Trocar placement
advertisement

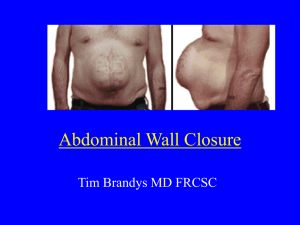
Patient positioning 1.) The patient is placed in supine position on the operating room table. (There is an inflatable transfer device placed on the stretcher in the holding area) 2.) The arms are extended laterally on arm boards and secured in place. 3.) Following intubation, a foley is placed and draped beneath the left leg. 4.) A seatbelt is used at the hip level to secure the patient in place. 5.) Sequential compression devices are placed bilaterally and activated prior to induction of anesthesia. 6.) A footboard is secured in place, keeping the patient's plantar surfaces flat against the board, to provide support when the table is in maximal reverse trendelenberg position. 7.) A blue towel is taped around both ankles to prevent rotation of the lower legs/feet. 8.) The fast clamp for the liver retractor is placed at the level of the patient's right hip. Trocar placement Objective: Place six ports perpendicular to the abdominal wall Position: Steep reverse Trendelenberg Instruments: Trocars, 2-0 silk suture x 2, insufflation tubing All skin incisions for ports are made following verification of the positioning by needle puncture, and injection of local anesthetic. The incisions are made with an 11-blade. All trocars should be inserted perpendicularly to the abdominal wall. When the blade tip is visible within the abdominal cavity, the tip is redirected toward the camera in order to avoid puncture of abdominal contents. Port 1: Through a 5 mm incision, a Veress needle is placed at the left subcostal anterior axillary line. A 2-0 silk suture is placed for securing the port later. Following insufflation of the abdomen to a pressure of 15 mm Hg, the Veress needle is exchanged for a 5 mm port. A 5 mm 45 degree laparoscope is then used to visualize the peritoneal cavity. Port 2: A 12 mm port placed 1 to 2 cm to the left of midline and one hand width inferior to Port 1. This will be the port used for the laparoscope for most of the case. The patient is placed in steep reverse Trendelenberg position. Port 3: A 5 mm port is placed in the right upper quadrant in the midclavicular line, at the edge of the liver. This port is connected to a second insufflator source. Port 4: A 12 mm port is placed in the right upper quadrant in the midclavicular line, at least one hand's width lateral to port 2 and one hand's width inferior to port 3. Port 5: A 5 mm port placed in the right midaxillary line, at the edge of the liver. This is used for the liver retractor. The 5 mm laparoscope is exchanged for a 10 mm laparoscope which is inserted through port 2. Port 6: A 5 mm port is placed in the left midaxillary line, one hand's width inferior and lateral to port 1. This port is anchored with a silk suture. Perils to avoid • Placing trocar at an angle • Placing trocars too close together • Placing subcostal trocars too low Gastric pouch Objective: create 15ml gastric pouch by separating the stomach with linear staplers Position: Steep Reverse Trendelenberg Instruments: Surgeon: Harmonic and alligator grasper Linear staplers Roticulating grasper Assistant: 2 alligator graspers 1. Make sure that the OG tube is removed by the anesthesiology staff. Confirm that it has been removed. 2. Create a window in the gastro-hepatic ligament (filmy portion). Identify the left gastric artery and create a posterior gastric tunnel inferior to the left gastric artery 3. Stapler 60mm white load x 1 to divide the omentum up to the gastric lesser curvature below 2nd branch of left gastric artery 4. Stapler 60mm blue load x 4-5 to divide the stomach and create a 15ml gastric pouch 5. The assistant should pull away the omentum and pull the fundus inferiorly with an alligator 6. When approaching the greater curvature and before the last blue load, use the suction to create a window in the gastro-splenic ligament 7. The assistant lifts the gastric remnant and the back of the stomach is cleaned from adhesions with the harmonic scalpel to create a free retrogastric space Perils to avoid • Grasping the gastrohepatic omentum with a grasper • Injuring pancreas, splenic vessels, liver, spleen • Making pouch too small or too large • Tearing stomach with grasper Jejunojejunostomy Objectives: 1. Divide jejunum 40 cm distal to the ligament of Treitz 2. Measure Roux limb 3. Create jejuno-jejunostomy Position: Flat Position Instruments: Surgeon: Duckbill graspers (long one in right hand, short one in left) Endoscopic staplers Endostitch (2-0 Surgidac and 2-0 silk) Alligator grasper Clip applier if needed Assistant: Duckbill graspers 1. Reflect the greater omentum superiorly and tuck it beneath the liver to expose the transverse mesocolon 2. Find ligament of Treitz 3. Pull out the proximal jejunum to create a C loop 4. Measure 40 cm from the ligament of Treitz 5. Stapler 60mm white load x1 to divide small bowel ("airplane maneuver") 6. Stapler 45mm gray load x1 to divide the mesentery (close the stapler and check bowel viability prior to firing) 7. Check the Roux limb length and double barrel the two limbs 8. Mark the Roux limb: Sew Penrose drain to the antimesenteric corner of the Roux limb with Surgidac Endostitch 9. Measure 75 cm (if BMI < 50) or 150 cm (if BMI > 50) Roux limb 10. Antimesenteric stay suture Roux limb to biliopancreatic limb with Surgidac Endostitch 11. Create enterotomies (first on the corner of the biliopancreatic limb with tips up, and then on the antimesenteric border of the Roux limb with tips down) with harmonic scalpel 12. Stapler 60mm white load x1 to create side to side jejuno-jejunostomy. Hold the margins of the enterotomies into the stapler to avoid sliding. Keep stapler elevated. 13. Corner suture to keep the two limbs parallel with Surgidac Endostitch 14. Stay suture to approximate the edges of the enterotomy with Surgidac Endostitch to the right of the anastomotic staple line 15. Position enterotomy between 2 and 8 o'clock. Staple with 60mm white load x1 to close enterotomies. Include minimal amount of tissue to avoid narrowing of the anastomosis 16. Brolin's antiobstruction stitch between the antimesenteric aspect of the Roux limb and the biliopancreatic limb pouch with Surgidac Endostitch 17. Close mesenteric defect. Start at the inferior aspect of the defect and apply running silk suture sewing superiorly (small bites to avoid mesenteric vessels) and tie to the tail of the Brolin's stitch. Perils to avoid • Tearing bowel with graspers • Making ends of divided bowel ischemic • Placing sutures anywhere except antimesenteric borders • Placing enterotomies anywhere except antimesenteric borders • Making enterotomies too large or stretching enterotomies • Backwall injury to bowel with stapler • ***Releasing grasp on bowel when using stapler • Narrowing anastomosis with closure of enterotomy • Creating kink in small bowel with Brolin stitch, corner stitch, or mesenteric closure • Neglecting bleeding from staple line • Creating bleeding in mesentery during closure Creating the mesocolic window Objectives: Create a mesocolic window Pass the Roux limb through the retrocolic retrogastric space Position: Flat Position Instruments: Surgeon: Alligator grasper Harmonic scalpel Roticulating grasper Assistant: 2 Alligator graspers 1. Locate the ligament of Treitz 2. Grasp a fold of mesocolon 2 cm lateral and above the ligament of Treitz 3. Harmonic scalpel to create the mesocolon window 4. Find the excluded stomach with an alligator grasper and bring it through the mesocolon window. The assistant should hold the stomach firmly with an alligator while the surgeon brings up the Roux limb 5. Find the Roux limb (Penrose drain) 6. Make sure that the Roux limb is not twisted (mesentery should lie medially) 7. Roticulating grasper to hold the Penrose drain and pass the Roux limb into the mesocolon window and behind colon and excluded stomach. Duckbill grasper to hold the antimesenteric border of the Roux limb and keep it from twisting Perils to avoid • Causing bleeding in mesocolon (incision too anterior) • Injuring pancreas (incision too posterior) • Letting go of excluded stomach • Twisting Roux as it is passed • Penrose falling off • Injuring colon Gastrojejunostomy Goal: anastomose jejunal Roux limb to gastric pouch Instruments: Surgeon: 2 Duckbills Roticulating grasper Harmonic Scalpel Endostitch Device Endoscopic stapler (45 mm blue) Curved bowel clamp Assistant: 2 Duckbills Suction and Irrigation Endoshears 1. Bring the Roux loop (Penrose drain) in the upper abdomen through the mesocolic window using an articulating grasper and a duckbill. Check that the Roux limb is not twisted (mesentery should be towards the left). Pull up the Roux limb with 2 duckbills. The assistant should hold the Roux limb with a duckbill by the Penrose drain. Expose the posterior surface of the Roux limb. 2. Approximate the Roux limb to the gastric pouch. 3. Running Endostitch Surgidac 2-0 full length x 2 for posterior external layer from posterior side of Roux limb, 1/2 cm from antimesenteric border, to posterior stomach. Follow yourself and do not lock suture. For the 2nd suture, suture the antimesenteric border of Roux to the posterior stomach x 2 bites, then to staple line x 2. Tie to the loop of suture. 4. Creation of the gastrostomy with the harmonic scalpel. 5. Creation of the jejunostomy with the harmonic scalpel. Stay close to the pouch. 6. Stapler 45mm blue load x 1 to create a 2 cm gastro-jejunostomy. The operating surgeon should hold the gastric edge tightly with an alligator; avoid slippage. The assistant should hold the jejunal edge at the 2 cm mark on the stapler with a duckbill. 7. Endostitch Polysorb 2-0 full length x 2 to close the gastro-jejunostomy starting at the 2 corners of the defect. 8. Before tying the 2 ends of the suture, an upper endoscope (insufflation off) is passed through the anastomosis and into the proximal Roux limb by the assistant. The upper endoscope will act as a stent. Tie 2 ends of suture after endoscopy. 9. Remove Penrose drain. 10. Endostitch Surgidac 2-0 full length for anterior inverting external layer. 11. Curved bowel clamp to occlude the bowel. 12. Patient is placed in level position. 13. Irrigation to submerge the G-J anastomosis. 14. Insufflation with the upper endoscope to check for leaks. 15. Suction the fluid. 16. Insertion of the Jackson-Pratt drain posterior to the anastomosis. 17. Remove the liver retractor and bring out the J-P drain. Clamp drain with hemostat. Tips: -Make a new ridge on the Roux side for the posterior layer -Make the tail on the 2nd suture of the posterior layer short -Maek the tail of the loop short -Make the enterotomy on the stomach about 1 cm away from the loop (closer to the lesser curvature) -Hold on tightly to the stomach when firing the stapler -Suture the corners on the 1st anterior layer Endoscopy Objectives: 1. Prevent occlusion of gastrojejunostomy with suture closure 2. Calibrate stoma 3. Insufflation test of the integrity of the completed anastomosis Instruments: Endoscopist: endoscope, camera head attachment with adapter, lightsource, insufflator attachment, saline irrigation, bite block, +/- Surgilube 1. The gastrojejunal anastomosis is created as described in the earlier section. 2. When the gastrojejunal defect has been re-approximated but not yet fully closed with Surgidac, the assistant hands the camera to the scrub nurse and moves to the head of the bed. 3. The anesthesiologist should have already placed a bite block in the patient's mouth to protect the endoscope and endotracheal tube. Check to make sure that the patient is fully paralyzed. 4. The circulating nurse will assist in creating a picture in picture (PIP) image of the endoscopy image within the operative field image. 5. Check the endoscopy equipment: Make sure the camera head is attached correctly and that the PIP is working. Test both the suction and insufflation on the endoscope in the bucket of saline provided. 6. Turn the insufflation off prior to advancing the scope. Turn the ignition button on and the filter button off and assess the PIP image. 7. Use either the saline or Surgilube to lubricate the scope. Ask the anesthesiologist to assist by giving the patient a jaw thrust and to secure the position of the endotracheal tube. 8. The scope is held approximately 10-15cm from the end and the endoscopist uses the left hand on the large wheel and their right hand on the scope to both advance and steer. 9. Pass the end of the scope straight back into the esophagus similar to passage of a nasogastric tube. It should fall without resistance into the esophagus. Once in the esophagus, the scope should be passed straight into the gastric pouch without any need for steering. 10. Once the scope has reached the stomach, the lighted end is visualized on the operative image screen and passed carefully through the anastamosis and into the Roux limb approximately 10cm. Care must be taken not to disrupt the gastrojejunal anastamosis. The two ends of the Surgidac are tied to close the gastrojejunal defect using the endoscope as a stent. 11. The end of the endoscope is kept in the small bowel lumen using the PIP image and a curved bowel clamp is placed around the Roux limb distal to the scope by the surgeon. 12. The table is taken out of reverse Trendelenberg and is leveled. The assistant uses the suction-irrigator to submerge the gastrojejunal anastomosis in water. 13. After the froth from the irrigation has cleared, the insufflator is turned on (labeled "air" on the control box) and the endoscopist insufflates the anastomosis. If unable to insufflate, check the PIP image to place the scope in the center of the lumen. 14. The surgeon and assistant inspect the irrigation for any obvious bubbles escaping the anastomosis during insufflation. 15. After satisfactory inspection, the lumen is centered and the bowel is desufflated. The endoscope is withdrawn from the Roux limb and then entirely from the patient's esophagus. 16. The bowel clamp is removed, the remaining irrigation is suctioned out, and the anterior row of the G-J anastomosis is started. The assistant re-gowns and gloves and returns to the operative field once the endoscope has been thoroughly suctioned out with saline. Perils to avoid: Beware of pushing the scope into the small bowel mesentery during passage into the Roux limb. Do not insufflate before the bowel clamp is place and secure and the anastamosis has been submerged. Beware of disrupting the G-J anastomosis during passage of the scope into the Roux limb. Closing defects and trocar sites Objective: close transverse mesocolon opening and Petersen's defect with continuous silk suture Instruments: Surgeon: Duckbill Endostitch Assistant: Duckbills Endoshears Patient position: flat 1. Roll over the omentum and identify the transverse mesocolon window. 2. Endostitch Silk 2-0 full length x 2 to close the transverse mesocolon and the Petersen's defects. Lock the suture over the small bowel. Tie 2 ends together with a loose air knot. Objective: close 12 mm trocar sites Instruments: Surgeon: Carter-Thomason suture passer, 0 polysorb tie x 2 Assistant: Duckbill 1. Push the 12mm ports towards the head and insert the Carter-Thomason device (loaded with 0 polysorb) perpendicular to the trocar (aiming towards the head). The assistant grasps the suture and holds it for step 2. 2. Repeat, pushing the port towards the feet, aiming the suture passer towards the feet. Grasp the suture and pull through. Repeat for the other 12 mm port. 3. Remove ports under laparoscopic vision. Deflate pneumoperitoneum. 4. 2-0 Prolene for drain fixation 4-0 Polysorb to close skin, apply benzoin and steri-strips Apply primapore dressings Attach J-P drain to bulb