Pediatric Simulation--Child with Neurological
advertisement

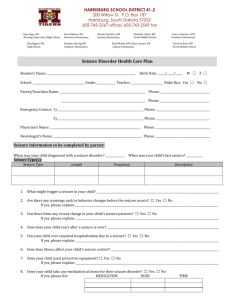
1 JACKSON STATE COMMUNITY COLLEGE Department of Nursing NUR 140 Clinical Simulation Instructor Handout: Child with Neurological Disorder Remember to try not to lecture or read all of the data to the students – have them get the data. Scenario: Simon Kidd is a 5-year-old with congenital hydrocephalus who had a V-P shunt placed when he was an infant. Mom brought him to the ED because he has started to have some irritability and is complaining of a headache. He also had a temp of 102.7 this am. Mom gave him Motrin. He is admitted to the pediatric unit for suspected shunt failure secondary to infection and monitoring for increased intracranial pressure. 1. Upon admission what should be included in the neuro exam? Mental Status – Decreased LOC Could use Glasgow Coma Scale (Eye opening, verbal response, physical response) Could test Cranial Nerves – Contralateral motor or sensory losses Pupillary changes – dilation with slowed constriction, visual disturbances such as diplopia, ptosis 2. What would be your next steps in assessing Simon? Vital signs including temp, BP, and pox Temp = 38.9, HR = 118, RR = 26 BP = 122/70 (pt is crying and it is difficult to obtain an accurate BP) Pox 98% on RA Full physical assessment - should be done on every pt Ask parents if they’ve noticed any changes in their child’s personality, mental status. Sometimes parents will state that their child just isn’t “right”. Developmental assessment. Getting pt ready for possible diagnostic tests – CT scan if ordered by MD 3. What are the interventions you as the nurse would employ to ensure the safety of this patient? Prepare room for seizure precautions: o Pad side rails o Have O2 and suction in the room o Determine what medication will be needed if he does seize – Usually Ativan during active seizure Start an IV for emergencies (Should be ordered) 4. Simon is admitted for us to monitor for increased ICP. What are the signs of increased intracranial pressure? Decreased LOC Behavior changes Headache Nausea and vomiting Aphasia Pupillary changes Cranial nerve dysfunction - III (oculomotor) – movement of eye muscles 2 Seizures VS – bradycardia, widening pulse pressure – LATE! Respiratory dysrhythmias (shallow, slowed respirations, irregular patters or periods of apnea – LATE!) **Cushing’s Triad: Bradycardia, Hypertension, & resp changes* ***Infant assessment – remember sunsetting eyes, bulging fontanelles, increased head circumference 5. What would be the nursing interventions you would employ to decrease the cranial pressure? Remember the 3 components of the head: brain, blood/fluid, CSF Elevate the head of the bed to assist venous drainage from the skull Align the head straight to assist venous drainage Give the pt a diuretic to decrease the circulating volume (usually Mannitol – use filter – crystallizes very easily) Give the pt an anti-inflammatory (usually a steroid – decadron) to decrease brain swelling if that is the problem Shunt revision EVD (external ventricular drain – PICU settings) if infected VP shunt Hyperventilation – LATE intervention – PICU 6. While preparing to hang the patient’s IVF the patient begins to seize. What will you do? How will you respond? What will you document? Maintain an airway during an dafter the seizure Do not leave the patient Maintain safety for the pt during the event – do not put anything in the patient’s mouth Note the time the seizure began Monitor the type of movements the pt has during their seizure Monitor the eye gaze and direction Determine if the patient is at all conscious through the seizure Monitor for length of the seizure Is the patient incontinent during or after the seizure? How long is the postictal phase? 7. You walk into the room after caring for this pt for several hours. He has been alert and oriented all day. He is now confused and has pulled out his IV. What has changed? His level of consciousness has changed. What will you assess? (Have students assess the pt as they would if they had been the one to enter his room) LOC Pupils – one is dilated (see note) VS Does he have increased ICP? Has his shunt stopped working? Has his infection gotten worse and affected the shunt function? **Note: If you can dilate one of Simon’s pupils do that so that will be a finding for the students. If not then tell them that one of his pupils is dilated. 8. What will you do with this information? Stay with the patient Monitor for seizure Put HOB up and align head 3 Put on oxygen Call for assistance and for someone to contact the MD immediately 9. The pt is taken to the OR to have her shunt changed. It was occluded from an infection and she is D/C’d home a week later – nice save! Give yourself a pat on the back. 4 JACKSON STATE COMMUNITY COLLEGE Department of Nursing NUR 140 Clinical Simulation Student Handout: Child with Neurological Disorder Simon Kidd is a 5-year-old boy with congenital hydrocephalus who had a V-P shunt placed when he was an infant. Mom brought him to the ED because he has started to have some irritability and is complaining of a headache. He also had a temp of 102.7 this am. Mom gave him Motrin. He is admitted to the pediatric unit for suspected shunt failure secondary to infection and monitoring for increased intracranial pressure. 1. Upon admission what should be included in the neuro exam? 2. What would be your next steps in assessing Simon? 3. What are the interventions you as the nurse would employ to ensure the safety of this patient? 4. Simon is admitted for us to monitor for increased ICP. What are the signs of increased intracranial pressure? 5. What would be the nursing interventions you would employ to decrease the cranial pressure? 7. While preparing to hang the patient’s IVF the patient begins to seize. What will you do? How will you respond? What will you document? 7. You walk into the room after caring for this pt for several hours. He has been alert and oriented all day. He is now confused and has pulled out his IV. What has changed? What will you assess? 8. What will you do with this information? 9. The pt is taken to the OR to have his shunt changed. It was occluded from an infection and he is D/C’d home a week later – nice save! Give yourself a pat on the back. 5 PEDIATRIC SIMULATION NEUROLOGICAL- INCREASED INTRACRANIAL PRESSURE AND SEIZURES DATE/TIME July 20, 2007 Time: 4:00PM SUBJECTIVE AND OBJECTIVE DATA MINIMAL EXPECTED STUDENT BEHAVIOR PROMPTS AND QUESTIONS TEACHING POINTS Physical Assessment: Student should have room with proper equipment. (suction, oxygen, padding of rails/extra pillows to prevent injury during seizure) What safety precautions should be initiated in this patient’s room in relationship to his condition and history? Pain Scale: 6 Neuro: Alert and oriented. Quiet. No acute distress Pupils- PERRL HR- 118 Ht-60” RR- 26 Wt-65lbs T- 102 BP- 122/70 Pulse Ox- 98% Student should ask questions to mother about change in behavior/personality. Physician’s Orders Student should investigate what the child’s developmental level is at present prior to illness. Admit to Ped Unit Neuro checks q 1hr x 4, then q 4hrs if stable IV D5 ½ NS at 60cc/hr Ativan 1mg IV q 4hrs prn seizure activity Vital signs q 4 hours Activity: Bed rest with BR privileges CBC,BMP,CXR, CT of head Complete physical assessment Should focus on neuro checks Which order should be done first? 6 Change in Neurological Status: Pt begins to have a seizure (will shake pt to simulate seizure) Should incorporate measures that would decrease the cranial pressure During seizure pt will vomit. Pt’s LOC has changed. Neuro: Decreased LOC Pupils- Rt pupil is dilated 3cm with slowed constriction Lt pupil- dilated no reaction Confused and combative. C/O blurred vision. Vital Signs: HR- 50 BP- 110/46 RR- 16 T-100 Student should initiate safety measures: turn to side, protect from injury, side rails up and padded, assure airway is patent. Student should know what to record about the seizure activity. Student should do a complete assessment, administer ativan safely with dose calculations, and notify physician of change in neuro status and recognize S/S of ICP Student should apply oxygen 2L/minute, stay with patient, Elevate HOB and keep in alignment. Designate another team member to contact physician. What is the biggest risk for the patient during the seizure activity? What do you do to assure the airway is patent? What are S/S of ICP? 7