Pediatric Surgery (Pg 68-81)
advertisement
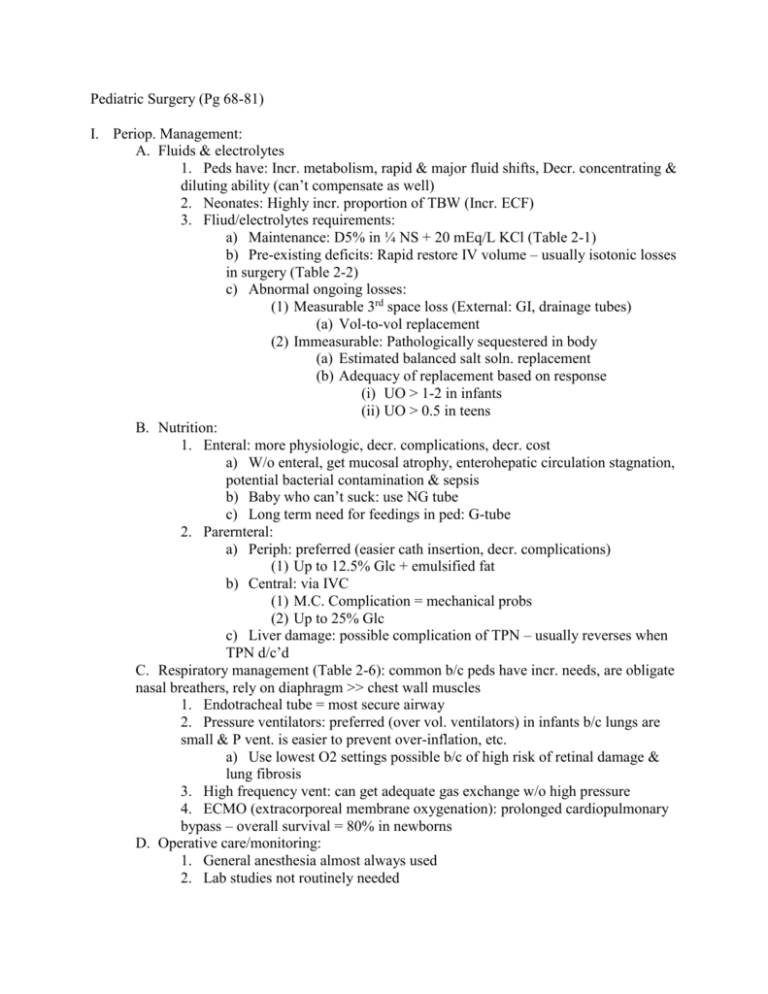
Pediatric Surgery (Pg 68-81) I. Periop. Management: A. Fluids & electrolytes 1. Peds have: Incr. metabolism, rapid & major fluid shifts, Decr. concentrating & diluting ability (can’t compensate as well) 2. Neonates: Highly incr. proportion of TBW (Incr. ECF) 3. Fliud/electrolytes requirements: a) Maintenance: D5% in ¼ NS + 20 mEq/L KCl (Table 2-1) b) Pre-existing deficits: Rapid restore IV volume – usually isotonic losses in surgery (Table 2-2) c) Abnormal ongoing losses: (1) Measurable 3rd space loss (External: GI, drainage tubes) (a) Vol-to-vol replacement (2) Immeasurable: Pathologically sequestered in body (a) Estimated balanced salt soln. replacement (b) Adequacy of replacement based on response (i) UO > 1-2 in infants (ii) UO > 0.5 in teens B. Nutrition: 1. Enteral: more physiologic, decr. complications, decr. cost a) W/o enteral, get mucosal atrophy, enterohepatic circulation stagnation, potential bacterial contamination & sepsis b) Baby who can’t suck: use NG tube c) Long term need for feedings in ped: G-tube 2. Parernteral: a) Periph: preferred (easier cath insertion, decr. complications) (1) Up to 12.5% Glc + emulsified fat b) Central: via IVC (1) M.C. Complication = mechanical probs (2) Up to 25% Glc c) Liver damage: possible complication of TPN – usually reverses when TPN d/c’d C. Respiratory management (Table 2-6): common b/c peds have incr. needs, are obligate nasal breathers, rely on diaphragm >> chest wall muscles 1. Endotracheal tube = most secure airway 2. Pressure ventilators: preferred (over vol. ventilators) in infants b/c lungs are small & P vent. is easier to prevent over-inflation, etc. a) Use lowest O2 settings possible b/c of high risk of retinal damage & lung fibrosis 3. High frequency vent: can get adequate gas exchange w/o high pressure 4. ECMO (extracorporeal membrane oxygenation): prolonged cardiopulmonary bypass – overall survival = 80% in newborns D. Operative care/monitoring: 1. General anesthesia almost always used 2. Lab studies not routinely needed 3. Pre-op intake: Older kids - no food or milk 8hrs & NPO hrs, Infants – 6 & 4 hrs, respectively 4. Intraoperative: a) Monitor O2 sat - if below 95%, needs immediate investigation b) If indwelling cath needed (BP instability), umbilical artery is safe easy access (Central venous caths not often used) c) Must prevent hypothermia in peds 5. Outpatient: starting at 3 mo for term babies & 52 wks if premature E. Emotional support & Pain management: 1. Face-mask anesthesia induction in little kids 2. Post-op: a) Long-acting local n. block during surgery helps for hours afterward & epidural cath can be left in place several days b) Avoid IM (administration hurts) c) Careful w/ narcotics b/c of apnea (patient-controlled dosing in kids over 5 actually works best) d) NSAIDs can be also used II. Neonatal surgical conditions - Birth defects = MMC of perinatal mortality in US A. Congenital diaphragmatic hernia – prototype of surgical cause of resp distress 1. Types: a) Bockdalek: defect of posterolateral diaphragm – most common b) Morgagni: retrosternal – not often emergencies 2. Embryology: pleuroperitoneal canal stays open, viscera pass thru, pulmonary hyperplasia 3. Pathophys: compression of lung by herniated viscera, pulmonary hyperplasia, pulmonary hypertension (can cause R to L shunting) 4. Presentation: dypnea & cyanosis, decr. breath sounds on side of herniation; confirmed by CXR 5. Tx: Resuscitate first then sgx: supplemental O2 & ET intubation w/ mech vent & place NG tube a) Pos P vent thru face mask is CI b) Sgx: Viscera reduced, diaphragm closed, ECMO used in peds who don’t respond well to vent support 6. Px: Mortality = 50% B. Neonatal thoracic mass lesions: congenital lobar emphysema, cystic adenomatoid malformation, pulmonary sequestration, foregut duplication cysts 1. Can be Sx or a-Sx; Seen on CXR 2. Tx: Surgical excision if possible 3. Good Px except cystic adenomatoid malformation w/ hydrops C. Esophageal atresia & Tracheoesophageal fistula - Usually occur in combo: 1. EA=interruption in continuity of upper & lower parts of esoph. 2. TEF=abnormal communication btw esophagus & trachea 3. Most common combo= upper esoph ends blindly & lower portion communicates w/ trachea (type C) 4. Pathophys: Often have “VACTER association” abnormalities a) Vertebral, Anal, Cardiac, Tracheal, Esophageal, Radial or Renal b) Presentation: (1) EA: immediate chocking & regurg w/ feeding, excess drooling, can’t pass NG tube, Air in abd if w/ TEF (not if isolated EA) (2) TEF (isolated): “H” type worst (get aspiration pneumonia), Dx w/ endoscopy or contrast swallow c) Tx (good Px): Elevate head, double-lumen tube in upper pouch to suction, primary repair if possible, staged repair + gastrotomy if needed D. Congenital GI obstruction – anywhere from stomach to anus (Tables 2-8, 2-9) 1. Presentation: Varies according to site of obstruction 2. Key signs: Polyhydramnios, Bilious vomiting, Abd distension, &Failure to pass meconium 3. Dx w/ Plain x-rays: a) Complete Prox: Few dilated bowel loops, air fluid levels, no distal air b) Partial prox: do upper GI contrast study c) Distal: many distended bowel loops, do contrast enema to verify 4. Tx: Always includes NG tube, IV hydration, prophylactic Abc’s a) Duodenal: Commonly causes by atresia & malrotation (1) Atresia often assoc. w/ Down’s syndrome or anular pancreas (2) Malrotation w/ Midgut volvulus most common in first month of life = most dangerous form of intestinal obstruction (3) Malrotation w/ Ladd’s bands: peritoneal attachments to lateral wall cross over duodenum (4) Get “Double Bubble” on x-ray (5) Tx: immediate sgx unless midgut atresia is r/o b) Small intestine: due to atresia, meconium ileus, intestinal duplication (1) X-rays: foamy appearing dilated meconium-filled bowel loops & no fluid air levels; calcification on abd x-ray = antenatal perf (2) Duplications = endothelial-lined cystic/tubular structures adjacent to alimentary tract on mesenteric side of nl bowel (3) Tx: Atresia & duplications - resection & primary anastamosis Meconium ileus – often nonoperative tx w/ Gastrographin (diatrizoate) enemas (radiopaque fluid)… if persists or if perf present, need sgx c) Colon: Hirschprung’s, meconium plug, neonatal small L colon syndrome, atresia (rare) (1) W/ Hirschprung’s rectosigmoid colon is most common site for boundry btw aganglionic colon & dilated nl colon; can present immediately or later in childhood (2) Dx w/ contrast enema, anorectal manometry, & rectal bx (3) Tx is usually staged: Temporary colostomy, then pull-trhough to anastomose proximal (ganglionic) bowel w/ anal canal (4) Probs: severe entercolitis w/ dehydration, peritonitis, & sepsis (5) Meconium plug (in premature babies) & small L colon syndrome (baby of DM moms) – contrast enema both Dx & Tx Pediatric Surgery p. 81-91 I. Anorectal Malformations - - - - - aka imperforate anus; rectum does not reach its normal perineal termination high malformation – rectum ends above levator muscles o rectum may end blindly, but usually terminates in anterior fistulous tract o Boys – fistula to urethra or bladder o Girls – fistula to vagina low malformation – rectum passes through levator muscles but does not terminate at external sphincter o fistula drains externally, but anterior to normal anal site o boys – small opening in ant. Perineum or forward to scrotal raphe o girls – small opening in ant. Perineum or posterior vulva behind hymen cloaca – rare, occurs in girls; single opening for rectum, vagina, and urethra diagnosis o if low lesion, can usu. see external fistula o if no external fistula, assume high lesion; may see stool from vagina or urethra in high lesion o if high or low is unclear, may do “invertogram” by holding baby upside down and performing lateral x-ray. If air is seen within 1 cm of perineal skin, probably low lesion. treatment o continence depends on: external sphincter, internal sphincter, and levator muscles (most important) o low lesion – if fisula is only slightly anterior, may not need modification if too anterior to function, surgery – perineal anoplasty o intermediate or high lesion – needs initial colostomy. Then, pull-through procedure in next few months where rectum is pulled through levator swing and anastamosed to perineum. Most common operation: Pena operation. prognosis o low – excellent prognosis o high – difficult to toilet train, may have occasional soiling, may need daily enemas II. Neonatal Jaundice: Biliary Atresia and Choledochal Cyst normal neonatal jaundice is usu. self-limited; indirect hyperbilirubinemia beware of direct bilirubin >2mg/dL for 2 weeks neonatal cholestatic jaundice: biliary atresia, choledochal cysts, screen for TORCH infections, antitrypsin def., galactosemia, and TPN or hypoxic injury to liver Biliary atresia, neonatal hepatitis, and infantile choledochal cysts may be manifestations of the same disease, but the etiology is unknown percutaneous liver biopsy may also be helpful in dx biliary atresia – progressive inflammatory obliteration of the bile ducts, beginning around the time of birth presentation: progressive jaundice, pale stools, enlarged liver, elevated conj. Bilirubin, alk phos, and other liver enzymes may do hepatic scintiscan after pretreatment with Phenobarbital to exclude biliary atresia if radionuclide shows up in intestine (shows bile duct patency) treatment: laparotomy to inspect hilum of liver; if intraoperative cholangiogram shows patent bile ducts then dx is probably neonatal hepatitis Kasai portoenterostomy – drain hepatic ductules at porta hepatis to halt disease process; cut across tissue and anastamose to intestinal tract before child is 8 wks old. 30% do well after this operation. Rest are candidates for liver transplant. Prognosis: depends on diameter of hepatic ductules and absence of hepatic fibrosis. Recurrent postop cholangitis is common, give long-term abx prophylactically. Portal hypertension with esophageal varices is also common. choledochal cysts – dilation of the common bile duct with distal obstruction presentation: presents similarly to biliary atresia identify with US treatment: excise and reconstruct biliary system by anastamosing defunctionalized bowel loop to proximal hepatic ducts prognosis: excellent Abdominal Wall Defects: Omphalocele and Gastroschisis omphalocele and gastroschisis are congenital defects of the abdominal wall through which the abdominal contents protrude externally to a varying degree embryology: four folds form abdominal wall: cephalic, caudal, and two lateral folds converge to form a large umbilical ring surrounding umb. Cord and yolk sac. Between weeks 5-10, intestine is extruded out of the umbilical ring and into the yolk sac. It then returns to abdominal cavity, where it undergoes rotation. Pathophysiology: omphalocele results when lateral folds do not close, extruded viscera remain in yolk sac; omphaloceles are always covered by a translucent membrane gastroschisis probably results from an in utero perforation of developing abdominal wall at pt where one of the paired umbilical veins undergoes atrophy (pt of weakness) Clinical presentation: Omphalocele – opening in abd. wall with protruding viscera covered by a translucent membrane. High rate of associated congenital anomalies. Gastroschisis – opening in abd. is lateral to umbilical cord, usu. to the R. Viscera are not covered by a membrane and may be inflamed and edematous. May have intestinal atresia caused by in utero compression and vascular compromise. Treatment: High risk for fluid and heat loss from exposed viscera – keep viscera moist with saline, wrap abdomen with plastic, IV fluids, broad spectrum abx, and NG decompression Gastroschisis – keep viscera on top of or beside baby to avoid kinking of vascular supply to bowel. Emergency surgery is required to replace viscera in abdomen and close defect. If abdominal cavity is too small to allow primary closure, place “silo” over defect and manually compress daily to reduce viscera and expand abdominal cavity. Omphalocele – Surgery is not emergent. Evaluated associated anomalies. Sac eventually epithelializes and contracts leaving a ventral hernia that can be repaired electively. Prognosis Gastroschisis – may have prolonged intestinal dysfunction after surgery as result of chronic inflammation of exposed bowel. Long-term outlook is good. Omphalocele – prognosis is related to associated anomalies that may be present Circumcision - among oldest of surgical procedures - most frequently performed operation on males in US - percent circumcised: 90% boys in US, 40% of boys in Canada, 15% in Australia, and very rarely in Europe - controversial, even within medical profession - American Academy of Pediatrics remains neutral, stating that risks and benefits should be given to parents and parents should decide - undersurface of foreskin is fused with glans at birth so in uncircumcised boys, attempts at retration of foreskin should be avoided until 2 to 3 years of age - advantages: prevents phimosis, prevents paraphimosis, lowers incidence of UTIs in infancy, prevents balanopsthisis (infection of glans and foreskin from retained secretions), prevents cancer of the penis - disadvantages: medically unnecessary in most boys, painful, risk of complications (low, but may include bleeding, infection, meatal ulcers, postcircumcision phimosis, necrosis) - contraindictions: anomalies of the external genitalia (hypospadias) because foreskin may be needed for operative correction, serious illness Surgical Conditions in the Older Child Inguinal Hernia and Hydrocele Repair of both inguinal hernias and hydroceles is most common operation performed by pediatric surgeons Hernias occur in 3% of children overall, with an incidence of 30% in very premature infants Increased intrabdominal tissue (ascites) and connective tissue disorders may predispose to hernias Boys are affected 6 x as often as girls Inguinal hernias in children are almost all indirect hernias, with hernia sac coming through internal inguinal ring Embryology: at 3 months gestation, processus vaginalis forms and passes through internal inguinal ring, then migrates down inguinal canal to scrotum, and lies in spermatic cord Processus is usually obliterated around time of birth In girls: tunica vaginalis Pathophysiology: continued patency of all or part of the processus vaginalis accounts for the development of hernias and hyrdoceles If processus is open and still continuous with peritoneal cavity, intraabdominal contents may protrude through and become inguinal hernia If processus is open but is too narrow for viscera to pass through, only peritoneal fluid may enter and form communicating hydrocele that communicates with peritoneal cavity If distal processus is obliterated, fluid accumulates above the testicle as a hydrocele of the spermatic cord If the proximal processus is obliterated, fluid may be trapped distally in the tunica vaginalis and produce a noncommunicating hydrocele Presentation and evaluation: About half of all inguinal hernias appear during the first year of life. Inguinal hernias appear twice as often on the right side because the R testicle descends later embryologically and its processus is less likely to have closed Ten percent of inguinal hernias are bilateral Examination: hernia - palpable as a firm mass that completely disappears with digital pressure. If not obvious, may be brought out by asking older children to jump or strain. Hydrocele - swelling of hemiscrotum, not reducible, does not extend upward to inguinal ring. Hydrocele of cord may resemble incarcerated hernia, but incarcerated hernias are very painful and may cause intestinal obstruction. Treatment: Inguinal hernias never resolve in children – should be repaired by high ligation of hernia sac at internal ring Incarcerated hernia is emergency because of strangulation of hernial contents and the possibility of testicle ischemia. Apply slow persistent pressure bimanually on mass and delay repair for 24 -48 hours to allow scrotal edema to subside. Child with inguinal hernia is at increased risk of having another one on contralateral side Umbilical Hernia caused by failure of umbilical ring to contract completely esp. common in African Americans, incidence is 50% most resolve spontaneously during childhood with very low risk of incarceration Presentation and evaluation: see bulge within umbilicus, palpate fascial defect when mass is reduced Treatment: surgery when hernia persists beyond 4 years of age Surgery if fascial defect is >1.5 cm when child is 2 years old Correct in pregnant girls because of increased risk with increased abdominal pressure Cryptorchidism Cryptorchid testes – testis has not descended into scrotum. Usually occurs 7-9 months gestation. Incidence – 3% term infants, 30% preterm Most cryptorchid testes spontaneously descend within 1 year 10-40 x increase in testicular malignancy with undescended testes, orchidopexy (surgical descent of testical) does not decrease malignancy rates, but increases rate of detection increased risk of testicular torsion, more vulnerable to trauma, and psychological concerns usually associated with patent processus vaginalis, so also predisposed to inguinal hernias undescended testes may be palpable in abdomen. Distinguish from retractile testis where testes is transiently pulled up by cremasteric muscle. Important to find undescended testicle. May be totally absent or may be above internal ring. Laparoscopy is best way to look for it. If bilateral nonpalpable testes, check HCG to see if serum testosterone rises. If it does not, no testicular tissue exists. New treatment: HCG or leutenizing hormone-releasing hormone as initial treatment, still controversial and more likely to work with bilateral cryptorchidism Most common treatment: orchidopexy during second year of life with closure of patent processus vaginalis. Place testicle in dartos muscle pouch. Atrophic testes or found in late puberty – orchiectomy, laparoscopic or open Prognosis: after orchidopexy, 80-90% of boys with unilateral cryptorchidism are fertile; 50% with bilateral cryptorchidism are fertile Testosterone and secondary sex characteristics are unaffected Pyloric Stenosis: Progressive hypertrophy of the musculature of the pylorus of infants, eventually leading to gastric outlet obstruction Common disorder. 1:500 infants. M:F = 4:1. Strong familial component. Etiology unknown. Hypotheses include: 1.) abnormal development of ganglion cells in the wall of the pylorus 2.) milk curds propelled against the pylorus submucosal edema blocks gastric outlet subsequent work hypertrophy of muscular pylorus. Presentation: Symptoms begin b/t 2-8 wks with nonbillious vomiting after feeding. Vomiting maybe projectile, and becomes progressively worse until food isn’t tolerated. Infant remains hungry and sucks vigorously. Stool frequency and urinary output is significantly decreased. Exam: Infant is irritable and dehydrated. Peristaltic waves seen moving across abdomen. Hallmark is palpable “olive”, a hard, round, movable mass in epigastrium. Pyloric mass maybe more palpable following empting of stomach with NG tube. When olive is identified, no imaging studies are necessary (i.e. palpable olive is pathognomonic for pyloric stenosis). If no olive is found U/S is highly accurate in diagnosing P.S. Length, diameter, and wall thickness all increased. Barium swallow can be utilized if U/S neg. and still have clinical suspicion. It will show a narrowed, elongated pyloric channel. Treatment: 1. Preoperative rehydration is essential. Infants are likely to have hypochloremic hypokalemic metabolic alkalosis (d/t vomiting). 2. Pyloromyotomy – operative longitudinal split of hypertrophic pyloric muscle that extends down to mucosa, but doesn’t enter it. 3. Feeding initiated 6 to 12 hrs postop and gradually incrased. Acute Abdomen: Children present a challenge to physicians b/c of the following factors: 1. Children tend to have a uniform reaction to infection. Whether they have strep pharyngitis, pneumonia, appendicitis, etc. they often have fever, vomiting and a “stomachache” 2. Surgical diseases in children are age dependent. Relative risks vary greatly with age. 3. Children have limited ability to express their symptoms. 4. Children in pain are not cooperative; examination is difficult. 5. Parental anxiety adds to the stress of the situation. Appendicitis: Most common condition requiring emergent surgery in childhood. Rare in infants, incidence increases thereafter and peaks in adolescents and young adults. Caused by obstruction of the appendix base by fecalith or lymphoid hyperplasia. Mucosal secretions expand the appendix increased intraluminal pressure bacterial overgrowth impairment of perfusion perforation within 24-48 hrs Delayed recognition more likely in children. Those under 5 usually have perforation by the time of presentation. Pain in periumbilical area migrating to RLQ, but this classic presentation may not always be present. Anorexia, N/V common. Temp is usually nl or slightly high. Early high fever suggests other diagnosis. Later, high fever indicates perforation. Cheeks often flushed, child unusually quiet, knees pulled up. Decreased bowel sounds w/ involuntary guarding, tenderness, and rebound in RLQ. Patients with perforation: often septic, abd distension d/t ileus, peritonitis, RLQ or rectal mass. Labs: Leukocytosis w/ left shift, few WBC/RBC present in urine consistent with inflamed appendix in congruity with the urinary tract. Β-HCG levels should always be checked in adolescent girls to exclude ectopic pregnancy. Only pathognomic sign of appendicitis is calcified fecalith that can be visualized on abdominal xray in 5 – 15% of patients. Ruptured appendix may lead to SBO and is the most common cause of obstruction in school-aged children. U/S is 90% accurate in making the diagnosis. Especially useful to rule-out ovarian cyst, adnexal torsion, and PID in girls. Differential diagnosis: Table 2-13. Tx: Urgent appendectomy after rapid IVF hydration and administration of broadspectrum antibiotics. Postop antibiotics unnecessary if perforation not present. If perforation present, antibiotics continued for at least 3 days and d/c when patient is afebrile for 48 hrs w/ nl white count. Complications: Intra-abdominal abscesses and wound infection. Abscesses drained percutaneously or transrectally via US guidance. Wound infections are opened and drained. Intussesception: Telescoping of one portion of the intestine into another. Usually ileocolic. Emergency condition, involved intestine can become strangulated. Typically affects children 6-18 months. Viral hypertrophy of Peyer’s patches most common cause. Less often causes: pathologic lead point (e.g. Meckel’s diverticulum, polyp, lymphoma, hematoma) Often follows viral illness. Presentation: intermittent bouts of colicky abdominal pain, causing child to cry and pull knees in towards chest. Between episodes child is initially well but becomes increasingly lethargic. Vomiting is common and eventually becomes bilious. Blood and mucus passed rectally as “currant jelly” stools d/t congestion and ischemia of intestinal mucosa. Examination: Irritable and somnolent, dehydrated, tender sausage shaped mass often palpable in RUQ. Digital rectal exam often yields blood and mucous. Abdominal xrays are normal or show paucity of air in RLQ, eventually showing dilated small intestinal loops consistent with obstruction. Diagnosis: Barium or air-contrast enema. Ileocolic intussusception appears as a filling defect in the colon, at which flow of contrast stops. U/S can also be diagnostic. Ileoileal intussusceptions are rare and are usually associated with a lead point of previous operation. Treatment: Pressure of barium or air is used to reduce intussusception and is successful in most cases. Also saline enema under US guidance can be used. Surgery is performed promptly if nonoperative reduction fails, which includes manual reduction and appendectomy. If intestine is necrotic or pathologic lead point is identified, that section of intestine is resected. Recurrent intussusception occurs in 5 -8% of children, regardless of method of reduction. Meckel’s Diverticulum Occurs in 2% of population Located in ileum, within 100 cm of the ileocecal valve. Contains heterotopic tissue in 50% of symptomatic patients. Most often lined with gastric mucosa. Embryologic remnant of vitelline duct, which communicates the intestine with the yolk sac. Most remain asymptomatic, but some may be complicated by bleeding, obstruction and inflammation. Bleeding results from ulceration adjacent to ectopic gastric mucosa of the diverticulum. Usually occurs in children younger than age 5. The blood is usually dark red, painless, and can be massive. Technetium pertechnetate scans show increased uptake in gastric tissue in 50% of cases. Can cause intestinal obstruction by acting as the lead point of an intussusception or by allowing the intestine to twist around it causing volvus. Meckel’s Diverticulitis occurs in older children and is almost always misdiagnosed preop b/c manifestations similar to those of appendicitis. Whenever nl appendix is found on laparotomy for presumptive appendicitis, distal ileum must be inspected for the possibility of Meckel’s diverticulitis. Tx: resected by laparotomy or laproscopic surgery. Asymptomatic diverticuli found incidentally at surgery are resected if: the child is young, diverticuli has narrow neck, ectopic tissue is palpable within lumen, or it is attached to abdominal wall. Gastrointestinal Bleeding: Most likely source of bleeding in a child may be suspected by the patient’s age, level of bleeding, the color and amount of blood, and associated findings. Common causes of GI bleeding according to age: Table 2-14. Gastroesophageal Reflux: Reflux of stomach contents into esophagus. Common in infants and children who have neurological impairments due to motor and reflex abnormalities of foregut, including: disordered swallowing, decreased esophageal clearance, an incompetent LES and delayed gastric emptying. Common in normal babies because lower esophageal sphincter is relatively incompetent for first few months of life. This is usually self-limiting: incidence and severity decreases with growth. In children with GERD, vomiting is more severe and may even mimic pyloric stenosis. Clinically significant complications of GERD: 1. failure to thrive (due to chronic regurgitation) 2. aspiration of gastric contents into airway recurrent pneumonia 3. apnea, probably because of reflux-induced laryngospasm or a vagal reflex (possible cause of SIDS ?) 4. peptic esophagitis which can lead to GI bleeding, stricture formation, or Barrett’s esophagus Diagnosis: So common that it is often diagnosed clinically. Barium swallow can be used to rule out obstructive lesions. Other tests include: pH probe study, nuclear scintiscan of the esophagus and endoscopy. Treatment: Medical management most common: upright positioning, thickening of feeds, agents to promote gastric emptying (metoclopramide) and H2 blockers to treat esophagitis. Surgery is indicated if medical management fails. Nissen fundoplication, in which the gastric fundus is wrapped around the esophagus 360 degrees. Complications include: inability to vomit and gas bloat syndrome (patients unable to burp, so they become distended following feeding. Recurrence more common in children that are neurologically impaired. Midline Neck Masses: Table 2-15 Thyroglossal duct cysts Thyroid gland descends from tongue base embryologically. Failure of thyroglossal duct to obliterate leads to thyroglossal duct cysts. Appear between 2-10 yrs of age. Presents as firm, round, midline neck mass that rises with swallowing or tongue protrusion. Infection of cyst is common. Must be removed with its tract and the center of the hyoid bone, or most will recur. Ectopic Thyroid Gland is arrested in its antenatal descent. Presents as midline neck mass and is the patient’s only thyroid tissue. May be divided and moved bilaterally or excised. Patient then receives thyroid replacement therapy. Dermoid or Epidermoid Cyst Arise from trapped epithelial elements. More superficial than thyroglossal duct cyst. Lymphadenopathy in midline may also appeal Thyroid Masses Uncommon in children. Thyroid nodule in children more likely to be malignant. Either lobectomy with biopsy or needle aspiration biopsy and an attempt at suppression with thyroid hormone is recommended. Lateral Neck Masses Acute Cervical Lympadenitis Predominantly occurs in young children following URI with staph or strep Child is febrile and swellings showing signs of inflammation including erythema and tenderness. Antibiotics may be curative. If mass is fluctuant because of abscess, I&D necessary. Chronic Lymphadenopathy Common in cervical region, often representing benign hyperplasia Other causes include: infections with mycobacteria, cat-scratch fever, and rarely lymphoma. Lymphoma is more likely if nodes are hard or fixed, continue to grow, and if patient has systemic symptoms of fever, malaise, and weighty loss. Open biopsy indicated if nodes larger than 2cm and persist for >6wks, or sooner if malignancy is suspected. Cystic Hygromas (lymphangiomas) Congenital malformations of the lymphatic vessels characterized by multi-loculated cysts filled with lymph May occur anywhere, most common in the posterior triangle of the neck followed by the axilla Maybe be present at birth, but almost always presents by age 2. They are usually a soft, compressible mass with ill defined borders. They may become infected; rarely regress. Resection is indicated, although there are recent reports of eradication of complex hygromas by injection of sclerosing agents. Branchial cleft cysts and sinuses: Various brachial clefts and arches that do not completely resorb. In childhood, sinuses are small cutaneous openings that often drain clear fluid. In older children, cysts are usually noted as subcutaneous masses. Remnants of the second branchial cleft are the most common and are located along the anterior border of the SCM. Remnants of the first branchial cleft are found near the ear or the angle of the mandible. Resection is indicated. Neonatal Torticollis (aka Wry Neck) Caused by fibrosis and shortening of the SCM. Traumatic etiology is hypothesized, with hematoma formation and organization within the muscle. The infant has a firm neck mass. The face is rotated away from the affected side and the head is tilted toward the ipsilateral shoulder. U/S confirms that the mass is within the muscle. Passive rotation exercises by the parents are usually curative. Surgical division of the SCM is reserved for rare treatment failures. Untreated, torticollis may lead to permanent facial asymmetry. Pediatric Surgery (99-107) Vascular Tumors Hemangiomas Biologically active benign vascular tumor are characterized initially by cellular proliferation, and followed in most cases by involution. Appear first few weeks after birth, commonly located on the head and neck, may be superficial or deep and may involve the viscera. Superficial lesions, aka capillary hemangiomas are firm, bright red and raised. Deep or cavernous, lesions are softer and may have blue discoloration, less likely to resolve. Most should be left alone. Indications for treatment include significant facial distortion, interference with fxn, thrombocytopenia from platelet trapping, and CHF. Management includes steroids, cyclophosphamides, a-interferon, embolization, and surgical excision. Vascular Malformations Biologically inert errors of morphogenesis of vessels. They are not proliferative and only grow with the child. Remain stable over time. Port wine stain, is seen at birth as a red or purple non-raised lesion, usually on the face. Arteriovenous fistula is another example of a malformation. Common on the extremities and the CNS. In the extremities they are usually multiple and may cause heart failure and hypertrophy of the affected limb. Port wine stain never regresses and is best treated with laser photocoagulation. Tumors in Children Neuroblastoma Most common extracranial solid tumor of childhood. Has the ability to undergo maturation to a benign form, ganglioneuroma. It spontaneously disappears more than any other human malignancy. Derived from embryonic neural crest tissue. Arises anywhere in SNS. Threequarters are intraabdominal. Of these, most arise from adrenal medulla. Most children will secrete catecholamines and their breakdown products in the urine. Abdominal mass is the present feature in most patients. Tumors in the mediastinum may produce respiratory distress, or may cause Horner’s. Systemic features include fever, weight loss, failure to thrive, anemia, and HTN. Most have metastasis at dx. Surgical resection remains the mainstay of treatment and is the only method of a cure. Survival rate is 40-50%. Survival rate of infants is 75% and children older than two is only 20%. Wilms’ Tumor Embryonal neoplasm of kidney. Associated with other anomalies such as hypospadias, hemihypertrophy, and aniridia (congenital absence of iris). Usually have an asymptomatic abd mass. Sometimes, they will have abd pain, hematuria, or HTN. Metastasis is less common. Investigations include U/S and CT scans of the abd/chest. Resection of the tumor as a total or partial nephrectomy is the mainstay of treatment. All children receive chemo postoperatively. Radiation is added to those with unfavorable histology, residual tumor, or metastatic disease. Survival rate of children has improved from 10 to 80% in several decades. As with neuroblastoma, younger children fare better. Teratomas Originate early in embryonic cell division. Tumor no longer required to contain all three germ layers to be classified as a teratoma. Often occur in the gonads or near the midline of the body. Benign or malignant. Benign tumors produce symptoms by compressing adjacent organs or by torsion. Most common teratomas in children occur in the sacrococcygeal region and the ovary. Sacrococcygeal teratomas occur predominantly in girls and can be massive. Arises from the coccyx and has an external component that is covered with skin. Resection should be prompt because of the incidence of malignancy is only 10% in neonates, but increases to more than 50% by 2 months of age. Delivery by csection is recommended for large tumors b/c rupture with exsanguination can occur during vaginal delivery. Hepatic Tumors Approximately ¾ of hepatic tumors in children are malignant. Most common of these are the hepatoblastoma and hepatocellular carcinoma. Usually have an abd mass associated with discomfort, anorexia, weight loss, and occasionally jaundice. Serum a-fetoprotein levels are usually elevated. Hepatoblastoma is more common in children less than three. HCC is more common in older children and is usually more invasive. For HCC resection is the treatment of choice. Liver transplantation should be considered for unresectable hepatoblastoma w/o metastasis. Hemangiomas are the most common benign liver tumors of children. Rhabdomyosarcoma Most common soft tissue sarcoma in children. Derived from primitive mesenchymal cells. Embryonal type found in the GU tract, head/neck, and orbit. The alveolar type occurs in older children and involves the trunk and extremities. Presentation consists of an asymptomatic mass. Dx is established by biopsy. Overall the survival rate is 70% Differences in Trauma Care Between Adults and Children Blunt trauma predominates in children Blood pressure is not a sensitive sign for shock. Children can compensate for hypovolemia very effectively by increasing PVR. Hypotension develops only after more than 25% of the total blood volume is lost. Children are more vulnerable to head injury Children have a greater risk of hypothermia Children have a quite flexible skeleton, therefore major internal organ damage without overlying fractures may be possible. Injury to the epiphyseal growth plate can inhibit growth and cause deformity. Gastric distention is more common in children b/c they tend to swallow air. More likely to have lasting psychological problems Head Trauma Major cause of death of injured children. A CT scan provides excellent anatomic definition and should be obtained promptly for a suspected injury. Intracranial pressure is minimized by hyperventilation to produce hypocapnia (which limits cerebral vasodilation) and by fluid restriction and diuretics. Chest Trauma Most injuries to the chest can be managed non-operatively with chest tube drainage and supportive care. Indications for surgery are massive, continued blood loss or uncontrolled air leaks through chest tubes; pericardial tamponade; and suspected injury to the esophagus, diaphragm, and great vessels. Abdominal Trauma Abd surgery after trauma is required for a child with a distended, tense abd or free intraperitoneal air on X-ray. These finding indicate either massive intraabdominal bleeding or a perforated viscus. If abd injury is suspected a CT scan is indicated. Every effort should be made to salvage the spleen, regardless of whether surgery is required b/c children are particularly susceptible to overwhelming postsplenectomy sepsis. UT Injuries Hematuria after injury indicates a CT scan. Surgical repair is needed if there is any extravasation of urine from the kidneys or bladder, or if the major renal vessels are injured. Presence of gross blood at the urethral meatus necessitates an urethrogram to r/o urethral injury before a Foley catheter is inserted. Burns One-third of burn injuries are caused by child abuse. When calculating the % of body surface area burns in children the “rule of nines” does not apply. Must use the Lund and Browder chart (fig 2-30). Hospital admission is advised if a second-degree burn involves more than 10 % of the body SA or if a third-degree burn covers more than 2%. Inpatient care is also recommended for significant burns of the hands, feet, face, or perineum, and for children younger than 2 years old. Child Abuse Suspicious clinical features include: discrepancy btwn history and physical findings, prolonged delay before seeking medical attention, recurrent trauma, inappropriate response of parents to child or to medical advice, child is overly fearful or withdrawn, sharply demarcated burns in unusual areas, long bone factures in children < 3yrs, trauma in genital or perianal areas, multiple old scars or healed fractures, bizarre injuries (bites, cigarette burns, rope marks). Aspiration A smaller object that passes through the larynx usually lodges in a mainstem bronchus. Complete obstruction causes atelectasis as air is absorbed distally. Partial obstruction of a bronchus produces hyperinflation distally through a ball-valve effect, as the airway collapses around the object during expiration and excessive air is trapped. CXR rarely shows a radiopaque foreign body, but often demonstrates hyperinflation of the invovled lung or lobe. Expiratory films and fluoroscopy are very helpful b/c expiration exaggerates the hyperinflation and produces the mediastinal shift in the opposite direction. If there is any suspicion of foreign body aspiration, rigid bronchoscopy is performed under general anesthesia. Ingestion Symptoms of obstruction, perforation, and bleeding are indications for immediate intervention. If the swallowed object is seen lodged in the esophagus on x-ray, there is significant risk of perforation. If batteries are swallowed and do not advance beyond the stomach for 24 hours or remain in the same area of intestine for a week despite purgatives and enemas, their removal is indicated. THE BLADDER Anatomy: Empty: behind pubic symphasis Full: palpable suprapubically Detrusor muscle: has no distinct layers Trigone: 2 layers: one fuses with ureteral musculature, one is like detrusor. Entire bladder is covered with pelvic fascia Superior bladder covered with peritoneum. Puboprostatic ligaments/ pubovesicular ligaments attach bladder to posterior aspect of pelvic bone Umbilical ligament attaches bladder to anterior abdominal wall Blood supply to bladder: superior, middle, inferior vesical arteries (from hypogastric), in females also from vaginal and uterine arteries Bladder drained by many veins all going to hypogastric veins Bladder lymphatics go to external iliac, hypogastric, common iliac, and sacral lymph nodes Evaluations for anatomy: Cystoscope: visualize Retrograde pylography= inject radiocontrast into ureter to evaluate shape, size, position of ureter and renal pelvis Urodynamic Evaluation: Urodynamics: evaluates reservoir and micturation Post void residual (PVR): amount of urine in bladder post void, can measure by catheterization or by ultrasound. If increased residual than obstruction, cystocele, neurogenic bladder. Cystometrogram (CMG): Measures bladder pressures, sensation, capacity and compliance. Detects premature detrusor contractions. Normal should fill to 350- 500 mls without detrusor contraction, first sensations of void need btwn 150-250 ml, definite urge at 350-450. Urinary flow rate (uroflow)- measures flow rate from urethra, normally men have peak of 20-25 ml/sec, women 20-30 ml/sec. Low flow= obstruction, poor detrusor fitness. Urethral pressure profile= not a common test, intraluminal pressure in urethra Sphincter electromyography (EMG): evaluates sphincter activity, should increase with filling, and decrease with voiding. Fluoroscopic cystography: visualize bladder neck and sphincter, can detect cystocele, bladder prolapse, reflux. Congenital anomalies Vesicoureteral reflux: (VUR) Primary reflux: short intramural ureteral tunnel, due to lateral placement of ureteral bud from fetal bladder. Reflux of dirty urine up ureter causes kidney damage. Graded on degree: grade 1 and 2 will resolve as child matures, over 2 may require correction. Secondary reflux: secondary to a surgical intervention, may require correction. Cystitis may cause transient reflux. Clinical evaluation: VUR usually detected during UTI workup 29- 50% of kids evaluated for UTI have VUR. Voiding Cystourethrogram (VCUG) is primary test for VUR: fill bladder with contrast and observe. Radionucleotide cystogram: VCUG with a radioisotope, is more sensitive to small degrees of reflux. Renal ultrasound and IVP can detect dilatation of upper urinary tract but cannot alone diagnose reflux. Treatment of VUR: Goal is to prevent UTI and renal damage. In kids 80% will eventually resolve, use antibiotics until resolved, reculture every 3 mo, with every fever and all urinary symptoms. VCUG, renal ultrasound, creatinine, BUN, height, weight and bp annually. Surgery if repeat UTIs, poor compliance, failed management, or loss of renal fxn. Ureteral implantation, lengthens the intramural portion of the ureter, immobilizing ureteral meatus, supporting ureter. Mild reflux: can inject Teflon or collagen into bladder wall at the ureteral orifice, too new for FDA approval. There is concern about mobilization of the Teflon to the brain or lungs. Glenn-Anderson technique for VUR: makes a long submucosal tunnel for the ureters Cohen procedure for VUR: cross trigone tunneling of the ureters Politano-Leadbetter technique for VUR: ureter is totally mobilized from bladder, then brought to a new orifice created superolaterally Other anomalies: Extrophy: improper development of abdominal wall, pelvic girdle, and anterior bladder wall. Posterior bladder wall exposed, pubic symphasis separated. Uncommon, 3:1 in males, leads to incontinence, UTI’s, increased risk of adenocarcinoma of bladder. Total reconstruction needed. Uracheal persistence: can be an umbilical sinus, abdominal wall cyst, diverticula off of bladder or fistula from bladder to umbilicus. Excise to treat. Assc with adenocarcenoma. Can not tell congenital from acquired. Trauma: Penetrating: gunshot, stab, instrumentation Blunt: rupture, intra/extra peritoneal extravasation, usually other pelvic and abdominal injuries accompany, presents with severe suprapubic/pelvic pain, unable to void Evaluation: Cystogram to check for bladder rupture: contrast in bladder, image, take a post-drainage image, 15% diagnosed post drainage Retrograde urethrogram to check for urethral tear Treatment: Small extraperitoneal rupture: 1-2 wks with foley Intraperitoneal or large extraperitoneal rupture will need surgery Inflammatory disease Bacterial cystitis: irratative voiding symptoms: dysuria, frequency, urgency, nocturia, possible hematuria. More common in women- fecal contamination In men due to retention, incomplete voiding E. coli 80% of UTI’s Evaluate: UA. If not responsive to antibiotics then cystoscopy and radiography Carcinoma considered if irritation persists with UA is neg. Interstitial cystitis Etiology unknown, Mainly in women Lower abdominal pain, irritative voiding symptoms, microhematuria, negative cultures May have mucosal ulcer (Hunner’s ulcer) Dx of exclusion, pain and frequency may be debilitating Histology shows chronic inflammation, mast cell infiltration, fibrosis Treatment: bladder dilatation under general anesthesia, infusion of dimethyl sulfoxide, heparin, may need to remove bladder Degenerative diseases Bowel/bladder fistulae: caused by sigmoid diverticulitis, neoplasm, crohn’s, or penetrating injury Present with UTI, hematuria, pneumaturia, fecaluria Eval w/ enema, cystogram, cystoscopy, CT Treat: resect part of bowel, debride and close fistula Vesiculovaginal fistula: Caused by pressure necrosis during long labor or from surgical injury Presents with continuous incontinence Eval w/ cystogram, cystoscopy, IVP, or bilateral retrograde pyelography to look at upper tract Treat with surgery, vaginal approach Urinary incontinence Stress: cough, sneeze, laugh, low resistance btwn bladder neck and urethra Urge: can’t get there in time, involuntary contraction Overflow: assc with obstruction, retention, uncontrolled emptying Total: continuous, vesicovag fistula Evaluation: history: meds, trauma, surgeries, deliveries, malignancy, diabetes, UTI, bowel habits, erectile and ejaculatory function Physical exam include back, abdomen, pelvis, rectum, perianal sensation, tone, lower extremity neuro exam Treat: if detrusor unstable (stress or urge): anticholinergics will relax Surgery to restore anatomy for stress incontinence: Marshall-Marchetti-Krantz: anterior abdominal approach, dissect, tack higher Stamey: vaginal incision, uses Dacron vascular graft to bolster Raz: vaginal incision, sutures placed several times through urethropelic liagament Transvaginal “sling” for stress incontinence, modifies bladder neck, uses, fascia or anterior vaginal wall to make a sling around urethra For men there is an artificial sphincter like the one we saw in anatomy with a fluid filled reservoir and pump in the scrotum and a cuff around the urethra Neurogenic bladder (there’s a nice chart in the book) complicated, many CNS components peripheral detrusor innervation: parasympathetics from S3, S4 trigone: sympathetics from T11-L2 external sphincter: S2 via pudendal classifications: uninhibited neurogenic bladder: uncontrolled contractions lead to frequency, urgency, urge incontinence, assc. w/ CVA, tumor, cerebral palsy, dementia, MS reflex uninhibited: phasic uninhibited contractions triggered by something, may be incomplete, from suprasacral cord lesion from trauma, tumor, MS. Detrusor sphincter dyssynergia: high T or C spine injury, no sensation of filling but will get sweating, headache, HTN, spasms when full Autonomic neurogenic bladder: no efficient detrusor contractions, must increase intraabdominal pressure to void. PVR is large. From damage to sacral cord, conus medularis, cauda equine, sacral plexus trauma, myelomeningocele, pelvic surgery Sensory neurogenic bladder: no sensation, no detrusor hyperreflexia, larc capacity. Tabes dorsalis, diabetes, syringomyelia, pernicious anemia. Motor paralytic bladder: rare, no detrusor fxn, normal sensation, normal capacity. Polio, trauma, meningomyelocele, congenital. Evaluation: Urodynamics (listed above) plus renal ultrasound, and creatinine Treatment: Anticholinergics to relax detrusor Intermittent catheterization- less infection than chronic indwelling Sphincterotomy- cut the sphincter, created incontinence but protects kidney from high pressure backup Bladder carcinoma 5th most common cancer in Americans, more common in men Assc. with smoking, rubber and oil refinery work 85-90% transitional cell Adenocarcinomas assc with patent urachus and bladder dome Squamous cell assc with schistosomiasis, indwelling foley, chronic inflammation Evaluation: Hematuria, irritative voiding symptoms, imaging, cytology Staged by depth: T1a: no invasion of bm T1b: in situ T2: superficial detrusor invasion T3: deep muscle, perivesicle fat T4: adjacent organ involved Treatment T1: transurethral resection Recurrence rate is 50% and requires intravesicle chemo: thiotepa, bacillus calmette-guerin, mitomycin-C Patients are at risk for cancers in other parts of the urinary system, need cystoscopy and cytology every 3-4 mo for first 1-2 yrs. For invasive tumors: cystectomy is required. For men remove bladder, prostate, perivesical fat, and pelvic lymph nodes. For women remove bladder, anterior vaginal wall, uterus, and lymph nodes. 5 yr survival is 60% for cystectomy post T3 cancer. When you remove the bladder you need to either divert urine to the skin using an ileal conduit made of colon or you can make a bladder pouch out of bowel that connects to the urethra which avoids the need for cutaneous diversion. Urology pgs. 419-428 Prostate Anatomy: peripheral zone, central zone, and transition zone. Ejaculatory ducts empty into prostatic urethra at level of verumonatanum. Prostate composed of glandular epithelium contained within a fibromuscular stroma. BPH = transition zone, usually begins in 5th decade of life. No causal assoc. between BPH and other dz’s ie. prostatitis or cancer. Obstructive symptoms see below. Gradual onset that may progress to urinary retention. See postvoid residual – abnormal amt. of urine in bladder after voiding. Indication for treatment is usually symptomatic relief, but could also be renal failure, recurrent bladder infections or stones. Medical tx. = alpha-1-adranergic blocking agents (ie. terazosin, doxazocin, and tamsulosin (flomax). 5-alpha-reductase inhibitor = Finasteride. Blocks conversion of testosterone to DHT, and will reduce the size of the prostate by 20-30%. Surgical Tx for BPH = removal of obstructing prostate tissue by open or transurethral prostatectomy (TURP). Tx related impotence occurs in less than 5% of pts. Acute Prostatitis – inflamed prostate, may be due to bacteria (most likely E. coli) or unknown etiology. Si/Sx – fever, back pain, chills, and dysuria, with swollen prostate, boggy to touch, very tender, poss inc. WBC. Non-bacterial prostatitis is symptomatically indistinguishable from bacterial, Chlamydia trachomatis may be cause in some cases. Prostodynia – aching perineal discomfort, urinary frequency, urgency, and dysuria. Obstructive symptoms = urinary hesitancy, dribbling, and difficulty emptying the bladder. Malignant Diseases of the Prostate: Carcinoma of the prostate is #1 cancer of men and 2nd leading cause of cancer death in U.S. 95% are adenocarcinoma arising from acinar structures. Higher incidence in African American men than caucasions. Early obstructive symptoms may be present and increase as the cancer grows. Late sx’s include pelvic pain, ureteral obstruction, or bone pain from distant mets. Screening (digital rectal exam and PSA) should start at 50 yrs, and 40 yrs for those with increased risk ie. fam hx or AA’s. Most cancers arise in the peripheral zone, and on DRE the prostate may have an area of induration or nodularity. PSA – serine protease enzyme, responsible for cleaving proteins in post-ejaculatory semen. Secreted by both benign and malignant protatic epithelial cells. Elevated in men with prostatitis, BPH, or prostate cancer. Level of 4.0 ng/ml is normal, and a change of .75 ng/ml/yr is acceptable. Two forms of PSA exist, unconjugated and free, an increased ratio of free:unconjugated is seen in BPH. Transrectal Ultrasonagrophy (TRUS) – best imaging test for the prostate, but not for prostate screening. Tumor Grade – uses the Gleason score. Tumors with scores of 2 – 4 are well-differentiated, 5 -7 moderately differentiated, 8 -10 poorly differentiated. Tumor Staging – T0 = no evidence of primary tumor, T1 = clinically inapparent tumor, T2 = tumor confined within prostate, T3 = tumor extends through the prostate capsule, T4 = tumor is fixed or invades adjacent structures. If metastasis is suspected or PSA > 10/Gleason score > 7, then bone scan and lymph node dissection are performed. Bone metastasis generally not seen with PSA’s less than 20. Treatment for localized prostate cancer include radical prostatectomy or radiation. If 10 year survival is unlikely then watchful waiting is usually Tx of choice. Brachytherapy using interstitial implantation of iodine-125 or palladium -103, is currently being used but there is limited long-term follow-up for this treatment. During radical prostatectomy the neurovascular bundle which lies posteriolaterally to the prostate and urethra. Potency can be preserved in 2/3’s of cases. Survival rate post-prostatectomy with no surgical margins = 15-years disease free in 50%. Tx for Metastatic Prostate Cancer – androgen deprivation is often used. Suppression of serum testosterone can be achieved by bilat orchiectomy, and oral estrogen therapy. Estrogen therapy has been replaced with Lutenizing hormone-releasing hormone LHRH. Loss of libido and impotency are consequences of orchiectomy and hormone therapy. Hormone therapy is effective for 18 -24 months after this disease progression resumes. Pts with metastatic carcinoma of the prostate die within 2-3 years of diagnosis. III.KIDNEYS A. Anatomy Paired retroperitoneal, T12, L1-L3 Left kidney more cranial than right 11x6x3 cm 150g in males, 135g in females Gerota’s fascia – renal fascia surrounding perineal fat B. Physiology Renal and acid base physiology is important Hyponatremia as a complication of fluid absorption during TURP RTA Hypercholoremic metabolic acidosis after urinary diversion using intestine C. Blood Supply Kidneys get 20% of cardiac output One renal artery that branches – danger of ischemia HTN: long-term sequelae of renal ischemia Aberrant lower pole arteries congenital uretopelvic junction obstruction D. Trauma Mostly blunt, often MVA hematuria Asstd with rib fracture, verterbral body and transverse process fractures, flank contusions/abrasions Must consider retroperitoneal hematoma secondary to kidney trauma in shock pts E. Evaluating and Treating Trauma No need to image those with microhematuria without history of major deceleration injury or hypotension Kids with deceleration injury think avulsion of uretopelvic jxn (may have normal urinalysis) Lacs: o Minor: extends no further than renal cortex, no urinary extravasation or large hematoma, capsule may remain intact (Grades I and II) o Major: transcapsular rupture through corticomedullary junction often with extravasation or large perirenal hematoma (Grades III, IV, and V) o For more info on grades of renal trauma see fig 9-12 Hemodynamically STABLE pts: o CT scan o Minor contusion is most common o Requires renal exploration ONLY if CT shows major renal injury Hemodynamically UNSTABLE pts: o OR for lap o “one shot” IVP – give IV bolus contrast, take image 10 min later o renal exploration if expanding or pulsatile retroperitoneal hematoma or abnormality on IVP o threshold for renal exploration lower for penetrating injury Renal Exploration: incision of posterior peritoneum medial to inferior mesenteric vein and anterior to aorta with isolation of renal vessels before colonic retraction 1. Congenital Disorders Horseshoe Kidney o Most common renal fusion anomaly, usually lower pole o Dx by IVP o Si/Sx: obstruction, infection, vague abdominal discomfort o Tx: symphisiostomy (surgical division) Congenital obstruction of the urinary tract o occurs most often at the uretopelvic jxn o leads to hydronephrosis: o si/sx: palpable abdominal mass, pain, hematuria, urinary infection, fever, hypertension, renal stones o Dx: IVP or ultrasonogram o Nuclear scan is preferable to IVP in kids due to quantification of renal fxn and obstruction o Tx: Surgical repair of obstruction to prevent renal fxn loss and UTI’s Inflammatory Diseases Pyleonephritis o A clinical Dx o Si/Sx: fever, flank pain, UTI, CVA tenderness on involved side o E. coli o Chronic pyelo → renal failure (common reason for transplant) o IVP: nonspecific findings – diffuse renal enlargement w/calyceal distortion o If uncomplicated Tx outpatient with oral ABx o With sepsis or significant compromise, admit for IV ABx o If si/sx persist > a few days, CT scan to exclude abscess o Tx renal abscess by percutaneous drainage and ABx Emphysematous Pyleonephritis o Life threatening o E. coli (mostly) form gas in renal parenchyma o Seen in poorly controlled diabetics o CT diagnostic o Septic, deteriorate rapidly o Emergency nephrectomy Xanthogranulomatous pyelonephritis o Females>males o History of failure to thrive and chronic UTI, presents 5th-7th decade o CT scan: imaging of choice o Diffuse enlargement, central nephrolithiasis, spherical areas surrounding kidney in hydronephrotic pattern o Affected kidney is nonfunctional → Tx: nephrectomy GU TB o Painless frequency esp at night o Sterile pyuria → suspect TB! o Positive PPD helpful, Dx by isolation of M. tuberculosis in urine o IVP is mandatory, also get chest films and spine imaging o Give anti-TB drugs, maybe nephrectomy o Tx ureteral stricture with temp internal stenting, corticosteroids, or uereteral reimplantation in distal ureteral strictures Neoplasms Most common presentation: painless hematuria Charcot’s triad: flank pain, abdominal mass, hematuria (rarely seen all together) CT scan Cystic lesions identified by IVP and confirmed by US If tumor invasion of IVC is suspected, get an MRI Benign Neoplasms o simple cystic lesions require no intervention o complex (septations, wall thickening, calcifications) require further investigation o consider complex cyst cancer until proven otherwise o needle biopsy of little value → do partial or radical nephrectomy Malignant Neoplasms o Renal Cell Carcinoma most common primary neoplasm of kidney usually from proximal convoluted tubules typically unilateral hematuria is most common sign flank pain and palpable flank mass next most common signs may also see fever, anemia, elevated sed rate no reliable tumor markers tends to invade renal vein and IVC → right atrium mets to lungs, bone brain late mets to liver Tx: radical or partial nephrectomy Get a bone scan for bone pain or elevated Alk Phos Preop get CXR and LFTs Post op complications: bleeding, retroperitoneal abscess, ileus, wound infection o Transitional Cell Carcinoma may present as renal mass or filling defect on IVP ereteroscopy to visualize or biopsy suspicious lesions upper tract seeds lower tract ALWAYS evaluate upper tract if TCC is found in lower tract Tx: nephroureterectomy with removal of cuff of bladder Urinary Stone Disease Mostly calcium oxalate Calcium stone risk factors: RTA, hyperparathyroidism, poor hydration, immobilization, family history Uric acid stone risk factors: high purine intake, hx of gout, poor hydration, hyperuricosuria Cystine stones in families with cystinuria (disorder of cysteine, ornithine, lysing, arginine reabsorption) → stones early in life Struvite stones with chronic UTI (esp indwelling foleys!), called staghorn when occupy entire collecting system Presenting symptom for stones: renal colic (usually Dx’d in ER) Constant pain in flank often radiating to groin with N/V Microhematuria is common Requires imaging study to Dx → classically IVP Elective metabolic workup: mostly in kids or pts with recurrent stones, may include: serum calcium, PTH, electrolytes, urine pH, 24 hour urine collection to measure calcium and other electrolytes Treatment depends on size, location, composition Obstructive pyelonephritis → urologic emergency (pus under pressure) o Cystoscopically placed stent or percutaneous nephrostomy o Do NOT remove stone (can lead to sepsis) o Goal: promote drainage <5mm: pass spontaneously >8mm require intervention o stent placement o flexible or rigid uereteroscopy with stone fragmentation and extraction (electrohydraulic lithotripsy or Holmium laser) o extracorporeal shock wave lithotripsy (see p 435 for mechanism) stones in collecting system: extracorporeal shock wave lithotrips or percutaneous removal uric acid stones can be treated medically by alkalization of urine with fluids Penis may be worth reading for humor/shock factor Anatomy: 2 corpora cavernosa surrounded by tunica albuginea. 1 corpus spongiosum – encloses urethra Both covered by Bucks fascia and skin Arterial:internal pudendal – internal iliac venous: iliac veins Trauma: Possibility of urethral trauma necessitates retrograde urethrogram Testicular ultrasound – helpful esp w/ test injury o Testical injury require exploration (surgically) Superficial injuries – normal closure Amputation – reimplantation possible (keep it cold) or partial penectomy Avulsion: o Primary closure o Circumferential – remove skin to coronal sulcus and ST Skin Graft Burns – don’t debride too much; replace catheter with suprapubic catheter Fracture – rupture of tunica albuginea of c.carnosum o Exploration + removal of hematoma Malignant Dz: Premalignant o Leukoplakia- white plaque: local excision o Balantis xerotic obliterans white, atrophic, edematous penis local excision + steroids o Bowens: solitary erythematous plaque on shaft – 25% malignancy Carcinoma in Situ; Tx: YAG laser, local excision, topical 5-Fluoruracil o Erythroplasia of Queyrat – raised red well marginated areas – CIS : Tx with YAG laser, local excision, topical 5-Fluoruracil o Giant condyloma acuminatum: exophytic undistinguishable from Squamous CC. local excisionpartial or complete penectomy Squamous CC: rare in US o Common in hot, humid areas with poor hygiene and non circumcised o Presents w/ ulceration, necrosis, suppuration, hemorrhage o Exam, palpation, LFTs, CXR, CT abdomen + pelvis, bone scan o Small cancers on prepuce – Tx w/ circumcision o Partial penectomy w/ 2cm margin for small distal tumors. 5 year cure rate = 70-80% o Larger tumors – total penectomy + perineal urethrostomy o Dissect inguinal nodes if enlarged 4-6weeks after antibiotics Sentinel nodes negative 90% 5 year survival Sentinel positive unilateral 56% bilateral 9% 5 year survival o Radiation – not as effective, but works in small low stage tumors Acquired Disorders: Priapism: prolonged erection of only corpora cavernosa(spongiosum limp) o Low flow: venous flow obstructed --> thrombosis(sickle cell, leukemia, carcinoma, intracorporeal injection of impotency meds) Can treat with phenylephrine Aspiration of blood and irrigate w/ saline Winter procedure – needle biopsy of corpora allowing communication to spongiosum --> draining blood o High flow: injury to vasculature --> increased blood flow 2* vascular fistula Corporal blood gas: low flow PO2 low; high flow PO2 high Tx with embolizing vascular fistula Phimosis: firbotic contracture of foreskin – prohibiting retraction of prepuce. o poor hygiene; DM. Tx w/ improved hygiene and circumcision Paraphimosis: mild prepuce contracture --> constricting band over coronal sulcus o Urologic EMERGENCY – compress glans and retract prepuce o if above fails --> incision of constriction. Followed by circumcision Peyronies Dz: o Scarring of tunica albuginea --> plaques on dorsal penile surface o Penile curvature --> sexual incapacitation o Immature phase: painful erection, progressive curvature, indurated plaque SURGERY CONTAINDICATED DURING THIS PHASE Vit E and Potaba or colchicine --> resolve spontaneously o If medical management fails – can correct curvature with surgery o Last resort = penile prosthesis! Circumcision and Dorsal Slit: Most common operation on males in US Contraindications: myelodyplasia, hypospadias newborn: no anesthesia just sugar Adults: anesthesia (is this ethical?) procedure: o hemostats to crush ---> dorsal slit of foreskin (can stop here) o ventral incision made ---> redundant prepuce removed circumferentially after coronal sulcus viewed o mucosa and cutaneous surfaces approximated w/ absorbable sutures Urethra: Anatomy: Posterior = prostatic (transitional epi) + membranous urethra Anterior = everything else – pseudostrat to stratified columnar Paired bulbourehtral glands secrete preejac into bulbous urethra Glands of Littre – secrete preejac into penile urethra Female – urethra 4cm long. Prox 1/3 = transitional rest = strat squamous o Periurethral glands of skene – empty into distal urethra Trauma: usually blunt o Urethral injury suspected w/ blood @ meatus, inability to void, penile edema + ecchymosis o Eval: radiograph before catheterization o Tx: extravasation limited by Bucks fascia – urethral cath or suprapubic cystostomy Urethral disruption: suprapubic tube x 3 mos ---> reconstruction Malignant Dz: o Male urethral ca: rare! >60y/o 80%= SCC Tx: distal: partial -->total penectomy. Proximal: urethrectomy + cystoprostatectomy o Female Urethra ca: only GU malignancy F>M. fungating papillary mass, bleeding local extension --> vagina, bladder common noninvasive distal: Squamous CC; Tx w/ urethrectomy Promximal or panureteral involvement: Tx w/ Chemo + Rad + Excision Urethral Strictures: usually caused by straddle injury o Obstructive voiding --> UTI o Eval: if catheter cannot pass: Eval w/ retrograde urethrogram +voiding cystourethrogram. If cath passes, no stricture o Tx: short discrete stricture: dilation. Long/recurrent stricture – open urethral reconstruction (cure rate 98%) Congenital Disorders: Posterior Urethral Valves: Paired folds of mucosa from prostatic -->membranous urethra which cause obstruction Dx: usually by antenatal US, or by poor urinary stream Tx: Catheter or supapubic tube until can endoscopically ablate the valves Hypospadias: 1 in 300 incidence. External urethra on ventral surface Classified by loc’n: perineal, penoscrotal, shaft, etc. Corpus spongiosum turns into fibrous bands distally causing ventral penile curvature Perineal hypospadias may be difficult to assign gender Tx: usually before age 2. Stop curvature; bridge urethral gap Infectious Dz: Gonooccal Urethritis: incubation period 2-14d. N.gonorrhae Yellow discharge, dysuria, itching, frequency 25% asymptomatic reservoirs Dx: swab of urethra culture in Thayer Martin Medium (maybe oral/anal swabs too) Tx: Ceftriaxone if suspicion Non-Gon Urethritis: dysuria, frequency, itching, clear/white discharge Chlamydia = most common Dx: urethral swab Tx: azithromycin If Urethritis, treat for both Gon and Non Gon w/ a combo of Azithro + Ceftriaxone Testes: mesoderm, descend by gubernacular ligament in the 8th month of gestation Cremaster muscle = internal oblique extension Congenital Disorders: Cryptorchidism: nonpalpable testicle – high incidence w/ premies Anorchia: prenatal torsion, rarely agenesis; usually unilateral: 2nd testicle hypertrophies to compensate and normal fertility and hormones: o if bilaleral: hormone replacement starting @ puberty Retractile: overactive cremaster muscle; usually descend @ puberty Undescended: usually just inside internal inguinal ring o HCG stimulation --> increased testosterone but if not, intersexuality questioned o Laparoscopy – locate nonpalpable testes o Need to bring down b/c increased frequency of cancer Does not decrease risk of cancer, but makes it easier to detect o Decreased fertility Patent Processus Vaginalis – inguinal hernia o Peritoneum extending from abd cavity o Hernation of viscera possible ---> EMERGENCY SURGERY o Partial closure – hydrocele, feels like silk in scrotum o May close after birth- surgery necessary >1 y/o o Tx: High ligation @ internal inguinal ring Testicular Cord torsion: o Neonates – epididymis, testicle, tunica vaginalis, twist w/in internal spermatic fascia --> infarct o Transverse positioned testicle, anterior epididymis, loss of cremaster reflex o Adolescents: tunica vaginalis surrounds testicle o may follow vigorous activity but activity does not cause it o DDx: trauma, epididymoorchitis, viral, testicular cord torsion o Torsion of appendage – blue dot (infarct) visible through skin on scrotum o Dx: color ultrasound o Tx: surgery >6 hours irreversible testicular damage If it is bell clapper anatomy, assumed bilateral, and both sides repaired Trauma: Ultrasound o Tunica albuginea intact – conservative mgt. torn – surgery Scrotal Infections o Cellulites (G+) or fungal o Necrotizing Fasciitis – Sub Q gangrene spreads rapidly – Tx w/ debridement + ABx to prevent death Malignant Dz: testicular cancer most common; males 18-35 o Eval: transilluminating – floating testicel = hydrocele: fluid at/below testicle = spermatocele o mass involving testicle = likely malignant --> Ultrasound --> surgery o surgery --> inguinal incision (don’t make test incision b/c lymph system in cancer) remove the testicle if tumor. o Tx: o Germ cell: o Nonseminoma: differentiate along extraembryonic lines or intraembryonic obtain tumor markers before orchiectomy (AFP diagnostic for nonsemin) B-HCG may be elevated in both (nonsemin/semin) Elevated AFP after surgery – nonseminomatous tumor/ or additional tuma Staging – CT scan, lymphography, Chest X-ray/Chest CT o Seminoma: white smooth monotonus: round/clear Tx: radiation (I&IIa) Bulky higher grade – platinum based chemotx Stage I: lymph node dissection 5 yr survival = 70% Male Infertility: 60% couples conceive w/in 3mos 90% w/in 1 yr if not using protection Infertility: 40% strictly male problem. Another 20% male contributing to problem Eval: illnesses(mumps), surgery, delayed puberty, meds, toxing, cigs, pot, lubricants Phys: genitals, Klinefelters habitus, visual field defects, olfactory (hypothalamus), gynecomastia, varicocele Semen – 3 samples after abstinence for 24 hours o low volume, decreased testosterone, retrograde ejaculation, duct obstruction Tx: o Retrograde ejac: sympathommimetrics or retrieve sperm from bladder for in vitro o Obstruction: fructose test (should be fructose in ejac) TRUS Tx w/ transurethral resection o Azoospermia: Rule out CF Atrophic testicles, increased FSH --> counsel for adoption Normal findings – scrotal exploration Varicocele – it’s possible to repair… may help Impotency: 85% causes are organic Vasculogenic – most common cause impotency: arterial insufficiency o HTN, hyperlipidemia, DM, cigs, pelvic trauma Endocrinologic: low testosterone low libido o Hypogonadotropic hypogonadism + pituitary adenoma possible etiology o Serum testosterone level if low get Gn + prolactin levels then get MRI pituitary Psychogenic: anywhere from minor component to entirely responsible o REM sleep erections: if no erections while sleeping; cause = organic o Neurogenic – spinal cord injury, MS, alocohol, DM, Surgery Eval: o Nocturnal tumescence, duplex US after pharmacologic erection, carvenosometry, pudendal arteriography o Usually not performd except in young men who have had pelvic trauma (in older men it’s irreversible) Tx: o Vaccum for erection; restrictive band for maintaining o Urethral suppository (alprostadil) o Prosthesis – LAST RESORT o PDE inhibitor Viagra – Smooth muscle relaxation (contraindicated in nitrates used) Bladder Catherterization: procedure on page 461 o Clean w/ iodine, lube it up, insert (as far as possible on males), wait for urine output, inflate balloon o Probs: resistance – DON’T FORCE!! o More lube o Coude cath – larger upward point sheath to get around prostate o If stricture – consult urology