Anesthesia

Anesthesia
Animals subjected to painful or anxiety-producing procedures must receive appropriate anesthetics, analgesics, and tranquilizing agents, except for cases approved by the Institutional
Animal Care and Use Committee (IACUC), when the use of these agents will interfere with the experiment. Justification must be supported by scientific rational. All drugs and compounds used in research, teaching, and testing are expected to be pharmaceutical grade compounds. The use of non-pharmaceutical grade compound requires approval from the IACUC.
General Information
Variations in dose and duration of action may be observed due to factors such as animal strain, route of administration, weight, temperament, presence of other drugs, sex, time of day, and the health status of the animal. Because of these considerations, animal users must be able to judge depth of anesthesia in the individual animal to avoid giving a lethal dose or a dose inadequate to control pain. Determining anesthetic depth requires frequent monitoring. Response to painful stimuli, such as withdrawal response to ear or toe pinch in rodents and rabbits, and toe pinch and corneal reflexes in carnivores, are good anesthetic depth indicators. Monitoring heart rate, oxygen saturation, respiratory rate, and temperature are recommended.
A patent airway should be maintained during surgery in nonrodents by using an endotracheal tube. Animals are very prone to hypothermia under anesthesia. They must be insulated from cold (room temperature) surfaces and require supplemental heat, usually in the form of circulating warm water pads. Thermal injury can occur from uncontrolled heat sources such as heat lamps and electrical heating pads. When animals have been administered anesthetics and analgesics for a surgical procedure, they are less likely to respond to being overheated by a heating lamp than a conscious, lucid animal.
If significant blood loss occurs, replacement fluids must be given to maintain normal body functions and to avoid shock; the amount of crystalloid fluids (e.g. lactated ringers solution,
0.9% NaCl) given to compensate for blood loss should be approximately 3 times the amount of blood loss.
It may be necessary to control salivary and respiratory secretions via atropine or glycopyrrolate.
If asepsis is accidentally compromised during surgery, antibiotics should be used to control postoperative infection. Antibiotics are most effective when given such that they reach adequate blood levels at the time of the surgery. Therefore, intramuscular (IM) antibiotics are best given before surgery.
Anesthetic Monitoring
Anesthesia must be monitored to ensure an appropriate depth. Anesthesia must be deep enough to provide adequate analgesia to the animal; however, excessive anesthetic depth is can result in the animal’s death. Monitoring cardiovascular and respiratory parameters, temperature, muscle tone, and muscle reflexes allow the anesthetist to ensure appropriate anesthetic depth, and should anesthetic problems arise they are recognized and treated rapidly.
Cardiovascular Parameters
Noxious surgical stimulation activates the sympathetic nervous system, often causing increased heart rate and blood pressure. It’s important to realize these changes occur in response to surgical stimuli even when anesthetic concentrations are high enough to prevent the animal from perceiving pain. In other words, if an animal seems adequately anesthetized on the basis of muscular relaxation and muscle reflexes, it may not be necessary to increase anesthetic depth when heart rate and blood pressure increase in response to surgical stimulation. The major exception to this rule is when neuromuscular blockers are used; in these cases, autonomic responses are often the only method to judge anesthetic depth. Therefore, if heart rate and blood pressure increase by 20% or more without another obvious cause, anesthetic depth should be increased when using a neuromuscular blocker.
Heart Rate – Tachycardia (rapid heart rate) can result from light anesthesia, low blood pressure, hypovolemia, hypoxemia, hypercarbia, and hyperthermia. Tachycardia is not necessarily suggestive of light anesthesia with inhalant anesthesia such as isoflurane. Bradycardia (slow heart rate) can also result from certain agents (especially xylazine, medetomidine, and the opioids), vagal reflexes (intubation, hypertension, abdominal disease), low body temperature, high blood potassium, or heart disease. Bradycardias due to opioids and vagal reflexes often resolve when the animal is given atropine or glycopyrrolate. Bradycardia due to xylazine or medetomidine may or may not resolve when the animal is given atropine or glycopyrrolate; decreased cardiac output due to xylazine and medetomidine does not resolve with anticholinergics. It may require reversing the xylazine or medetomidine with yohimbine or atipamezole).
Capillary Refill Time (CRT) - The CRT is the time the gums, or other vascular mucous membrane, take to return to normal color after blanching them with digital pressure. Usually,
CRT is 2 seconds or less. If longer than 2 seconds, then hypotension may be present.
Hypothermia and pain can also cause a prolonged CRT.
Arterial Blood Pressure - Mean arterial blood pressure must be greater than 60 mm Hg to maintain adequate tissue perfusion. If measuring blood pressure with a Doppler ultrasonic monitor, systolic blood pressure greater than 100 mm Hg generally indicates adequate tissue blood flow. Low blood pressure may be due to excessively deep anesthesia, excessive blood loss, peripheral vasodilation, or heart disease.
Electrocardiogram (ECG) - ECGs allow the anesthetist to see heart rate and rhythm. ECGs show only the heart’s electrical activity, not its ability to perfuse tissues.
Respiratory Parameters
Respiratory Rate - Because of the pronounced variation between species, the anesthetist must be familiar with each species’ normal respiratory rate. Most anesthetic agents depress respiration, therefore the rate generally decreases as anesthetic depth increases. If this causes hypoventilation, the animal may require mechanical ventilation.
Tidal Volume - The tidal volume is the amount of gas entering the respiratory tract during one breathing cycle. This is usually monitored subjectively, by looking at chest wall movement or rebreathing bag movement. Ruminants, rabbits, and guinea pigs may develop abdominal distension secondary to gas accumulation in their gastrointestinal tracts, compromising
respiration. If this occurs, chest wall motion may be exaggerated, even though the animal is inhaling little air; therefore, always evaluate concurrent movement of volume in the rebreathing bag to confirm adequate tidal volume.
Mucous Membrane Color: - Unless pigmented, the gums (or other mucous membranes) should be pink in color. Cyanosis, due to reduced hemoglobin in the blood, may occur when an animal is severely hypoxemic. However, anemic animals will usually not exhibit cyanosis even with severe hypoxemia. Cyanosis always requires immediate treatment to increase blood oxygen.
Pulse Oximetry - Pulse oximeters measure oxygen saturation level of the hemoglobin in the arterial blood, which is related to the partial pressure of oxygen. Oxygen saturation in animals on supplemental oxygen should be 98-100%. Oxygen saturation in animals breathing room air should be at least 95%. An oxygen saturation of 90 % corresponds to a blood oxygen pressure of
60 mm Hg, which is hypoxemic. In this situation, the anesthetist should take immediate steps to improve oxygenation, such as giving 100% oxygen, inserting an endotracheal tube, and assisting ventilation. Hypotension and hypothermia will impair the pulse oximeter’s accuracy, because it depends on adequate tissue perfusion. Patient movement, bright external light sources, hair and pigmented skin may also interfere with pulse oximetry. It is important to note that oxygen saturation will not allow you to assess the patient’s carbon dioxide status. Either capnography or blood gas analysis is needed to assess this.
Capnography - End-tidal CO
2
reflects the partial pressure of CO
2
in the arterial blood. In very small animals, end-tidal CO
2
may underestimate arterial CO
2
. In general, end-tidal CO
2
of 35-45 mm Hg is normal. End-tidal CO
2
greater than 45 mm Hg suggests hypoventilation, exhausted
CO2 absorber or rarely, developing malignant hyperthermia (mostly in swine). End-tidal CO
2 less than 35 mm Hg suggests iatrogenic hyperventilation, or reduced lung perfusion.
Central Nervous System Parameters
Thermoregulation - Anesthetic depression of brain thermoregulatory mechanisms, hair removal, wetting with disinfectant solutions, and opening a body cavity predispose anesthetized animals to hypothermia. Esophageal temperature is a fairly accurate reflection of core body temperature, while rectal temperature decreases more slowly. Minimize hypothermia by using a circulating water warming blanket and warmed supplemental fluids. Avoid electric heating pads, which can cause serious thermal burns. Animals will also benefit from the using bubble wrap or other methodologies to minimize heat loss.
Anesthetic Depth - Adequate anesthesia involves unconsciousness to prevent pain perception, and usually also involves muscular relaxation . Ketamine alone will not cause muscle relaxation.
Anesthetic depth varies with the type of procedure and the type of animal. Some species, especially sheep, are more tolerant of surgical manipulation than others, such as rabbit. Very painful procedures (e.g. periosteal or joint capsule incision, visceral traction, and corneal procedures) require a deeper level of anesthesia than other procedures. The anesthetist must frequently assess anesthetic depth as different tissues are manipulated during a procedure.
Voluntary movement in response to a surgical stimulus may indicate light anesthesia.
The pedal withdrawal reflex is another useful method to assess anesthetic depth. Extend the leg and pinch a toe with fingernails or gently with a hemostat. If the animal withdraws the leg in response, then administer additional anesthesia before initiating any painful procedures. The
ears of rabbits and rodents can be tested similarly, with head shaking indicating more anesthetic is needed.
Jaw tone also helps assess muscle relaxation and anesthetic depth in certain species. If the animal closes its mouth as the mandible is moved, more anesthesia is needed. Purposeful movement is an indication of light anesthetic depth and usually occurs in response to painful stimulus.
Ocular reflexes can also be used to assess anesthetic depth. The palpebral response is blinking that occurs when the eyelid is lightly touched. Most species lose this response fairly early in surgical anesthesia. However, rabbits are an exception as they may maintain a palpebral response even at deeper planes of anesthesia. Animals anesthetized with ketamine usually continue to show a palpebral response. Nystagmus indicates a light plane of anesthesia, except in ruminants.
Monitoring of Anesthetic Depth in Specific Species: (not applicable when using ketamine alone)
Rabbits - The pinna reflex (ear movement in response to an ear pinch) is usually the most accurate measure of anesthetic depth. The pedal withdrawal reflex and jaw tone are also helpful.
Ocular reflexes are not helpful, because rabbits often maintain the palpebral reflex even during deep anesthesia.
Ferrets - Muscle relaxation and loss of the pedal withdrawal reflex are recommended to monitor anesthetic depth in ferrets.
Cattle, Sheep and Goats - The palpebral reflex disappears with very light anesthesia in these species, so it’s not a reliable indicator. Chewing should not occur when the jaw is stimulated.
Lightly anesthetized sheep show a dorso-lateral eye position. However, adequately to deeply anesthetized sheep have a centrally positioned eyeball with a dilated pupil. Since it’s difficult to differentiate adequate from excessive anesthesia on the basis of these eye signs, it’s worthwhile to try to decrease the anesthesia. Surgical anesthesia in cattle causes ventral eye movement, so that the cornea is completely hidden by the lower eyelid. As anesthesia becomes deeper, the cornea moves back to the center of the eye; a centrally located cornea in an anesthetized cow suggests that the anesthesia is too deep. (Note: if ketamine is used to induce anesthesia, the eye will remain fixed and central regardless of anesthetic depth, for about the first 30 minutes.)
Active regurgitation (explosive discharge of rumen contents, particularly when the larynx is stimulated) usually indicates an anesthetic level that is too light. Passive regurgitation (a continual stream of rumen fluid draining from the mouth) usually signifies moderate to deep levels of anesthesia. When passive regurgitation is present, try to decrease the anesthetic depth so that the esophageal sphincter is not so relaxed. However, in non-fasted ruminants, regurgitation can occur continuously regardless of anesthetic depth.
Swine - Ocular reflexes are unreliable in assessing anesthetic depth in pigs. If the pig is adequately anesthetized, it should have a relaxed jaw tone, and the pedal withdrawal reflex should be absent.
Rodents - The pedal withdrawal reflex, palpebral or pinnal reflex, and jaw tone (in larger rodents) can be used to assess anesthetic depth. Purposeless “swimming” movements can occur even very deeply anesthetized.
Anesthetic Agents
Ketamine (Vetalar, Ketaset, Ketalar) is a dissociative anesthetic which is supplied as a slightly acidic solution with a pH of 3.7-4.5. It may be administered intramuscularly, intraperitoneally, or intravenously to laboratory animals. Additional doses of anesthetics should be 50% of the initial dose.
Mechanism of action - Ketamine appears to alter the reactivity of the CNS to various sensory impulses without blocking the sensory input at spinal or brain stem levels. The input may reach cortical receiving areas, but fails to be perceived because of depression or disorganization of the associated areas during periods of anesthesia.
Physiologic effects - There are species specific differences in the degree of CNS stimulation produced by ketamine. Due to CNS stimulation in species with low seizure thresholds, poor or inconsistent analgesia, especially poor visceral anesthesia, and poor muscle relaxation, ketamine is usually combined with various tranquilizers, narcotics, barbiturates, or inhalational agents.
When multiple drug protocols are used, ketamine dosages may need to be modified due to potentiation of actions. Due to increased sympathetic tone, ketamine tends to maintain or increase heart rate, blood pressure, and cardiac output. Respiratory rate may increase, tidal volume may decrease, and an apneustic breathing pattern may be produced. Most pulmonary function tests remain within normal limits. Higher doses are more likely to produce respiratory depression, hypoxemia, and hypercarbia.
Indications/contraindications - Somatic analgesia is produced by ketamine alone or the combination of ketamine with tranquilizers. Visceral analgesia requires the combination of ketamine with narcotic, alpha adrenergic (e.g. xylazine), or inhalational agents. Somatic analgesia is adequate for minor surgical procedures. More extensive procedures such as entering major body cavities requires visceral analgesia. Clinically, animals with hepatic dysfunction do not metabolize ketamine as rapidly as normal animals. Animals with renal dysfunction or obstruction have prolonged sleep times or may not recover. It appears to be strain-dependent, working better in C57B6 mice.
Xylazine (Rompun, Gemini) is a potent Alpha-2-receptor agonist, non-narcotic sedative and analgesic as well as a muscle relaxant. Xylazine is available in 2% and 10% solutions with an adjusted pH of 5.5. It may be administered by intravenous, subcutaneous, intramuscular, and intraperitoneal routes.
Mechanism of action: Sedative and analgesic activity are related to central nervous system depression mediated by stimulation of alpha-2-receptors. The muscle relaxant effect is based on inhibition of intraneural transmission of impulses in the CNS. Alpha-2-receptor antagonists, such as rauwolscine, idaxozan, priscoline, and yohimbine, selectively block the alpha-2-receptors. The latter two are available clinically.
Physiologic effects - High doses of xylazine may be accompanied by cardiovascular and respiratory depression and arrhythmias (bradycardia, decreased cardiac output, increased central venous pressure, and heartblock). Xylazine causes hyperglycemia, diuresis, and increased uterine pressure and/or contraction. Xylazine may depress thermoregulation during the procedure and for several hours after sedation is no longer evident. Temperature monitoring intra- and postoperatively, along with appropriate nursing care such as frequent turning of the animal and supplemental heat will increase the success of the procedure.
Indications/contraindications - Xylazine is a useful preanesthetic agent, sedative, short-acting analgesic in animals. When used by itself, some animals may awaken suddenly with signs of aggression, so use alone as sedation in potentially aggressive animals is not recommended. Its major use is found when it is combined with ketamine to provide anesthesia with visceral analgesia. Xylazine will potentiate the effects of other tranquilizers, narcotics, and barbiturates.
Appropriate reduction of the dosage of these agents should decrease potential problems.
Xylazine is contraindicated in animals with cardiac disease, respiratory disease, liver or kidney disease, shock, or general debilitation.
Lidocaine ( Xylocaine) is a fast-acting, short duration (one hour at most, unless combined with epinephrine) local anesthetic.
Mechanism of action - Local anesthetics block nerve conduction by preventing depolarization of fast sodium channels after repolarization. Epinephrine may prolong lidocaine’s effect; lidocaine with epinephrine should not be given locally in appendages because of the risk of excessive vasoconstriction, and it should not be given IV.
Indications/contraindications - Lidocaine is contraindicated in some cases of heart block. It is relatively contraindicated in animals with liver disease, hypovolemia or hypoxia. Overdose may cause neurologic signs and/or cardiac arrhythmias. The usual maximum dose is 4 mg/kg locally, regionally or epidurally. A simple way to use local anesthetics is to infiltrate each tissue plane of the incision site, and any body cavity that is opened. Local anesthetic techniques cause complete analgesia, and therefore are very useful in preemptive analgesia. Stinging associated with giving lidocaine to a conscious animal can be lessened by mixing it with sodium bicarbonate (1 part of
1 mol/l NaHCO3 to 9 parts of 1-2% lidocaine, mixed just before giving) or by warming the lidocaine to body temperature.
Bupivacaine (Marcaine) is a slower-acting, longer duration local anesthetic than lidocaine. Its onset of action is within 10 minutes, and its duration of action is generally 4-8 hours.
Mechanism of action - Local anesthetics block nerve conduction by preventing depolarization of fast sodium channels after repolarization.
Indications/contraindications - Bupivacaine is contraindicated in some cases of heart block. It is relatively contraindicated in animals with liver disease, hypovolemia or hypoxia. Cardiotoxicity is more likely with equivalent doses of bupivacaine than lidocaine, and overdose may cause ventricular arrythmias and cardiodepression. The usual maximum dose is 1mg/kg locally, regionally or epidurally. A simple way to use local anesthetics is to infiltrate each tissue plane of the incision site, and any body cavity that is opened. Local anesthetic techniques cause complete analgesia, and therefore are very useful in preemptive analgesia.
Diazapam (Valium) is a benzodiazepine compound with muscle relaxant and anticonvulsant activities in animals. Diazepam can be administered intramuscularly, intraperitoneally, and intravenously.
Mechanism of action - In animals, diazepam appears to act on parts of the limbic system, thalamus, and the hypothalamus to produce calming effects. It was found to reduce neural firing in the hippocampus, suggesting this location as a site of action. High affinity benzodiazepine receptors in the CNS have been found to be associated mainly with synaptic membranes. The major muscle relaxant actions may arise at the spinal, supraspinal, and neuromuscular synaptic sites, where GABA is the neurotransmitter.
Physiologic effects - In clinical doses, there is minimal respiratory and cardiac effects. The toxicity of diazepam is relatively low, with no acute hepatotoxic or nephrotoxic effects being apparent. Diazepam readily crosses the placenta and has an associated increased risk of congenital malformations when administered during early pregnancy. Also, it may increase cough reflex and laryngospasm. Diazepam has been used as an appetite stimulant in cats.
Indications/contraindications - Diazepam is an excellent preanesthetic agent for animals with a history of CNS disorders and to minimize CNS stimulation produced by ketamine.
Benzodiazepines have been combined with neuroleptanalgesics to increase the degree of sedation in laboratory animals. There is considerable species variation in degree of sedation produced by diazepam. In domestic pigs, non-human primates, rabbits, and rodents, sedative effects may be displayed (in contrast to dogs and cats where minimal sedation and even hyperexcitability may be produced). Benzodiazepines potentiate the effects of most anesthetics and narcotic analgesics. In contrast to the -water soluble benzodiazepine, midazolam, diazepam is prepared in organic solvents precluding its mixture with water soluble agents and perhaps producing longer duration of action.
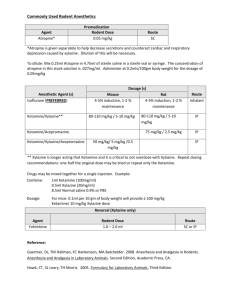
Injectable Anesthesia for Laboratory Animals
Drug
Ketamine:Xylazine
Mouse
80-120 mg/kg:10-16 mg/kg
IP (20-40 min. of anesthesia)
Rat
80-100 mg/kg: 5-10mg/kg
IP (20-50 min. of anesthesia)
Ketamine:Xylazine:
Acepromazine
50 mg/kg: 5 mg/kg: 1 mg/kg IP (30-45 minutes of anesthesia
Pentobarbital -variable anesthetic depth; poor analgesia
30-50 mg/kg IP (20-40 min. of anesthesia)
40-50 mg/kg IP (20-60 min. of anesthesia)
250 mg/kg IP (15-45 min. of anesthesia)
Tribromoethanol (Avertin)
See mixing instructions below.
275 mg/kg IP (30-50 min of anesthesia)
Atipamezole (for reversal of
Xylazine)
1.0 mg/kg IP 1.0 mg/kg IP
Dilutions of Injectable Anesthetic Mixtures for Use in Rodents:
MOUSE:
Ketamine/Xylazine (high dose)
Dosage: Ketamine
Xylazine
Dose Rate: 0.1 ml/10gm body weight IP*
120mg/kg
16.0 mg/kg
Volumes: Ketamine
Xylazine at 20 mg/ml**
WFI***
0.30 ml
0.20 ml
2.00ml
Total Volume 2.5 ml
*IP = intraperitoneal injection
**Xylazine in this mixture is at a concentration of 20 mg/ml. Xylazine is available in concentrations of 20 mg/ml and 100 mg/ml.
***WFI = water for injection. For controlled substance accountability, each ml contains 12 mg ketamine.
Tracking controlled substances (ketamine) – 1.2 mg per 10 gm body weight
Ketamine/Xylazine (low dose)
Dosage: Ketamine 80 mg/kg
Xylazine
Dose Rate: 0.13 ml/20 gm body weight IP*
10mg/kg
Volumes: Ketamine
Xylazine at 20 mg/ml**
0.30 ml
0.20 ml
WFI*** 2.00ml
Total Volume 2.5 ml
*IP = intraperitoneal injection
**Xylazine in this mixture is at a concentration of 20 mg/ml. Xylazine is available in concentrations of 20 mg/ml and 100 mg/ml.
***WFI = water for injection. For controlled substance accountability, each ml contains 12 mg ketamine.
Tracking controlled substances (ketamine) – 1.6 mg per 20 gm body weight
RAT:
Ketamine/Xylazine
Dosage: Ketamine
Xylazine
100 mg/kg
10mg/kg
Dose Rate: 0.2 ml/100 gm body weight IP or SC*
Volumes: Ketamine
Xylazine at 20 mg/ml**
WFI***
2.0 ml
1.0 ml
1.0 ml
Total Volume 4.0 ml
*IP or SC = Intraperitoneal or Subcutaneous
** Xylazine in this mixture is at a concentration of 20 mg/ml. Xylazine is available at concentrations of 20 mg/ml and 100 mg/ml. If using 100 mg/ml the volume of Xylazine would be 0.2 ml with a volume of 1.8 ml of WFI. The volume of Ketamine would remain the same.
***WFI = water for injection
Tracking controlled substances (ketamine) – 10 mg per 100 gm body weight
Avertin (tribromethyl alcohol and tertiary amyl alcohol): tribromethyl alcohol – light sensitive, stored under refrigeration tertiary amyl alcohol – explosive, store in safety cabinet
100% stock solution: mix 10g tribromethyl alcohol with 10 ml tertiary amyl alcohol
2.5% stock solution: mix 1:40 with water or isotonic saline
Mix under a fume hood. Gloves and a lab coat should be worn. Only containers marked for use in this procedure are to be used.
Storage - 4°C. Protect from light (wrap in foil or place in an amber bottle)
Dosage – 0.01 - 0.015 ml/gm of body weight or 0.375 mg/gm of body weight IP
Sterilize in a Nalgene 0.22 µm filter bottle and use fresh
Inhalant Anesthesia
Isoflurane is an inhalant anesthetic agent that produces rapid induction and recovery from anesthesia. The depth of anesthesia can be easily and rapidly altered. Virtually no metabolism occurs in the body because isoflurane is almost completely eliminated in expired air. Liver microsomal enzymes are minimally affected which results in little interference with drug metabolism or toxicology studies.
A scavenging system is important so that investigators are not exposed to the anesthetic vapors.
Fume hoods, negative suction to the outside or to activated carbon canisters work well. Carbon canisters must be weighed prior to initial use and periodically thereafter so that replacement of the canisters can be timely.
Isoflurane is best used with an anesthetic machine fitted with a precision vaporizer to deliver controlled amounts of anesthetic and oxygen. Anesthetic can be delivered to the animal via an induction chamber, facemask or endotracheal intubation.
Less desirable, isoflurane can be delivered on cotton balls or cotton gauze in a closed container.
Care should be taken to prevent the animal from coming in direct contact with the anesthetic.
This is most commonly done to anesthetize an animal prior to a procedure that will result in euthanasia such as perfusion. After the animal is anesthetized, it can be removed and a nosecone
(50 ml conical tube) used to maintain anesthesia. The nosecone is fitted with isoflurane-wetted cotton. This method should be done under a fume hood or negative pressure scavenging system.
Amphibian Anesthesia
Amphibians in the early stages of their life cycle (e.g., tadpoles) are entirely aquatic and have gills for respiration. Most amphibians lose their gills during metamorphosis and develop lungs.
Most importantly, amphibian skin acts as a semi-permeable membrane that allows for respiration
(cutaneous respiration) and absorption of substances through the skin.
Amphibians may be anesthetized by immersion in an anesthetic solution, placement in an anesthetic gas induction chamber or by anesthetic preparations applied to the skin.
Amphibians can remain out of water for long periods of time if they are kept moist.
Fasting for 12-24 hours prior to anesthesia is recommended to decrease the incidence of regurgitation which will foul the water of the anesthetic or recovery container.
Amphibians go through an excitement phase during anesthetic induction. It is important to induce anesthesia in a container that will prevent injury due to the animal jumping or falling out.
Induction
Decreased gular (throat skin)movement and diminished withdrawal reflex
Stages of anesthesia in amphibians
Light anesthesia
Loss of righting reflex and
Surgical anesthesia
No withdrawal reflex (toe absence of abdominal respirations pinch) and gular (throat skin) movements cease
Pulmonary respiration will cease during anesthesia in amphibians and can not be used to monitor anesthetic depth. Cutaneous respiration is sufficient to prevent clinical hypoxia during anesthesia.
Heart rate may be monitored during anesthesia by direct observation (ventral midline, caudal to the shoulders), ECG, ultrasonography or a Doppler flow detector. Normal values for heart rates have not been published.
MS-222 : Wide margin of safety. Solutions must be buffered with sodium bicarbonate to maintain neutral pH.
Tadpoles and newts 250-500 mg/l
Frogs and salamanders 1 g/l
Large specimens and toads 2-3 g/l
Benzocaine: Powder must be dissolved in ethanol to create a stock solution. Solutions must be buffered with sodium bicarbonate to maintain neutral pH. True toads, spadefoots and large salamanders – 2 gm/l
Isoflurane: May be mixed into a viscous solution with KY jelly and water or injected into an absorbant pad and applied directly to the dorsum of the animal. Applied to skin in patch or viscous gel.
Once the amphibian reaches the appropriate level of anesthesia for the procedures planned, the animal should be removed from the anesthetic bath and rinsed with fresh water or the topical preparation should be removed by rinsing. The animal will remain anesthetized for 10-80 minutes, depending on the method and drug concentration used.
Recovery from anesthesia (righting reflex returns and animal able to move normally) will take
30-90 minutes after the animal is rinsed with fresh water.
Do not raise the amphibian's body temperature above that of normal room temperature in an attempt to speed recovery. Increasing the body temperature will increase metabolism and oxygen requirements. Cutaneous respiration may not be sufficient to maintain adequate oxygenation.
Do not apply alcohol or other preparations that contain alcohol directly to the skin of an amphibian. It may be absorbed through the skin and may dissolve normal secretions that protect the animal from dehydration and infections.
For additional information regarding anesthetic use in amphibians please consult the following references.
1. Stetter MD: Fish and Amphibian Anesthesia. In Veterinary Clinics of North America: Exotic
Animal Practice 4(1), January 2001; pp. 69-82.
2. Green DE: Anesthesia of Amphibians in the Field. Amphibian Research and Monitoring
Initiative Standard Operating Procedure, March 2001. National Wildlife Health Center, United
States Geological Service.
3. Smith JM and Stump KC: Isoflurane Anesthesia in the African Clawed Frog ( Xenopus laevis). Contemporary Topics, 39(6), November 2000; pp. 39-42.
4. Wright KM and BR Whitaker: Amphibian Medicine and Captive Husbandry. 2001; pp. 115-
121. Krieger: Malabar, Florida.
Fish Anesthesia
When working with a new anesthetic protocol or species it is advisable to anesthetize a few fish and follow them through full recovery to insure drug dosages and techniques are safe and provide sufficient anesthetic depth for the intended procedures.
Fish are often fasted for 12-24 hours prior to anesthesia to reduce the risk of regurgitation of food that may lodge in the gills or foul the water. Fasting also decreases fecal contamination of water used for anesthesia and recovery.
Adequate oxygenation is necessary for maintenance of normal physiologic homeostasis during fish anesthesia. Oxygen should be supplied, via an air stone or similar device, to all water chambers used during transport, anesthesia and recovery.
Ideally, water taken from the original fish holding tank can be used in transport, anesthetic and recovery chambers. If water from another source is to be used, water quality parameters (i.e., chlorine, temperature, pH and ammonia) should closely duplicate that of the original holding tank.
Anesthetic Agent Dose Comments
MS-222 (tricaine methanesulfonate)
75-125 mg/l (induction) and
50-75 mg/l (maintenance)
Benzocaine hydrochloride 25-100 mg/l
Sodium bicarbonate should be added to stock solution to maintain neutral pH. Only
FDA approved anesthetic for fish (21 day withdrawal).
Sodium bicarbonate may need to be added to stock solution to maintain neutral pH. Small margin of safety between effective and lethal doses.
When a fish reaches the level of anesthesia sufficient to perform surgery, there is a total loss of equilibrium and muscle tone, decreased respiratory rate and no response to stimuli. A firm squeeze at the base of the tail may be used to determine response to stimuli.
Respiratory rate may be evaluated by observing movement of the operculum (rigid flap that covers the gills) as it opens and closes. Gill color should be dark pink to light red. If respirations become extremely slow or stop, the fish may be placed in anesthetic-free recovery water until respirations resume.
Water temperature should be maintained at the species normal optimum during both anesthesia and recovery.
For additional information regarding anesthetic use in fish please consult the following references:
1. Stetter MD: Fish and Amphibian Anesthesia. In Veterinary Clinics of North America: Exotic
Animal Practice 4(1), January 2001; pp. 69-82.
2. Burka JF, et al: Drugs in Salmonid Aquaculture - A Review. J. Vet Pharmacol. Therap. 20,
1997; pp. 333-349.
3. Bowser PR: Anesthetic Options for Fish. In Recent Advances in Veterinary Anesthesia and
Analgesia: Companion Animals, 2001. International Veterinary Information Service, Ithaca, NY.