Colorectal Cancers
advertisement

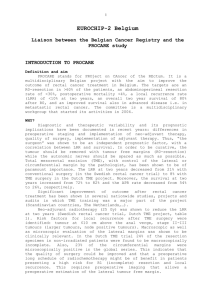
Colorectal Cancers Colorectal cancer (CRC) is a common and lethal disease. Approximately 148,000 new cases of large bowel cancer are diagnosed each year in the United States, of which 106,000 are colon and the remainder rectal cancers. Clinical Manifestations: Abdominal pain — 44 percent Change in bowel habit — 43 percent Hematochezia or melena — 40 percent Weakness — 20 percent Anemia without other gastrointestinal symptoms — 11 percent Weight loss — 6 percent Pronosis worse symptomatic vs asymptomatic (5 year survival 49 vs 71 percent) Metastatic disease: Approximately 15 to 20 percent of patients have distant metastatic disease at the time of presentation. CRCs can spread by lymphatic and hematogenous dissemination, as well as by contiguous and transperitoneal routes. The most common metastatic sites are the regional lymph nodes, liver, lungs, and peritoneum, and patients may present with signs or symptoms referable to any of these areas. The presence of right upper quadrant pain, abdominal distention, early satiety, supraclavicular adenopathy, or periumbilical nodules usually signals advanced disease. Because the venous drainage of the intestinal tract is via the portal system, the first site of hematogenous dissemination is usually liver, followed by lungs, bone, and many other sites, including brain. However, tumors arising in the distal rectum may metastasize initially to the lungs because the inferior rectal vein drains into the inferior vena cava rather than into the portal venous system. Location: For each stage, cancers arising at or below the peritoneal reflection (rectosigmoid and rectum) have a worse five-year survival rate than those arising more proximally. Furthermore, within the rectum, distal cancers have a worse prognosis than more proximal lesions. DDX of a colonic mass includes a number of benign and malignant disorders and generally requires histologic evaluation Adenocarcinoma is most common form of CRC Staging (Clinical and pathological): Polyps that contain an area of invasive malignancy without associated adverse histologic features have a low risk of lymphatic and distant metastases; in such patients, clinical staging is unnecessary, and polypectomy alone may represent appropriate therapy Clinical Staging evaluation: Preoperative clinical staging is best accomplished by physical examination (with particular attention to ascites, hepatomegaly and lymphadenopathy), computed tomography (CT) scan of the abdomen and pelvis, and chest radiograph. The single most common liver test abnormality associated with liver metastases is an elevation in the serum alkaline phosphatase level. In patients with newly diagnosed CRC, preoperative abdominal and pelvic CT scans can demonstrate regional tumor extension, regional lymphatic and distant metastases, and tumor-related complications (eg, obstruction, perforation, fistula formation). Endoscopic ultrasound (EUS) exceeds the capability of CT scan to locally stage the depth of transmural invasion and the presence of perirectal nodal involvement for rectal cancers. The correlation between EUS tumor (T) stage and pathologic T (pT) stage ranges from 70 to 92 percent. PROGNOSIS — Despite the enormous number of correlative studies exploring the prognostic significance of various histologic, molecular, and clinical features, the pathologic stage at diagnosis remains the best indicator of long-term prognosis for both colon and rectal cancer. The most important characteristics are the presence of distant metastases, local tumor extent, nodal positivity (particularly the number of involved lymph nodes), and residual disease. Colon cancer — The estimated five-year survival rates by stage stratified by TNM stage (show table 3) are [65,66]: Stage 0 — 100 percent Stage I: T1 — 97 percent; T2 — 90 percent Stage II: T3 — 78 percent; T4 — 63 percent Stage III: Any T; N1 = 1-3 positive regional lymph nodes; M0 — 66 percent Any T; N2 = 4 or more positive regional nodes; M0 — 37 percent Stage IV: Any M1 = presence of distant metastases — 4 percent Rectal cancer — Five-year survival rates for rectal cancer tend to be somewhat lower, and are heavily dependent upon case mix (show table 5) [36,69]. In particular, the survival of patients with stage III disease is variable, and depends upon the T stage (ie, T1-2 versus 3-4) and the extent of nodal disease. As an example, when data from the National Cancer Database were stratified according to subsets of stage III disease, the following five-year survival rates were reported [67]: Stage IIIA (T1-2, N1) — 55.1 percent (n = 1043 patients) Stage IIIB (T3-4, N1) — 35.5 percent (n = 2856 patients) Stage IIIC (Any T, N2) — 24.5 percent (n = 2089 patients) Treatment: Surgery Abdominal perineal resection (APR) — An APR, which requires incisions in both the abdomen and perineum, entails removal of the primary tumor along with a complete proctectomy. This results in the need for a permanent colostomy. Sphincter-sparing procedures — Sphincter-sparing approaches for distal rectal cancers have evolved along two pathways: For patients with small rectal cancers that are confined to the rectal wall, local excision techniques may offer local control and survival rates that are comparable to APR, while preserving sphincter function. For patients with larger or more invasive tumors of the distal rectum (eg, T3 or T4 lesions), preoperative or neoadjuvant chemoradiotherapy may facilitate the conversion of a planned APR to a sphincter-sparing LAR by promoting tumor regression. This topic is discussed elsewhere. Low anterior resection — Most invasive rectal cancers involving the upper third of the rectum can be adequately treated by an LAR with preservation of the anal sphincter. Local excision — Early distal rectal cancers with favorable features that are classified as T1 or T2 by depth of invasion may be treated by local excision through the anus (transanal excision), by division of the anal sphincter (transsphincteric or York-Mason procedure), or through a posterior parasacral approach (Kraske resection).