Pediatric Anesthesia (CA 3)
advertisement

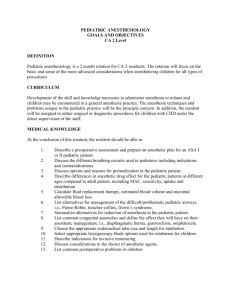
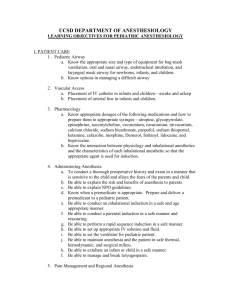
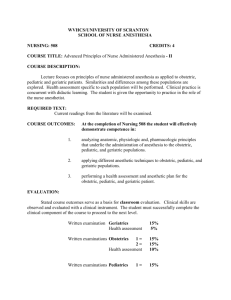
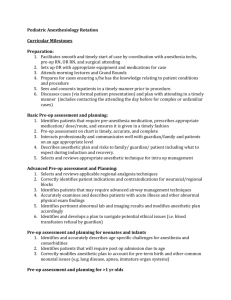
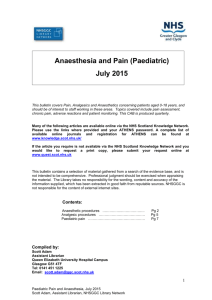
PEDIATRIC ANESTHESIOLOGY GOALS AND OBJECTIVES CA 3 Level DEFINITION Pediatric anesthesiology is a 1-3 month rotation for CA-3 residents. The rotation will continue to focus on all forms of anesthesia for pediatric patients having simple and complex operations, including those who may have congenital heart disease. CURRICULUM Development of the skill and knowledge necessary to administer anesthesia to infants and children may be encountered in a general anesthesia practice. The anesthesia techniques and problems unique to the pediatric practice will be the principle concern. In addition, interested residents may be assigned to either surgical or diagnostic procedures for children with CHD under the direct supervision of the attending staff. MEDICAL KNOWLEDGE At the conclusion of this rotation, the resident should be able to: 1. Describe a preoperative assessment and prepare an anesthetic plan for an ASA IIII pediatric patient. 2. List several options for premedication in the pediatric patient. 3. Determine the differences in anesthetic drug effects for the neonate and infant 4. Calculate fluid replacement therapy, estimated blood volume and maximal allowable blood loss for more extensive operations 5. Calculate the volume of blood and or blood products that should be used when transfusion is required 6. Evaluate and list management strategies for difficult/problematic pediatric airways, i.e., Pierre-Robin, Goldenhar’s, and Down’s syndrome, including potential problems that can occur with the use of the smallest fiberoptic scopes. 7. Describe common congenital anomalies and define their anesthetic considerations i.e., diaphragmatic hernia, gastroschisis, omphalocele 8. Differentiate between gastroschisis and omphalocele 9. Determine appropriate laryngoscope blade, tube size and length for intubation. 10. Illustrate situations where the use of LMA is appropriate 11. Present the indications for invasive monitoring. 12. Justify the choice of anesthetic agents. 13. Describe the differences in cardiopulmonary bypass for infants and children.(optional) 14. Describe immediate postoperative care and common complications. 15. Recognize the impact of URI, and RAD on anesthetic management in pediatric patients 16. 17. 18. 19. Appreciate side-effects of seizure medications, anti-depressants and bronchodilators and their potential adverse reactions during anesthesia Determine situations where SBE antibiotic prophylaxis is and isn’t indicated Describe the anatomy and physiologic derangements of the most common cardiac abnormalities: ASD, VSD, Tetralogy of Fallot, PDA and Coarctation Discuss the impact of intra-cardiac shunts on anesthetic management PATIENT CARE At the conclusion of this rotation, the resident should be able to: 1) Manage children with a normal pediatric airway utilizing appropriate mask, bag and oral airway. 2) Evaluate and plan the management of children with more difficult airway anatomy. 3) Manage bag mask, +/- oral airway in children with more difficult airway anatomy 4) Intubate children with a normal pediatric airway with skill and quickness using appropriate blade, tube in the majority (>95%) of cases. 5) Obtain appropriate intravenous access in the majority patients, including some infants and toddlers (>75%) 6) Obtain appropriate intra-arterial access in some cases. 7) Recognize appropriate blood warming equipment and filters for transfusion in pediatric patients. 8) Manage an appropriate anesthetic for more advanced pediatric cases . 9) Perform basic pediatric regional anesthesia with staff supervision: a) Caudal Epidural b) Lumbar Epidural c) Simple Peripheral Nerve Blocks . 10) Recognize and manage laryngospasm in the pediatric patient. 11) Recognize and treat common post-operative respiratory complications including croup/stridor, laryngospasm and bronchospasm. 12) Maintain stabilization on arrival to PACU/ICU. INTERPERSONAL AND COMMUNICATION SKILLS At the conclusion of this rotation, the resident will: 1) Discuss important differences in treating neonates, children and adolescents in all areas mentioned above. 2) Access current literature to delineate specific concerns regarding the perioperative care of all scheduled complex cases she/he is assigned. 3) Perform preoperative consultations of seriously ill children and communicate effectively with staff anesthesiologists, surgeons and family. 4) Describe the combination of techniques and therapies for providing no pain, memory or movement of the child during planned procedures. 5) Create rapport with parents, caretakers, children and surgeons. 6) Evaluate and prepare children with simple or repaired cardiac lesions. 2 7) Determine which children require premedication. 8) Interface effectively with parents. 9) Develop a reasonable plan with the attending staff. 10) Follow the postoperative course of their patients. 11) Provide guidance and care for patients on the Pain Service. 12) Communicate changes effectively with pain service team, floor nurses and family. PROFESSIONALISM At the conclusion of this rotation, the resident will: 1) 2) 3) 4) 5) 6) 7) 8) Function effectively in the O.R. through effective interface with the surgical team. Safely transfer the children to the PACU/PICU. Effectively communicate immediate postoperative plans. Secure consent and provide assurance to parents of pre-anesthetic children. Arrange and participate in a parent-present induction of anesthesia for a child. Provide consultative services preoperatively for all kinds of pediatric procedures. Establish reasonable analgesia plans for all types of pediatric surgery. Follow patients post-operatively on the Pain Service. Rev. 7/2009 3