COLLES FRACTURE
advertisement
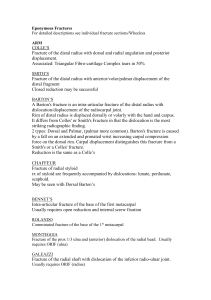
COLLES FRACTURE This is a very common injury which affects the distal end of the radius. It was first described by Abraham Colles in 1814 who reported a transverse fracture of the radius, within 1 inch of the wrist, and with dorsal displacement and dorsal angulation of the distal fragment. The fracture is most common in elderly postmenopausal osteoporotic women who give a history of a fall onto an outstretched hand. Clinical features: Classically, the fracture presents with a 'dinner fork' deformity of the wrist. There are five components to the deformity: dorsal angulation of the distal fragment dorsal displacement of the distal fragment radial deviation of the hand supination proximal impaction Radiology reveals a transverse fracture of the distal radius about 2.5 cm from the wrist. The fragment is tilted and shifted backwards and radially, with proximal impaction. Occasionally, the distal fragment is severely comminuted or crushed. Frequently, there is an associated fracture of the ulnar styloid. In severe cases, there may be dislocation of the distal radio-ulnar joint or fracture of the styloid process of the ulna. Differential diagnosis: It is important to exclude a Galeazzi fracture in patients with a suspected Colles' fracture as the former requires internal fixation. Colles' fracture does not occur in children. A more likely explanation of a 'dinner fork' deformity in such patients would be be a greenstick fracture of the distal radius or a fracture separation of the radial epiphysis. Treatment: A displaced fracture should be reduced under appropriate anaesthesia such as: Bier's block axillary block general anaesthesia Disimpaction is achieved by pulling the hand distally and hyperextending the wrist. Once the fracture has been reduced, the wrist is manipulated into a position of palmar flexion, ulnar deviation and pronation. a plaster is applied which extends from elbow to the metacarpophalangeal joints, which lie in the line of the proximal skin crease in the palm and not at the base of the fingers. This arrangement permits thumb and finger movements as well as elbow flexion. The patient is given a sling with instructions to actively exercise the fingers, elbow and shoulder. The fracture should be inspected the following day to check that the plaster is not too tight. A further appointment should be made in 7-10 days. Re-displacement is not uncommon and requires re-reduction. The fracture should have united by about 6 weeks. Undisplaced or minimally displaced fractures may be treated directly with a Colles' backslab. Severely comminuted and unstable fractures may require external fixation. Designs such as the Pennig fixator incorporate a jointed body so permitting early movement. Complications: Early Possible early complications include: swelling and pain of the fingers: o from an overly tight plaster o easily corrected by re-plastering median nerve damage: o rare, due to carpal tunnel compression o may require decompression Sudek's atrophy: o usually restricted to the fingers but may involve the shoulders o exercise of the limb helps to prevent it Complications: Late Possible late complications include: mal-union: o is common o the reduction may have been incomplete or displacement overlooked o disability may be minor but unsightly deformity may be more of a problem o surgical correction may be indicated non-union of the ulnar styloid process rupture of extensor pollicis longus: o due to either movement across a sharp edge of bone or if displacement is minimal, probably, ischaemia o usually treated by tendon transfer using one of the extensors of the index finger stiffness: o from inadequate exercise and / or prolonged splintage o may affect the wrist or the shoulder