Peripheral Blood Tests in Iron Deficiency Anemia Diagnosis
advertisement
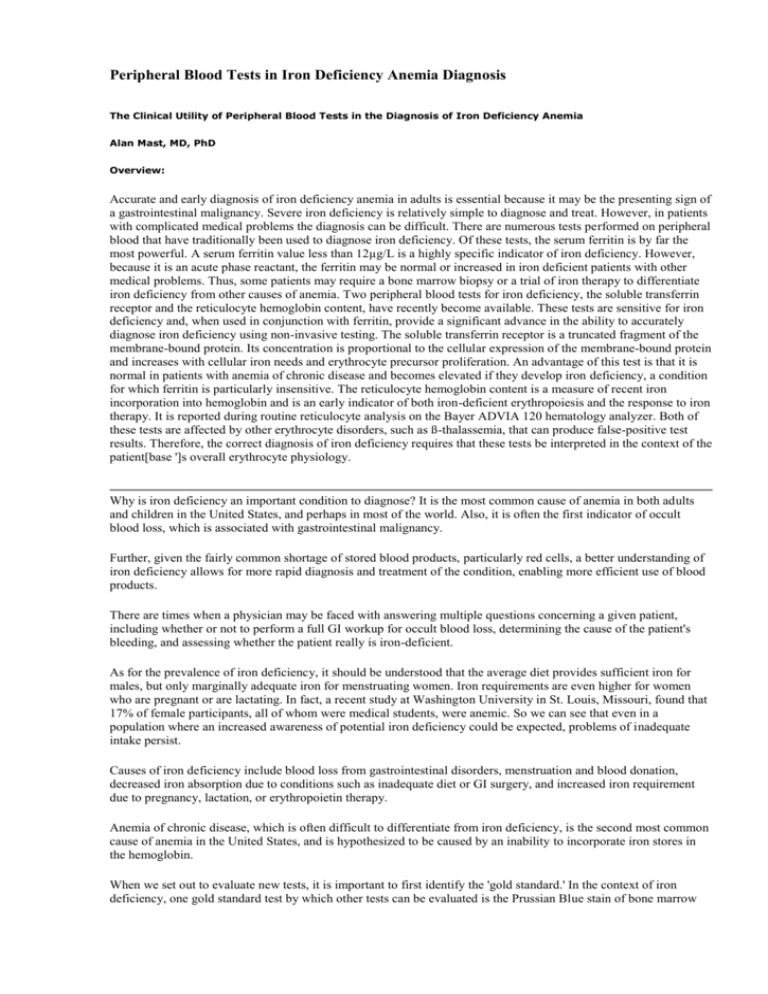
Peripheral Blood Tests in Iron Deficiency Anemia Diagnosis The Clinical Utility of Peripheral Blood Tests in the Diagnosis of Iron Deficiency Anemia Alan Mast, MD, PhD Overview: Accurate and early diagnosis of iron deficiency anemia in adults is essential because it may be the presenting sign of a gastrointestinal malignancy. Severe iron deficiency is relatively simple to diagnose and treat. However, in patients with complicated medical problems the diagnosis can be difficult. There are numerous tests performed on peripheral blood that have traditionally been used to diagnose iron deficiency. Of these tests, the serum ferritin is by far the most powerful. A serum ferritin value less than 12µg/L is a highly specific indicator of iron deficiency. However, because it is an acute phase reactant, the ferritin may be normal or increased in iron deficient patients with other medical problems. Thus, some patients may require a bone marrow biopsy or a trial of iron therapy to differentiate iron deficiency from other causes of anemia. Two peripheral blood tests for iron deficiency, the soluble transferrin receptor and the reticulocyte hemoglobin content, have recently become available. These tests are sensitive for iron deficiency and, when used in conjunction with ferritin, provide a significant advance in the ability to accurately diagnose iron deficiency using non-invasive testing. The soluble transferrin receptor is a truncated fragment of the membrane-bound protein. Its concentration is proportional to the cellular expression of the membrane-bound protein and increases with cellular iron needs and erythrocyte precursor proliferation. An advantage of this test is that it is normal in patients with anemia of chronic disease and becomes elevated if they develop iron deficiency, a condition for which ferritin is particularly insensitive. The reticulocyte hemoglobin content is a measure of recent iron incorporation into hemoglobin and is an early indicator of both iron-deficient erythropoiesis and the response to iron therapy. It is reported during routine reticulocyte analysis on the Bayer ADVIA 120 hematology analyzer. Both of these tests are affected by other erythrocyte disorders, such as ß-thalassemia, that can produce false-positive test results. Therefore, the correct diagnosis of iron deficiency requires that these tests be interpreted in the context of the patient[base ']s overall erythrocyte physiology. Why is iron deficiency an important condition to diagnose? It is the most common cause of anemia in both adults and children in the United States, and perhaps in most of the world. Also, it is often the first indicator of occult blood loss, which is associated with gastrointestinal malignancy. Further, given the fairly common shortage of stored blood products, particularly red cells, a better understanding of iron deficiency allows for more rapid diagnosis and treatment of the condition, enabling more efficient use of blood products. There are times when a physician may be faced with answering multiple questions concerning a given patient, including whether or not to perform a full GI workup for occult blood loss, determining the cause of the patient's bleeding, and assessing whether the patient really is iron-deficient. As for the prevalence of iron deficiency, it should be understood that the average diet provides sufficient iron for males, but only marginally adequate iron for menstruating women. Iron requirements are even higher for women who are pregnant or are lactating. In fact, a recent study at Washington University in St. Louis, Missouri, found that 17% of female participants, all of whom were medical students, were anemic. So we can see that even in a population where an increased awareness of potential iron deficiency could be expected, problems of inadequate intake persist. Causes of iron deficiency include blood loss from gastrointestinal disorders, menstruation and blood donation, decreased iron absorption due to conditions such as inadequate diet or GI surgery, and increased iron requirement due to pregnancy, lactation, or erythropoietin therapy. Anemia of chronic disease, which is often difficult to differentiate from iron deficiency, is the second most common cause of anemia in the United States, and is hypothesized to be caused by an inability to incorporate iron stores in the hemoglobin. When we set out to evaluate new tests, it is important to first identify the 'gold standard.' In the context of iron deficiency, one gold standard test by which other tests can be evaluated is the Prussian Blue stain of bone marrow aspirate. However, while this method will readily detect the level of iron stores in the bone marrow, it is an invasive and painful procedure, and is relatively expensive. A second gold standard is the measurement of response to iron therapy. This can be an adequate gold standard, but its efficiency can be complicated by the fact that it requires a compliant patient who will continue to take the iron therapy despite its side effects. This method also requires a significant amount of time to find out if a patient is irondeficient or not, because it takes one to two weeks for hematocrit levels to rise in response to the therapy. Besides the potential gold standard tests of bone marrow aspirate and response to iron therapy, there have traditionally been a number of blood tests used to assess iron deficiency. These peripheral tests include serum iron, TIBC (transferrin), percent saturation of TIBC, serum ferritin, free erythrocyte protoporphyrin, peripheral smear, hemoglobin, MCV, and RDW. Additionally, there are two newer blood tests for iron deficiency that will be examined in more detail: soluble transferrin receptor and reticulocyte hemoglobin content. Numerous studies have been conducted comparing the more traditional blood tests for iron deficiency to a gold standard of bone marrow aspirate evaluation, and these studies appear to reach the same conclusion. For example Lough, et al.1 studied the peripheral blood tests in 447 patients undergoing bone marrow aspiration. They concluded that, "Serum ferritin should be retained in the laboratory investigation of iron deficiency," and that, "Serum iron and iron binding capacity should be removed from the repertoire." Another study, by Burns, et al. 2 evaluated peripheral blood tests in 301 anemic patients, and concluded that serum ferritin was clearly the only useful test for diagnosing iron deficiency in hospitalized patients. Importantly, they also pointed out the main limitation for ferritin: that it is limited by its low sensitivity. Finally, one other study from Murthy et al.3 studied the peripheral blood tests in 191 patients and concluded that serum ferritin was the most reliable non-invasive test for iron deficiency. Several other studies in the literature have come to the same conclusion - that serum ferritin, at least in most patients, is the single best test for the diagnosis of iron deficiency, and that other traditionally used peripheral tests add little additional diagnostic utility to serum ferritin alone. It is important to note, however, as previously mentioned, that there can be a problem with the sensitivity of serum ferritin. This is due to the fact that serum ferritin is an acute phase reactant, leading to increased levels in ill persons. This means that when studying iron deficiency in a given population using serum ferritin levels, iron status can be accurately determined when levels are above or below given cut-off points, but that there is a substantial portion of the population that does not meet either cutoff, resulting in an indeterminate diagnoses. To examine this limitation of serum ferritin a little more closely, think about a possible study in a given population in which a ferritin of less than 30 µg/L indicates iron deficiency and a ferritin higher than 100 µg/L indicates that a patient is not iron deficient. That leaves measures from 30-100 µg/L as indeterminate. To determine if patients with indeterminate measures are iron-deficient, further testing will be necessary. One option at this point would be to do a bone marrow aspirate. However, given the previously discussed drawbacks to this method of testing, it would be preferable to have alternatives. The two newer peripheral tests of iron status the soluble transferrin receptor and the reticulocyte hemoglobin content - may provide these alternatives, helping to avoid bone marrow biopsy. Looking at soluble transferrin receptor (sTfR), it is important to recall that transferrin is the protein that binds iron, and that iron is transported into a cell through the transferrin receptor. When cells require iron, they express a number of transferrin receptors on the cell surface, and the number of expressed transferrin receptors on a cell is a measure of how iron-starved the cell is. The soluble form of the transferrin receptor results from what can be thought of as a sort of random proteolysis. At a certain rate of transferrin receptor expression, receptors are cleaved off the cell surface and become soluble. The level of these circulating transferrin receptors, about 80% of which originate from erythrocyte precursors, is directly proportional to the amount of transferrin receptor expressed by the cells. This means that when serum transferrin receptor levels go up, it is usually due to red cells being starved for iron. Another factor to consider when studying serum transferrin receptors is that any time there is an increased reticulocyte count, there will be higher levels of transferrin receptors. Accordingly, conditions associated with erythropoiesis, such as hemolytic anemia or sickle cell anemia, will result in higher sTfR. Importantly though, sTfR is not elevated in the anemia of chronic disease. We conducted a study of 62 patients 4 in whom iron deficiency was confirmed either through bone marrow aspirate or response to iron therapy. This study showed that ferritin testing with a low cutoff (<12 ng/ml) was very specific, but had very poor sensitivity. When the ferritin cutoff was raised (<30 ng/ml), sensitivity was raised to 92% without losing any specificity. Soluble transferrin receptor in this study was also found to be very sensitive and relatively specific, but had a low positive predictive value. This low predictive value of sTfR, along with the good performance of the ferritin test in this population, led us to conclude sTfR should be reserved mainly for patients with anemia of chronic disease, such as those with rheumatoid arthritis. The results of this study are summarized in Table 1. Table 1. Mast, et al. (Clin Chem; 1998) Sensitivity Specificity PPV NPV Ferritin-12 25 98 75 84 Ferritin-30 92 98 92 98 sTfR 92 84 98 58 To summarize the use of the soluble transferrin receptor, it is a sensitive test for iron deficiency, but does not differentiate iron deficiency from other causes of increased erythropoiesis, which may result in a low positive predictive value. It is, however, useful for differentiation of iron deficiency from anemia of chronic disease. Regarding reticulocyte hemoglobin content (CHr), we must first understand that reticulocytes are the stage of the red cells in which they have almost matured - right after they are released from the bone marrow but before they have completely matured into a red blood cell. As immature cells, the reticulocytes still contain RNA and can be differentiated from mature red cells. This means that you can get a sort of 'snap shot' of recent iron available for incorporation into red blood cells by using reticulocyte hemoglobin content. The reticulocyte lifespan is typically about four days, but three of these days are in the bone marrow and only one day is in the peripheral blood. So, by looking at the reticulocyte hemoglobin content, the measure of iron available for incorporation at a point three days previously is determined. Reticulocyte hemoglobin content is useful as an early measure of functional iron deficiency because the only cells being measured are those recently released from the bone marrow. This means that CHr is going to be very sensitive in detecting recent iron deficiency, and that it can be used to indicate whether a given patient is responding to iron therapy more quickly than hematocrit measures. We recently sought to assess the clinical utility of reticulocyte hemoglobin content for prediction of bone marrow iron stores in 87 United States military veterans. In this study, participants' CHr, ferritin, percent transferrin saturation, and mean corpuscular volume (MCV) were prospectively measured in patients undergoing bone marrow aspiration. Prussian Blue staining of participants' bone marrow aspirate was used as the gold standard assay of iron status. The peripheral blood tests were submitted to be performed as routine tests in the laboratory, meaning that these samples received no special handling. Additionally, 34 non-anemic medical students were recruited to use as a comparison group. Results showed clearly that measures of reticulocyte hemoglobin content were lower in the 21 of 87 study group patients found to be iron-deficient based on the absence of stainable iron in their aspirate. The iron-deficient study participants had an average CHr of 26.3 pg, while the medical student control participants averaged 30.8 pg - about the same as the average of the iron-replete members of the study group. (Table 2). Table 2. Comparison of the CHr in iron replete and iron deficient patients to non-anemic medical students. Average CHr (pg) CHr Range (pg) Medical Students 30.8 28.8-32.9 Iron-Replete Patients 30.7 22.8-43.7 Iron-Deficient Patients 26.3 21.0-36.4 It was determined that 27 pg was the optimal cutoff value to differentiate iron-deficient from iron-replete patients in terms of reticulocyte hemoglobin content. Fourteen of 21 iron-deficient patients had a CHr less than 27 pg, resulting in a sensitivity of 66.7% for this test. Of those iron-deficient patients whose CHr measures were not below the cutoff, two had received four units of packed red blood cells within 24 hours prior to the bone marrow exam, and two were undergoing oral iron therapy. A fifth iron-deficient patient with a CHr level above the cutoff was caused by an increased MCV(CHr is determined by MCV multiplied by hemoglobin concentration) present because of a concomitant vitamin B12 or folate deficiency. In terms of specificity, only six of 66 iron replete patients had a CHr measure of less than 27 pg - a specificity of 91%. Of these six patients, two had ß thalassemia and a third had a clinical history of iron deficiency anemia. Data from this study showed, based on receiver operator curve analysis, that reticulocyte hemoglobin content was the best indicator of iron deficiency when compared to ferritin, transferrin saturation, or MCV. In conclusion, when looking at peripheral blood tests for iron deficiency, ferritin is a highly specific test, but has low sensitivity, and the other tests traditionally used for iron deficiency add little diagnostic power to that of ferritin alone. The soluble transferrin receptor and reticulocyte hemoglobin content (CHr) are useful newer tests for detecting iron deficiency that have higher sensitivity and specificity for iron deficiency than other traditionally used tests. However, abnormal hemoglobin related to thalassemia can produce false-positive results for iron deficiency in both tests, and therefore results from these tests should be interpreted in the context of the patient's overall erythrocyte physiology. It is hoped that a method of combining measures of ferritin, reticulocyte hemoglobin content, and soluble transferrin receptor can be developed to give an accurate indication of whether or not a given patient is truly iron-deficient, independent of performing a bone marrow biopsy. References 1. 2. 3. 4. Lough M, Egan EL, O'Cearbhaill HG: Diagnosing iron deficiency in a hospital population. Ir J Med Sci 989;158:108-109. Burns ER, Nahum S, Lawrence C, Wenz, B: Clinical utility of serum tests for iron deficiency in hospitalized patients. Am J Clin Path 1990;93:240-245 Murthy GD, Pasquale D, Chu RC, Lansing LS, Tsan MF, Gershman LC, Chikkappa G: Noninvasive diagnosis of iron deficiency. Fed Pract 1998;15:13-25 Mast AE, Blinder MA, Gronowski A, Chumley C, Scott MG: The clinical utility of the serum transferrin receptor in the evaluation of iron deficiency anemia. Clin Chem 1998; 44:45-51