DRAFT - University of Texas System
advertisement

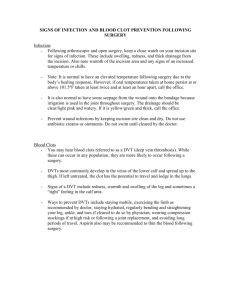
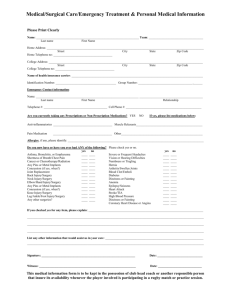
PROJECT NAME: Decreasing Colorectal Surgery Infection Rate Using a Multidisciplinary Approach Institution: South Texas Veterans Health Care System and University of Texas Health Science Center at San Antonio. Primary Author: Jose A Cadena Zuluaga MD Secondary Author: Robin Santamaria, RN Project Category: Patient Safety Overview: This was a quality improvement project to decrease the rate of colorectal surgery infections at the South Texas Veterans Health Care System in San Antonio, a quaternary level facility affiliated with the UTHSCSA. It provides healthcare services to approximately 93,000 veterans. During the first quarter of FY 2010, the infection control office noticed a high rate of infections among patients undergoing colorectal surgeries. Rates of infection were 30% during the first quarter, as compared to 20% for FY 09. A group of physicians (surgeons, infectious diseases), nurses (OR nurses, QM nurses, Infection Prevention nurse, nurse anesthetists), and pharmacists was assembled to review the perioperative care of the patients and institute evidence based interventions to decrease rates of infections. This quality improvement group was supported by the chief of staff, and hospital leadership. This project was on line with the VA Mission: Honor America’s veterans by providing exceptional health care that improves their health and well-being. Aim Statement (max points 150): To decrease the rate of colorectal surgical site infections by 30% over a 3 month period, by reviewing the patient care process and implementing evidence based practices during the perioperative care of the patients, and sustain the improvement over time. Measures of Success: We measured the rate of colorectal surgery infection per month. In addition, we monitored the implementation of evidence based measures, such as appropriate use of prophylactic antibiotics (selection, dose, duration, re dosing intervals), perioperative normothermia, glucose control, preoperative bath and skin preparation with chlorexidine (CHG). We used quality improvement tools to present the process to the hospital leadership, staff and service chiefs involved in the process. Means, and proportions, odds ratios, and 95% confidence intervals will be determined. To compare differences between groups, Chi square or Fisher’s exact tests were used. Use of Quality Tools (max points 250): Fishbone diagram- Cause Effect Diagram: Process Flow chart-Pre intervention: Process Flow Chart- Post intervention: Bair hugger temperature management system Patients goes to preprocedure appointment Colorectal surgery starts Normothermia NO YES Foley catheter placed Consent signed/ education Anesthesia adjusts temperature Bair hugger Redose antibiotics if needed during surgery Skin Prep with chlorexidine YES Proper Preoperative Antibibiotics at Clinic Using CPRS template and quick cards YES NO NO Door monitor System. Doors opening during surgery? Surgeon/ OR Check antibiotics NO Hair clipping Alarms alert OR staff to close door OR Humidity and Temperature YES YES Wound dressing Silver coated dressing Patient transferred to OR NO Patient comes to \ hospital/ check in Alarms Alert Engineering for correction Surgeon reviews Chlorexidine bath Wound class confirmed YES IV placed and MRSA screening done Proper preoperative antibiotics administered NO Patient transferred to SICU Process Control Charts: Per month, Pre and Post Intervention: Per Quarter: Pre and Post intervention: Interventions (max points 150 includes points for innovation): The QI improvement team plan was to review all the evidence based measures to decrease colorectal surgery infections, and implement those interventions consecutively, while tracking the implementation rate. All team members contributed to select the interventions based on their knowledge. Infectious diseases, pharmacy and surgery reviewed the literature and suggested improving the preoperative antibiotic prophylaxis, based on recommendations from the IDSA, ASHP and SCIP. A retrospective review revealed that the compliance with the guidelines was 50%. During the first phase of the working group the focus was to improve antibiotic administration. This was corrected by updating the antibiotic prophylactic cards used by residents and staff. In addition, an electronic medical record template was created to facilitate perioperative antibiotic administration. Timing of antibiotic administration was standardized, to be administered within one hour of incision, even among those patients receiving antibiotics for other reasons. Skin preparation was changed from a surgeon specific protocol based on preferences to chlorexidine skin preparation (N Engl J Med 2010;362:18-26, British Journal of Surgery 2010; 97: 1614–1620). Perioperative normothermia was closely monitored and encouraged. A new system to ensure 100% normothermia was successfully implemented by anesthesia (N Engl J Med 1996;334:1209-15). Glucose levels were monitored closely in all patients to evaluate if hyperglycemia was a contributing factor. However, it was ruled out by chart review (J Gastrointest Surg (2009) 13:508–515). Training of surgery residents on hand hygiene was performed monthly when they started surgery rotation, as well as education on antibiotic prophylaxis during surgery. Residents received a quick card that explained the preferred regimens. Nurses from the OR observed that the doors in the OR had automatic sensors that would open the doors during procedures. These doors were deactivated to ensure maintenance of positive air pressure in the OR. Also, an alarm was installed to alert providers if doors were left open. Improved control of temperature and humidity in the OR was achieved. The alarm systems were also more easily monitored by engineering. When temperature or humidity deviated from the standard, they were quickly corrected. The timeline of the implementation of change varied over time, and was modified in accordance with the Plan-Do-Study- Act process improvement approach. Initially there was a focus on data analysis followed by improvement in administration of perioperative antibiotic prophylaxis, hair removal, and normothermia adjustments (February to September 2010). After this, rates of infection decreased. The QI improvement team thought that they had achieved their main goal. However, rates started to increase and the team met again and started evaluating and implementing additional interventions on April 2011 (CHG skin preparation and use of CHG impregnated wipes prior to surgery at preoperative area), CHG skin preparation was associated with additional decrease in the rates of infection, and sustained infection rate change. During review there were some discordances regarding wound classification. This was standardized after an in- service was provided to the OR staff. Also, reference cards for wound classification were disseminated. Surgeons were asked to verify wound class to facilitate surveillance requirements. Information regarding the progress of the QI group was presented at the infection control committee, and at the Clinical Executive Board meetings every other month, during the preparation and implementation period of the project. Results (max points 250): Prophylactic antibiotics: Preoperative antibiotic use was evaluated before intervention: - June 2009, proper antibiotic choice was observed on 73 %, timing in 81%. - December 2010, proper antibiotic choice in 56% (5/9), timing in 67%, (6/9). Post intervention: - March 2010, proper antibiotic choice 88% ( 7/8). - June 2010, proper antibiotic choice: 100%, (9/9), Timing 9/9 (100%), dose 7/9 (78%). - July 2012, proper antibiotic choice: 100%( 12/12), Timing 100%, choice 100%. Normothermia: Pre intervention: - June 09 11 surg reviewed 4 correct - Post intervention: - May 10: 80% (8/10) maintained normothermia - Jul 11: 100% (12/12) maintained normothermia. CHG bath before surgery: (Implemented May 2011) - Aug 11: 100% 9/9 preoperative bath with CHG impregnated cloths. - Sept 11: 80% (8/10) preoperative bath with CHG impregnated cloths Glucose control: - Feb 11 No hyperglycemia within 48 hours of surgery: 82% (9/11). - July 11 No hyperglycemia within 48 hours of surgery: 83% (10/12). The team, led by a Pham D, reviewed and found no significant correlation between infection and hyperglycemia. CHG skin prep: Pre intervention: - Oct/Nov 2010: CHG use for skin preparation before surgery: 73%. 11/15. - July 2011: CHG use for skin preparation before surgery: 50% (6/12). At this time we enforced CHG skin prep. Post intervention: - Aug 2011 CHG use for skin preparation before surgery: 100% (9/9) - Sept 2011 CHG use for skin preparation before surgery: 70% (7/10) - Feb 2012 CHG use for skin preparation before surgery: 62%, (8/13) There was no association between use of hand ports during surgery and infection on analysis so we did not continue to track this measurement. The rate of surgical site infection among patients undergoing clean or clean contaminated colorectal surgeries decreased from 23% (24/104) during the pre-intervention period to 16% ( 37/226) during the post intervention period (OR: 0.65, 95% CI: 0.4- 1.2, p:0.15) Revenue Enhancement /Cost Avoidance / Generalizability (max points 200): At the ALMVA we perform an average of 90 clean/ clean contaminated colorectal surgeries a year. If we decrease the rate of infection from 23% to 16%, we would be able to avoid about 7 surgical site infections per year. Our QI project has already been running over 2.5 years, so it may have led to avoiding about 18 surgical site infections. The cost of a general surgery infection in the US is estimated to be $10,497 dollars (Surgery 2011; 150:934-42). This allows us to calculate a possible cost avoidance of $188,946 dollars during the intervention period. We did not use additional staff or resources to implement our interventions; beyond those already planned by the institution (i.e. remodeling of the ORs was an ongoing process, we only standardized clinical care processes). We are planning to share our experience with the UT affiliated hospitals participating on the UT infection prevention collaborative so they can implement their own processes to decrease colorectal SSIs. Conclusions and Next Steps: Colorectal surgical site infection rates can be decreased when implementing a bundle of evidence based practices including proper perioperative antibiotic dosing, skin preparation with CHG, increased education on hand hygiene, sustained perioperative normothermia and avoidance of frequent unintended opening of operating room doors. This goes in line with the organizational goals to provide the best possible care to our veterans. We plan to continue monitoring the application of these evidence base interventions and make them part of our patient safety culture. We will continue to monitor our rates of infection and share our experience with other hospitals involved in the UT infection prevention collaborative, in order to provide them with information about the implementation process of best practices.