CBC with differential, chemistry panel anticholinergic Ab and tensilon test 7. Imaging:CT/MRI: 8.Treatment a) Referral to internist and/or endocrinologist b) return patient to euthyroid state c) Topical/supportive therapy d) Optical and medical therapies e) Elevate patient’s head for sleep f) Active congestion treated more aggressively g) General: Steroids, orbital radiation, orbital decompression, strabismus surgery, lid surgery Case 3: Orbital Cellulitis with a subperiosteal abscess 1) Clinical Features: 2) Etiology/Histology: a) extension from sinus infection: 90% b) ethmoidal sinus: 90% c) orbital trauma/surgery d) vascular infection or infection via other tissue e) Organisms: staph, strep, H-flu, and gram - rods Testing: a) Exam/Vitals: b) Labs: CBC with differential, chemistry panel, culture: blood, wounds, debrided, material c) LP with CSF analysis d) CT/MRI:inflammatory/infectious material and cells in sinus/orbit Classification:: Chandler Inflammatory Edema: Orbital Cellulitis: Subperiosteal Abscess: Orbital Abscess: Cavernous Sinus Thrombosis: Treatment: a) Admission to hospital: referral to ENT, Internal Medicine, and Ophthalmology b) Nasal decongestant spray prn, Ab ointment topically: culture specific c) Surgical drainage of abscesses d) I.V. Abx x 1 week, response w/in 48 hrs Case 4) Lacrimal Gland Inflammation/Infiltration: 1)Features: Persistent, progressive swelling of outer 1/3 of upper eyelid (S-Shaped) Pain, Tenderness, Temporal lid injection, Conjunctival fornix injection, Displacement of globe 2)Etiology: Inflammatory disease, Structural disease, Neoplastic disease 3)Tests:Labs, CT/ MRI: Lacrimal gland biopsy: Suspected tumor Uncertain inflammatory/infectious process 5) differential diagnosis: 6) Treatment: referral to internist/hematologist/ oncologist, steroids, antibiotics, surgical removal Case 5) Paraocular Sinus Mucoceles 1) Clinical Features: Slow space-occupying lesions; May be sterile or harbor infection Increase in size, May be worsened by active sinusitis, Proptosis, Restricted EOM’s Orbital displacement 2) Etiology / Histology: Form as a result of blockage of sinus cell ostium 3)Testing: CT/MRI 4) Treatment: Consultation with ENT, Surgical excision and removal of sinus mucosa Establish normal drainage, Obliteration of sinus Case 6) Orbital Metastasis 1)features: May arise from various sources, Seeds to sinuses via blood stream, or lymphatic dissemination Similar signs and symptoms to other orbital diseases, Pain and proptosis may be a prominent early sign, Diplopia earlier, Less proptosis due to earlier presentation 2)Differential diagnosis: 3)testing: CT/MRI/Ultrasound: Ultrasounic differences 4)Treatment: Radiation therapy, Chemotherapy, Surgery, Hormonal therapy