08ostomy
advertisement

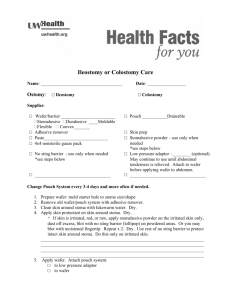
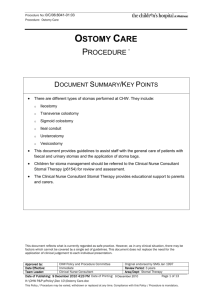
OSTOMY (ILEOSTOMY, COLOSTOMY) CARE - NEONATAL Department NICU PURPOSE To outline the care of an infant who has a colostomy or ileostomy. DEFINITIONS Colostomy: Is a surgically created opening in the large bowel. The location depends upon the site of disease or trauma. Therefore, ascending, transverse, descending or sigmoid describe the location. A colostomy may be end, loop or double barrel. When the distal portion of the large bowel and the rectum have been resected, the proximal limb is brought out as an end colostomy. Sometimes the distal limb is not resected, but is oversewn and replaced in the pelvis. A double-barrel colostomy is performed by exteriorizing both the proximal and distal ends of the bowel. This is called an end colostomy (proximal stoma) with a mucus fistula (distal stoma). Ileostomy: Is an opening into the ileum or terminal portion of the small intestine. Stool consistency depends on the location of the ostomy. EQUIPMENT Appropriate size ostomy bag Stomahesive paste 3 mL syringe Ostomy wafer (if not already applied to ostomy bag) Gauze pads Sterile water 2 – Heelwarmers Gloves PROCEDURE ASSESSMENT 1. Inspect stoma appearance at least every 12 hrs. The stoma should be moist, red and shiny. 2. Inspect patient’s abdomen for softness at least every 6 hours. 3. Inspect peristomal skin for signs of erythema and excoriation at least every 12 hours (when bag not in use) and at bag changes. 4. Assess stool output for consistency and volume at least every 12 hours. Transverse or descending colostomy: Stool output is thick liquid to soft-formed. Ascending colostomy: Stool is thin to thick liquid. Ileostomy: Stool is watery to thick liquid and is highly corrosive to the skin. 5. Assess need for initial bag placement. Initially baby may only require 2x2’s moistened with vaseline over stoma(s) until output increases, usually after 3 days. If this is the case, change vaseline gauze every 4 hours to avoid adherence to stoma. 6. Assess need for bag change. Change bag whenever it is not intact. Ideally bag should stay on for at least 24 hours. 7. Assess need for emptying bag. Bag should be emptied when it is one-third to one-half full. OSTOMY (ILEOSTOMY, COLOSTOMY) CARE - NEONATAL 2 of 3 INTERVENTIONS 1. Application of appliance: (When possible, enlist the assistance of a second person). Place a small amount of stomahesive in 3 mL syringe. Cut out middle of wafer (area inside plastic ring) with scalpel. Save middle portion. Trace stoma pattern onto wafer. Cut holes for stomas out of wafer using sharp scissors. Save paper from back of wafer to use for future pattern (if not previously done). If pouching two stomas, be sure wafer covers skin around both stomas allowing no exposed skin between each. Remove old pouch (if applicable with gauze pads moistened with water). Cleanse skin around stoma with water and dry thoroughly. Inspect stoma color and peristomal skin at this time. Take syringe with stomahesive paste and squeeze out small amount of paste around each stoma. Premature infant skin is very permeable to topical products. There is a high rate of transdermal absorption. Products such as stomahesive have a high alcohol content, therefore application should be limited. Position wafer over stomas. Place two heel warmers over stomas and wafer. Hold for a full two minutes. This allows the wafer to adhere to the skin. Position and place ostomy bag in lateral position to allow for easy drainage. Place a heel warmer over the ostomy bag and wafer. Hold for one full minute. This will allow the bag to adhere to wafer. 2. Emptying pouch (Perform when 1/3rd to ½ full) Put on non-sterile gloves. Open the bottom of bag over a disposable diaper or container and allow to drain. Use a syringe filled with cool water to rinse the stool out of the pouch. Dry end of pouch and secure with fastener or rubber band. Remove gloves and wash hands. REPORTABLE CONDITIONS Notify MD of the following: Changes in stoma color (deep purple/black) or size Abdominal distension or firmness Bilious emesis Excessive bleeding from stomas No stool output for 24 hours (once the stoma becomes productive). Breakdown of the peristomal skin. TEACHING 1. Explain need for ostomy and future surgeries to parents. 2. Explain appliance change to parents and enlist assistance when available. 3. Assist in diminishing parent’s feelings of helplessness and loss of control by incorporating any preferences for their infant’s ostomy care into the plan of care. OSTOMY (ILEOSTOMY, COLOSTOMY) CARE - NEONATAL 3 of 3 DOCUMENTATION Document the following on the nursing flowsheet: a. Stool output/consistency/color every 12 hours. b. Stoma appearance c. Peristomal skin integrity d. Abdominal girths every 6 – 12 hours. e. Presence of emesis and color f. Abdominal softness/firmness REFERENCES/ REGULATORY STANDARDS Merenstein, G. B. & Gardner, S. L. (2006). Handbook of neonatal intensive care. St. Louis; Mosby. MacDonald, M. G. & Ramasethu, J. (2002). Atlas of procedures in neonatology (3rd ed.). Philadelphia; Lippincott. Origination Date Approval Date Review Dates 1/00, 7/03, 1/04, 7/05, 8/06, 5/07 Committee Approvals: Regional Neonatal Joint Practice: 1/00, 7/03, 1/04, 7/05, 8/06, 5/07 Pediatric Committee: 10/03, 2/04 Infection Control/Pharmacy & Therapeutics: 11/03, 4/04 MEC: 1/04, 6/04, 9/06 Policy & Procedure Committee: 8/05, 10/06 Operations Committee: 8/05, 10/06 Community Board: 9/05, 12/06 Central Standards Committee: 2/04, 6/04