Item 11 Annual Infection Control Report 2010-11
advertisement
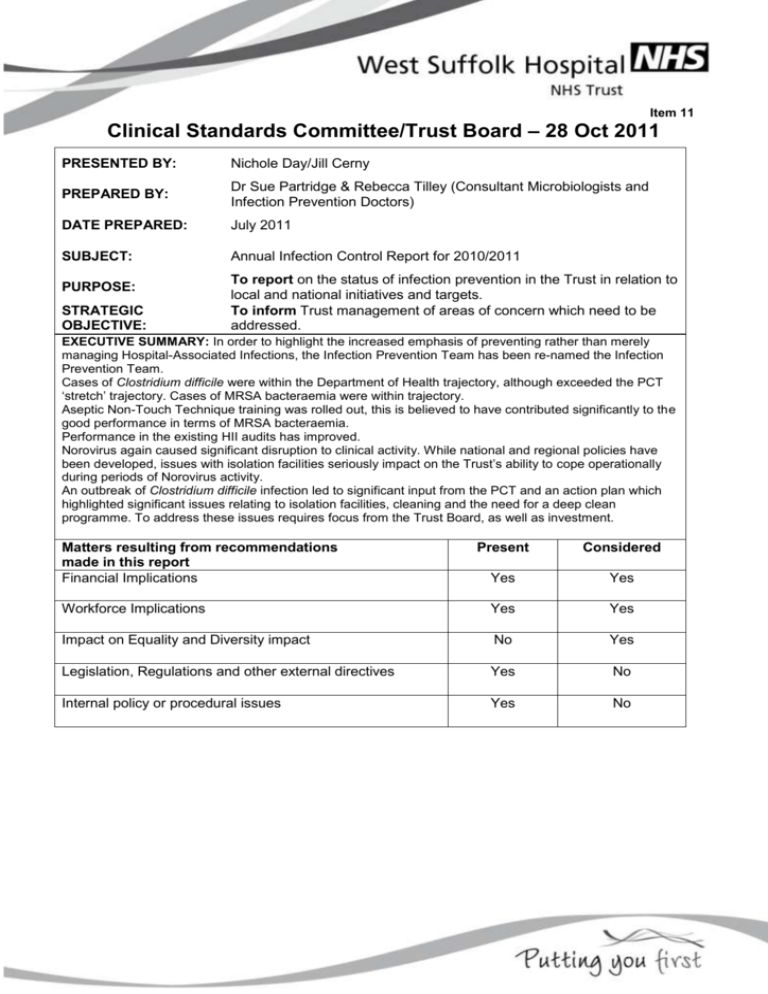
Item 11 Clinical Standards Committee/Trust Board – 28 Oct 2011 PRESENTED BY: Nichole Day/Jill Cerny PREPARED BY: Dr Sue Partridge & Rebecca Tilley (Consultant Microbiologists and Infection Prevention Doctors) DATE PREPARED: July 2011 SUBJECT: Annual Infection Control Report for 2010/2011 PURPOSE: STRATEGIC OBJECTIVE: To report on the status of infection prevention in the Trust in relation to local and national initiatives and targets. To inform Trust management of areas of concern which need to be addressed. EXECUTIVE SUMMARY: In order to highlight the increased emphasis of preventing rather than merely managing Hospital-Associated Infections, the Infection Prevention Team has been re-named the Infection Prevention Team. Cases of Clostridium difficile were within the Department of Health trajectory, although exceeded the PCT ‘stretch’ trajectory. Cases of MRSA bacteraemia were within trajectory. Aseptic Non-Touch Technique training was rolled out, this is believed to have contributed significantly to the good performance in terms of MRSA bacteraemia. Performance in the existing HII audits has improved. Norovirus again caused significant disruption to clinical activity. While national and regional policies have been developed, issues with isolation facilities seriously impact on the Trust’s ability to cope operationally during periods of Norovirus activity. An outbreak of Clostridium difficile infection led to significant input from the PCT and an action plan which highlighted significant issues relating to isolation facilities, cleaning and the need for a deep clean programme. To address these issues requires focus from the Trust Board, as well as investment. Matters resulting from recommendations made in this report Financial Implications Present Considered Yes Yes Workforce Implications Yes Yes Impact on Equality and Diversity impact No Yes Legislation, Regulations and other external directives Yes No Internal policy or procedural issues Yes No Risk Implications for West Suffolk Hospital (including any clinical and financial consequences): Sub-optimal care for patients with increased morbidity and mortality, including that associated with transmission of infections between patients. Increased length of stay and its associated costs, potential financial penalties levied by Commissioners. Mitigating Actions (Controls): Infection Prevention Policies and Guidelines, continual audit and feedback. Training and engagement of all clinical staff with Infection Prevention issues. Level of Assurance that can be given to the Committee from the report based on the evidence [significant, sufficient, limited, none]: Limited Recommendation to the Committee: The committee is asked to support the Infection Prevention Team in their attempts to implement effective guidance, maintaining patient safety as a priority over other targets. The need for improved isolation facilities should be addressed urgently. The massive increase in mandatory audit and surveillance places significant demands on the IPT which it is unable to meet in its current configuration. The Trust will need to identify resources (not necessarily within the IPT) if this additional activity is to be sustained. SECTION 1: Key Performance Indicators Detail performance indicators that provide an overview of the high quality, safe and effectiveness of the service/area. Clostridium difficile infection From 01-04-2010 to 31-03-2011 there were 37 cases of C. difficile in patients aged >2 years apportioned to the Trust. This was against a Department of Health trajectory of 51. The PCT had set a stretch trajectory of 29 which was revised to 42 after the outbreak. The cases included an outbreak on ward G4 in November/December. The outbreak investigation identified significant issues, which were addressed in an Action Plan. These included “Isolation” of patients with diarrhea in a shared side-room i.e. not isolated Decontamination facilities for patients’ drinking vessels Storage facilities for enteral feeds Arrangements for a Trust-wide deep clean programme Creation of a permanent decant ward (F7) The introduction of Hydrogen Peroxide fogging as part of the deep cleaning regime. Equipment was initially loaned and subsequently purchased by the Trust. The DH trajectory for 2011-12 is for cases not to exceed 32, the PCT stretch trajectory is 29. MRSA Bacteraemias From 01-04-20010 to 31-03-11 there were 0 cases of hospital-acquired MRSA blood stream infection reported from the Trust, against a trajectory of 4. The target for 2011-2012 is no more than 2 cases. Continued limitation of cases of MRSA bacteraemia requires rigorous implementation of ANTT (see below), compliance with Trust policy regarding MRSA screening and decolonisation of new admissions and in-patients (the frequency of this depending on the clinical area), and good management of urinary catheters. A multidisciplinary group is reviewing guidelines on catheter insertion and care. While screening and decolonisation of MRSA positive patients reduces the risk of transmission, lack of isolation facilities means that positive patients cannot all be accommodated in single rooms, which would further reduce the risk of transmission. Saving lives High Impact Intervention (HII) Audits Six HII care bundles are currently audited. These are: 1) Central venous catheter insertion and ongoing care 2) Peripheral cannula insertion and care 4) Prevention of surgical site infection 5) care of the ventilated patient 6) Urinary catheter insertion and care 7) Prevention of C. difficile infection. Areas which consistently fall below 95% are peripheral cannula ongoing care (failure to record presence/absence of signs of infection at insertion site) and care of the ventilated patient (oral hygiene). These are being addressed. Two additional High Impact Interventions are likely to be introduced over the coming year Cleaning and decontamination Antibiotic prescribing Hand hygiene audits Hand hygiene audits now include a component for auditing the “bare below the elbows” component of the uniform policy/dress code. Compliance has risen consistently over the year, with 100% compliance being regularly attained in most areas. Surgical Site Infection Surveillance The Trust has continued to report orthopaedic surgical site infection rates as part of the mandatory reporting mechanism. For the year January-December 2010, infection rates were as follows (figures in parentheses are the quoted UK rate, although it is not clear what time period those figures refer to).: HIP 1.8% (0.8%) KNEE 0.34% (0.6%) HEMIARTHROPLASTY 2.64% (1.7%) The Surgical Directorate has appointed Specialist Nurses to lead on Surgical Site Infection Surveillance in General Surgery. This commenced in Apr 11. Antibiotic Prescribing The trust-wide antibiotic audit programme was able to be implemented in Jan 2010 following the appointment of an audit nurse on secondment as an additional resource. Significant improvements in antimicrobial prescribing were seen over the year but this remains an ongoing challenge due to the frequent changeover of junior medical staff. Reporting of the audit results was a CQUIN requirement in 2010-11. The Antimicrobial Management Group initiated a number of other interventions to support prudent prescribing. These included: Dedicated antimicrobial section on drug chart Abbreviated credit-card sized antibiotic guidelines The requirement to report the audit results has moved from CQUIN into the contract for 2011-12. SECTION 3: RESIDUAL RISK IMPLICATIONS FOR TRUST Identify the key risks to provision of a high quality, safe and effectiveness of the service Health care associated infections are a continued, ongoing risk to the patients cared for within the Trust. Infections are distressing for both patients and their relatives. Infections lead to increased costs and increase length of stay. There is the potential for a fatal outcome. Failure to achieve targets will lead to bad publicity and financial penalties for the Trust An appropriate response to outbreaks, including effective communications, is necessary to mitigate the risk of adverse publicity for the Trust. SECTION 4: Further mitigating actions (controls) for next reporting period Describe further work to be undertaken (with timescales and costs) to address risks While the incidence of Hospital-associated MRSA bacteraemia is low, thorough investigation of any cases (RCA and SUI reporting) is essential. Avoidable MRSA bacteraemia must be considered a “never event” throughout the Trust and support should be given to the Infection Prevention Team and Matrons in their continued efforts to improve practice. The introduction of standardized aseptic non-touch technique (ANTT) represents significant progress, but training, assessment and ongoing training are essential. Efforts need to be targeted at limiting the risk of patients developing C. difficile infection, by prudent antibiotic use, effective cleaning regimes and appropriate isolation and management of patients with diarrhoea. These issues are being actively addressed. The appropriateness of the C. difficile cohort unit should be reviewed as the number of cases has reduced. While the unit was a valuable resource for managing large numbers of cases, consideration needs to be given to alternative approaches to the isolation of these patients. This should minimize the risk of transmission of C. difficile between cases (as there are many different strains), while preserving the expertise which has been developed in the nursing staff caring for patients with Clostridium difficile-associated infection. The overall lack of isolation facilities must be addressed.