1 Medical Coding Exam System - Week 3 Day 4 Practice Exam
advertisement
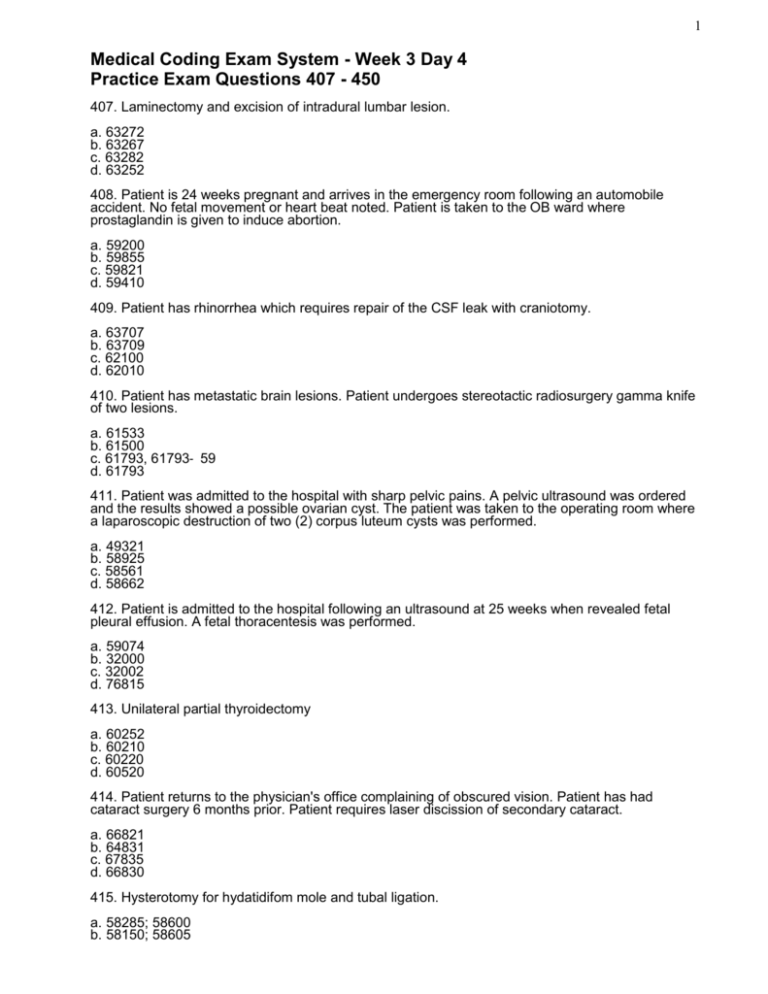
1 Medical Coding Exam System - Week 3 Day 4 Practice Exam Questions 407 - 450 407. Laminectomy and excision of intradural lumbar lesion. a. 63272 b. 63267 c. 63282 d. 63252 408. Patient is 24 weeks pregnant and arrives in the emergency room following an automobile accident. No fetal movement or heart beat noted. Patient is taken to the OB ward where prostaglandin is given to induce abortion. a. 59200 b. 59855 c. 59821 d. 59410 409. Patient has rhinorrhea which requires repair of the CSF leak with craniotomy. a. 63707 b. 63709 c. 62100 d. 62010 410. Patient has metastatic brain lesions. Patient undergoes stereotactic radiosurgery gamma knife of two lesions. a. 61533 b. 61500 c. 61793, 61793‐ 59 d. 61793 411. Patient was admitted to the hospital with sharp pelvic pains. A pelvic ultrasound was ordered and the results showed a possible ovarian cyst. The patient was taken to the operating room where a laparoscopic destruction of two (2) corpus luteum cysts was performed. a. 49321 b. 58925 c. 58561 d. 58662 412. Patient is admitted to the hospital following an ultrasound at 25 weeks when revealed fetal pleural effusion. A fetal thoracentesis was performed. a. 59074 b. 32000 c. 32002 d. 76815 413. Unilateral partial thyroidectomy a. 60252 b. 60210 c. 60220 d. 60520 414. Patient returns to the physician's office complaining of obscured vision. Patient has had cataract surgery 6 months prior. Patient requires laser discission of secondary cataract. a. 66821 b. 64831 c. 67835 d. 66830 415. Hysterotomy for hydatidifom mole and tubal ligation. a. 58285; 58600 b. 58150; 58605 2 c. 51900; 58605 d. 59100; 58611 416. Decompression internal auditory canal. a. 69979 b. 69915 c. 69970 d. 69960 417. Patient was admitted with a cystocele and rectocele. An anterior colporrhaphy was performed. a. 57250 b. 57260 c. 57240 d. 57110 418. Patient comes in through the emergency room with a laceration of the posterior tibial nerve. Patient is taken to the operating room where the nerve requires transposition and suture. a. 64856 b. 64831; 64832; 64876 c. 64840; 64874 d. 64834; 64859; 64872 419. Patient undergoes total thyroidectomy with parathyroid autotransplantation. a. 60240; 60512 b. 60520; 60500 c. 60260; 60512 d. 60650; 60500 420. Modified radical mastoidectomy a. 69511 b. 69505 c. 69635 d. 19180 421. Aphakia penetrating corneal transplant. a. 65755 b. 65730 c. 65750 d. 65765 422. Patient undergoes enucleation of left eye and muscles were reattached to an implant. a. 65135-LT b. 65105-LT c. 65730-LT d. 65103-LT 423. Patient has an incompetent cervix which was repaired using a vaginal cerclage. a. 57700 b. 57531 c. 59320 d. 53902 424. Robert is admitted with emphysematous nodules. He undergoes, without complication, a wedge resection of the right upper lobe. Robert developed atelectasis post-operatively that required monitoring with portable chest x‐ rays and extended his length of stay. a. 518.89, 997.3, 32.3 b. 997.3, 518.0, 518.89, 32.29 c. 492.8, 997.3, 518.0, 32.29 d. 518.89, 518.0, 32.29 492.8 Other emphysema 518.0 Atelectasis 3 518.89 Other diseases of lung, NEC 997.3 Respiratory complications 32.29 Local excision/destruction of lung tissue or lesion 32.3 Segmental resection of lung 425. Grace has pneumonia. She also has acute exacerbation of COPD. a. 491.21 b. 486, 491.21 c. 491.20, 486 d. 486 426. Open I&D of a deep abscess of the cervical spine: a. 22010 b. 22015 c. 10060 d. 10140 427. Patient presents with a history of upper abdominal pain. Cholangiogram was negative and patient was sent to the hospital for ERCP. During the procedure, the sphincter was incised and a stent was placed for drainage. a. 43260; 43262; 43624 b. 43262; 43269 c. 43267 d. 43262; 43268 428. Caloric vestibular test using air: a. 92543; 92700 b. 92543; 92543 c. 92700 d. 92543 429. Blood transfusion of three units of packed red blood cells a. 36430 b. 36430; 36430; 36430 c. 36460 d. 36455 430. The physician’s office note states: “Counseling visit, 15 minutes counseling in follow up with a patient newly diagnosed with diabetes.” If the physician reports code 99214, which piece of documentation is missing to substantiate this code? a. chief complaint b. history c. exam d. total length of visit 36430 Transfusion, blood or blood components 36455 Exchange transfusion; blood, other than newborn 36460 Transfusion, intrauterine, fetal 431. Patient is admitted to the hospital with facial droop, left-sided paralysis. CT scan of the brain shows subdural hematoma. Burr holes were performed to evacuate the hematoma. a. 852.20; 61156 b. 432.1; 61314 c. 432.1; 61154 d. 852.20; 61150 432. A patient initially consulted with Dr. Ramos at the request of Dr. Lee, the patient’s primary care physician. Dr. Ramos examined the patient, prescribed medication, and ordered tests. Additional visits to Dr. Ramos’ office for continuing care would be assigned from which E&M section? a. office and other outpatient services, new patient b. office and other outpatient services, established patient c. office or other outpatient consultations, new or established patient d. confirmatory consultations, new or established patient. 4 433. The discharge diagnosis for this inpatient encounter is “rule out myocardial infarction.” The coder would assign a. a code for a myocardial infarction b. a code for the patient’s symptoms c. a code for an impending myocardial infarction d. no code for this condition 434. Down syndrome, Edwards’ syndrome and Patau syndrome are all examples of defects. a. musculoskeletal b. chromosomal c. genitourinary tract d. digestive system 435. A final progress note is appropriate as a discharge summary for a hospitalization in which the patient a. dies within 24 hours of admission b. has no co-morbidities or complications during the episode of care. c. was admitted within 30 days with same diagnosis d. was an obstetric admission with a normal delivery and no complications. 432.1 Subdural hematoma 852.20. Subdural hemorrhage following injury without mention of open intra-cranial wound. Unspecified state of unconsciousness. 61150 Burr hole(s) or trephine; with drainage or brain abscess or cyst. 61154 Burr hole(s) wit evacuation and/or drainage of hematoma, extradural or subdural 61156 Burr hole(s); with aspiration of hematoma or cyst, intracerebral 61314 Craniectomy or craniotomy for evacuation of hematoma, infratentorial; extradural or subdural 436. In reviewing a medical record for coding purposes, the coder notes that the discharge summary has not yet been transcribed. In its absence, the best place to look for the patient’s response to treatment and documentation of any complications that may have developed during this episode of care is in the a. doctors progress note section b. operative report c. history and physical d. doctors orders 437. George underwent a laparoscopic cholecystectomy with exploration of the common duct. How should you report this procedure? a. 47600, 47715-51 b. 47564 c. 47610 d. 47562, 47564-59 438. Today, Juan presents to the radiation oncologists solely to receive radiation treatment for his secondary stomach wall cancer. The primary neoplasm was diagnosed as anal sphincter cancer. How should you report these diagnoses codes? a. 151.9, 197.8 b. V58.0, 197.8, 154.2 c. 154.2, 197.8, V58.0 d. 197.8, 151.9 439. Which of the following would NOT require HCPC/CPT codes? a. hospital ambulatory surgery visit b. hospital outpatient visit c. clinic visit d. hospital inpatient visit 440. Staging a. refers to the monitoring of incidence and trends associated with a disease b. is continued medical surveillance of a case c. is a system for documenting the extent or spread of cancer 5 d. designates the degree of differentiation of cells 441. An anesthesiologist administers anesthesia for a male patient prior to the surgeon performing a total hip replacement. The patient is 75 years old and suffers from mild hypertension. How should you code the anesthesia services? a. 01214, 99100-59 b. 01214-47 c. 01214-P2, 99100 d. 01214-P3 442. Patient is treated for congestive heart failure with pleural effusion. A therapeutic thoracentesis is performed. a. 511.9, 34.91 b. 428.0, 34.04 c. 428.0, 511.9 d. 428.0, 511.9, 34.91 443. David was experiencing chronic fatigue and was experiencing flu like symptoms. Blood testing indicated that he had hepatitis C. A pecutaneous lover biopsy was performed to determine the stage of the disease. a. 070.51, 487.1, 780.79, 50.12 b. 070.41, 50.11 c. 070.51, 487.1, 50.11 d. 070.51, 50.11 444. Dale is admitted with emphysematous nodules. He undergoes, without complication, a wedge resection of the right upper lobe. Dale developed atelectasis post-operatively that required monitoring with portable chest x-rays and extended his length of stay. a. 518.89, 997.3, 32.3 b. 997.3, 518.0, 518.89, 32.29 c. 492.8, 997.3, 518.0, 32.29 d. 518.89, 518.0, 32.29 445. Abbreviations and symbols are to be used in patient records only when a. There is an explanatory legend included in the documentation b. abbreviations and symbols are never used c. they can be found in a medical dictionary d. they are part of a published facility list that has been approved by the medical staff. 446. The term that indicates this is the type of code for which the full code description can be known only if the common part of the code (the description preceding the semicolon) of a preceding entry is referenced: a. stand-alone b. indented c. independent d. add-on 492.8 Other emphysema 518.0 Atelectasis 518.89 Other diseases of lung, NEC 997.3 Respiratory complications 32.29 Local excision/destruction of lung tissue or lesion 32.3 Segmental resection of lung 447. What code would be used to report a massive debridement of an open abdominal wound, including subcutaneous tissue and muscle? a. 11000 b. 11010 c. 11042 d. 11043 448. In reviewing the medical record of a patient admitted for a left herniorrhaphy, the coder discovers an extremely low potassium level on the laboratory report. In examining the physician’s orders, the coder notices that intravenous potassium was ordered. The physician has not listed any 6 indication of an abnormal potassium level or any related condition on the discharge summary. The best course for action for the coder to take is to: a. confer with the physician and ask him or her to list the condition as a final diagnosis if he or she considers the abnormal potassium level to be clinically significant. b. code the record as is. c. code the condition as an abnormal blood chemistry. d. code the abnormal potassium level as a complication following surgery. 449. In general, all three key components (history, physical examination and medical decision making) for the E/M codes in CPT should be met or exceeded when a. the patient is established. b. a new patient is seen in the office c. the patient is given subsequent care in the hospital d. the patient is seen for follow up inpatient consultation 450. Lisa Lopez was admitted to the ambulatory care unit of the hospital for a planned cholecystectomy for cholelithiasis. Shortly before surgery, Lisa developed tachycardia, and the surgery was canceled. After a thorough work‐ up for tachycardia, Lisa was discharged. This outpatient admission should be coded in the following sequence: a. V-code for canceled surgery, tachycardia, cholelithiasis b. tachycardia, V-code for canceled surgery, cholelithiasis c. cholelithiasis, V-code for canceled surgery. d. cholelithiasis, V-code for canceled surgery, tachycardia. 7 Medical Coding Exam System - Week 3 Day 4 Practice Exam Answers 407 - 450 407. a. 408. b. 409. c. 410. c. 411. d. 412. a. 413. b. 414. a. 415. d. 416. d. 417. c. 418. c. 419. a. 420. b. 421. c. 422. b. 423. c. 424. c. 425. b. 426. a. Codes 10060 and 10140 are used for I&D’s of superficial abcesses, 427. d. Radiology codes would be used for the supervision and interpretation. 428. c. Code 92543 is for use when an irrigation substance is used. 429. a. Report this code only once regardless how many units were given. 430. d. In order to use time as a factor in determining the appropriate E&M code, the total time spent with the patient, as well as the amount of time spent in counseling, must be recorded. 8 431. c. Codes starting with 852 are considered to be traumatic injuries. No injury was stated in the case, so 432.1, non-traumatic subdural hematoma would be the appropriate code. 432. b. Consultation codes can no longer be coded when the physician has taken an active part in the continued care of the patient. 433. a. When a diagnosis is preceded by the phrase “rule out” in the inpatient setting, the condition is coded as though it is confirmed. 434. b. chromosomal 435. d. A final note may substitute for a discharge summary for patients admitted for less than 48 hours with minor problems, uncomplicated deliveries and for normal neonates. 436. a. The physician releasing the patient should write a final note of summary of the patient’s course of treatment, sating the patient’s condition at discharge, and instructions for the patient’s activity, diet and medications as well as any follow up appointments or instructions. If patients expires, the final notes describe the circumstances regarding the death, the findings, the cause of death and whether or not an autopsy was performed. 437. b. The code 47564 would report a laparoscopic procedure. The code 47610 would report an open procedure 438. b. General guidelines in the ICD9CM Manual, Chapter 2, state that neoplasms give specific details related to sequencing order to report codes. Notice, under Chapter 2, a., that “treatment directed at the malignancy indicates assignment of the appropriate treatment code (radiation) as first listed followed by site being treated.” Notice, under Chapter 2, b., that “treatment of secondary site would be reported next, followed by primary site that still exists.” 439. d. The hospital inpatient visit would not be coded using HCPCS/CPT codes. Hospital inpatient visit diagnoses and procedures are coded using ICD-9-CM codes. 440. c. Staging is a term used to refer to the progression of cancer. In accessing most types of cancer, a method (staging) is used to determine how far the cancer has progressed. The cancer is described in terms of how large the main tumor is, the degree to which it has invaded surrounding tissue, ad the extent to which it has spread to lymph glands or other areas of the body. Staging not only helps to assess outlook but also the most appropriate treatment. 441. c. Anesthesia codes must have a physical status modifier. This question has qualifying circumstances based on the patient age. 442. d. 443. d. Fatigue and flu like symptoms/signs of hepatitis would not be coded. 444. c. The atelectasis is coded because it required monitoring and extended his length of stay. 445. d. Any abbreviations permitted in a patient record should be understood by all. Use of abbreviations is strictly prohibited when documenting the final diagnoses and procedures for an episode of care. 9 446. b. The indented code indicates this is the type of code for which the full code description can be known only if the text preceding the semicolon of a preceding entry is referenced. The CPT manual is formatted in this manner in order to save space. 447. d. 11043 identifies the debridement of the skin, subcutaneous tissue, and muscle. 448. a. A coder should never assign a code on the basis of laboratory results alone. If findings are clearly outside the normal range and the physician has ordered additional testing or treatment, it is appropriate to consult with the physician as to whether a diagnosis should be added or whether the abnormal finding should be listed. 449. b. All three components (history, physical examination and medical decision making) are required for new patients and initial visits. At least two of the three components are required for established patients, subsequent visits and follow-up consultations. 450. d. There are V-codes that indicate various reasons for canceled surgery. Review codes V64.0x, V64.1, V64.2, and V64.3. As usual, the principal diagnosis is always the reason for admission—in this case, the cholelithiasis. The contraindication (the tachycardia) should also be coded.