POSTOPERATIVE DELIRIUM IN ADULTS IN THE PACU
advertisement
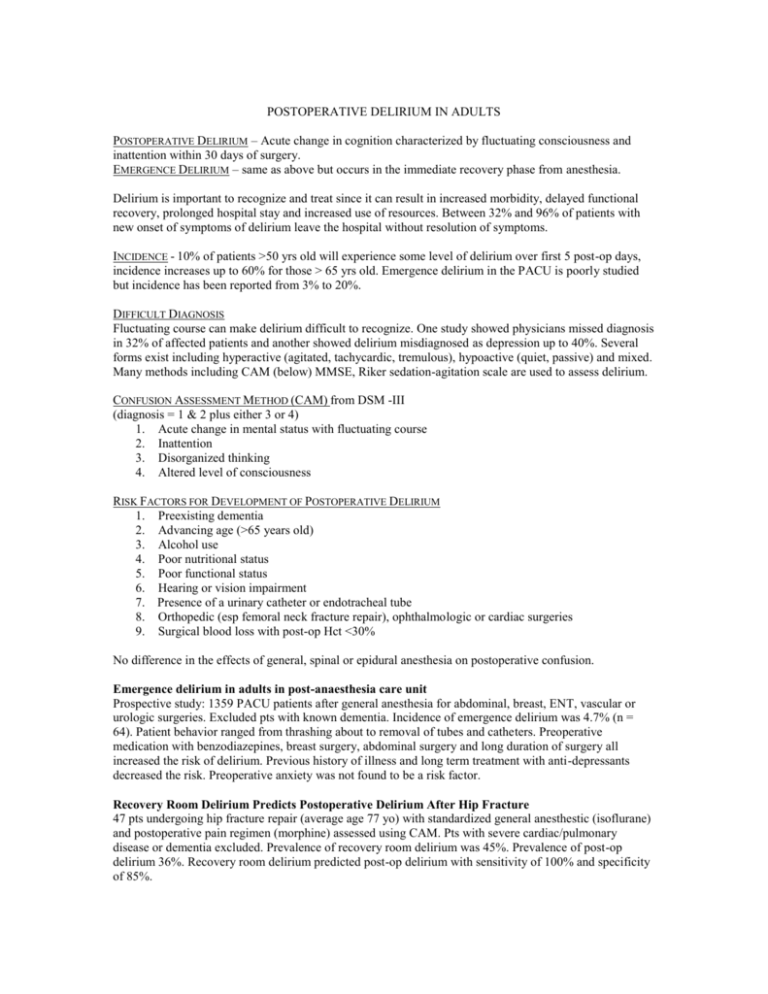
POSTOPERATIVE DELIRIUM IN ADULTS POSTOPERATIVE DELIRIUM – Acute change in cognition characterized by fluctuating consciousness and inattention within 30 days of surgery. EMERGENCE DELIRIUM – same as above but occurs in the immediate recovery phase from anesthesia. Delirium is important to recognize and treat since it can result in increased morbidity, delayed functional recovery, prolonged hospital stay and increased use of resources. Between 32% and 96% of patients with new onset of symptoms of delirium leave the hospital without resolution of symptoms. INCIDENCE - 10% of patients >50 yrs old will experience some level of delirium over first 5 post-op days, incidence increases up to 60% for those > 65 yrs old. Emergence delirium in the PACU is poorly studied but incidence has been reported from 3% to 20%. DIFFICULT DIAGNOSIS Fluctuating course can make delirium difficult to recognize. One study showed physicians missed diagnosis in 32% of affected patients and another showed delirium misdiagnosed as depression up to 40%. Several forms exist including hyperactive (agitated, tachycardic, tremulous), hypoactive (quiet, passive) and mixed. Many methods including CAM (below) MMSE, Riker sedation-agitation scale are used to assess delirium. CONFUSION ASSESSMENT METHOD (CAM) from DSM -III (diagnosis = 1 & 2 plus either 3 or 4) 1. Acute change in mental status with fluctuating course 2. Inattention 3. Disorganized thinking 4. Altered level of consciousness RISK FACTORS FOR DEVELOPMENT OF POSTOPERATIVE DELIRIUM 1. Preexisting dementia 2. Advancing age (>65 years old) 3. Alcohol use 4. Poor nutritional status 5. Poor functional status 6. Hearing or vision impairment 7. Presence of a urinary catheter or endotracheal tube 8. Orthopedic (esp femoral neck fracture repair), ophthalmologic or cardiac surgeries 9. Surgical blood loss with post-op Hct <30% No difference in the effects of general, spinal or epidural anesthesia on postoperative confusion. Emergence delirium in adults in post-anaesthesia care unit Prospective study: 1359 PACU patients after general anesthesia for abdominal, breast, ENT, vascular or urologic surgeries. Excluded pts with known dementia. Incidence of emergence delirium was 4.7% (n = 64). Patient behavior ranged from thrashing about to removal of tubes and catheters. Preoperative medication with benzodiazepines, breast surgery, abdominal surgery and long duration of surgery all increased the risk of delirium. Previous history of illness and long term treatment with anti-depressants decreased the risk. Preoperative anxiety was not found to be a risk factor. Recovery Room Delirium Predicts Postoperative Delirium After Hip Fracture 47 pts undergoing hip fracture repair (average age 77 yo) with standardized general anesthestic (isoflurane) and postoperative pain regimen (morphine) assessed using CAM. Pts with severe cardiac/pulmonary disease or dementia excluded. Prevalence of recovery room delirium was 45%. Prevalence of post-op delirium 36%. Recovery room delirium predicted post-op delirium with sensitivity of 100% and specificity of 85%. DIFFERENTIAL DIAGNOSIS OF POSTOPERATIVE DELIRIUM IN PACU Arterial hypoxemia Preexisting cognitive disorder (Dementia, Parkinson’s) Hypoventilation with hypercapnia Metabolic derangements (renal, hepatic, endocrine) Drugs (Anticholinergics, benzodiazepines, opioids, B-blockers) Drug or ETOH withdrawal Electrolyte abnormalities Incomplete muscle relaxant reversal Seizures Acute CNS event (stroke) Infection PATHOPHYSIOLOGY Poorly understood. Some hypotheses: When oxidative metabolism of the brain decreases neurotransmitter levels decline and cause mental dysfunction. Specific neurotransmitter acetylcholine is crucial as it plays a role in awareness and arousal. Elderly patients are relatively deficient in acetylcholine and are therefore more sensitive to anticholinergic drugs. Increase in serum cortisol from stress of surgery possibly responsible for postoperative confusion. Hypocapnia which occurs intraoperatively can decrease cerebral blood flow via vasoconstriction. Disturbance of sleep-wake cycle or sleep deprival TREATMENTS & INTERVENTIONS First consideration is to always treat any underlying organic cause. Have caregiver or family member come to bedside to help orient the patient. Make recovery room cheerful & well lit to promote awareness and alertness. Remind patient of situation. Provide patients with eyeglasses and hearing aids as soon as possible. Treat pain! One study showed higher pain scores at rest increased risk of delirium over first 3 post-op days. Be conservative with opioids in elderly as they can also contribute to CNS depression and confusion. If sedation required can use benzodiazepines (versed or ativan) 0.5 to 1mg IV. Avoid antihistamines (Benadryl) especially in elderly as they can cause paradoxical agitation and worsen confusion via anticholinergic activity. Avoid physical restraints if possible as they may aggravate the confusion. If necessary for patient safety, reasons for the restraints should be explained frequently to the patient. Haldol can be given if having hallucinations or severe agitation. Can give 0.5mg IV at a time. Less cardiovascular and anticholinergic effects than other antipsychotic medications. Physostigmine, a cholinesterase inhibitor that passes the blood brain barrier to counteract CNS anticholinergic activity which is often present after atropine or scopolamine or even Demerol administration. Dose 1-2mg IV. Watch for bradycardia and increased secretions. Melatonin to assist with sleep-wake cycle, can be given preoperatively for prevention and postoperatively for treatment References: 1. Demure M, Fain, M. The Elderly Surgical Patient and Postoperative Delirium. J Am Coll Surgeons Nov 2006; (203) 752-757 2. Paarikh S, Chung F. Postoperative Delirium in the Elderly. Anesthesia & Analgesia 1995; (80) 1223-32 3. Hanania M, Kitain, E. Melatonin for treatment and prevention of postoperative delirium. Anesthesia & Analgesia 2002; (94) 338-9 4. Lepouse C, Lautner C, et al. Emergence delirium in adults in post-anaesthesia care unit. British Journal Anaesthesia May 2, 2006; (96) 747-53 5. Sharma P, Sieber F, et al. Recovery Room Delirium Predicts Postoperative Delirium After Hip Fracture Anesthesia & Analgesia 2005; (101) 1215-20