chapter 17-the blood
advertisement
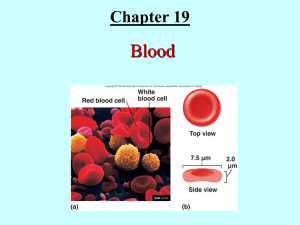
CHAPTER 17-BLOOD I. BLOOD A. Is the only fluid tissue in the human body. It contains living cells and fluid. B. Blood is pushed through the body by the pumping action of the heart. 1. Arteries-carry blood away from the heart. These branch until they become microscopic capillaries. Carbon dioxide and wastes can pass into capillaries by diffusion. Nutrients diffuse out of capillaries into body tissues. 2. Capillaries lead to Veins, which carry deoxygenated blood back to the heart. a. This blood is then pumped to the lungs where it picks up oxygen. The oxygenated blood is then returned to the heart for dispersal to the body. II. CHARACTERISTICS/FEATURES OF BLOOD A. It is classified as being a type of connective tissue since blood contains the 3 elements of connective tissue: 1. Cells 2. Matrix-the liquid portion of blood. 3. Fibers-mostly protein fibers such as fibrin. These provide support to blood. These also play a role in blood clotting. B. It has a salty, metallic taste. This is due to the presence of iron. C. Blood’s color depends on the amount of oxygen it is carrying. 1. Scarlet red blood is oxygen rich; whereas, dark red blood is low in oxygen. D. Blood has a greater density than water. E. Blood is slightly alkaline, with a pH between 7.35 and 7.45. F. It maintains a temperature around 100.4 degree F (38 degrees C). This is slightly higher than normal body temperature. G. Blood makes up about 8% of total body weight. H. Average blood volume is 5-6L in males and 4-5L in females. III. FUNCTIONS OF BLOOD A. Distribution-this includes: 1. Carrying oxygen from the lungs to body tissues. 2. Delivering nutrients and water to body tissues. 3. Transporting metabolic wastes from body tissues to sites of elimination. a. CO2 is carried to the lungs and nitrogen wastes to the kidneys. B. Regulation-The regulatory functions of blood include: 1. Maintaining normal body temperature a. Blood does this by absorbing and distributing heat throughout the body and to the skin where heat loss can occur. 2. Maintaining normal pH in body tissues a. Many blood proteins and solutes act as buffers. These buffers prevent sudden pH changes. b. Blood stores bicarbonate ions, which serve as the primary buffer in body tissues. C. Protection-this includes: 1. Preventing blood loss-platelets and blood proteins aid in clot formation which stops blood loss. 2. Fighting and preventing infection-antibodies and leukocytes are involved in fighting and preventing infection. IV. COMPOSITION OF BLOOD A. Blood is composed of 2 Primary Components: 1. Plasma-the liquid matrix of blood. 2. Formed Elements-blood cells and cell fragments. These are suspended in plasma. a. The Formed Elements in Human Blood: 1) Erythrocytes-red blood cells. 2) Leukocytes-white blood cells. 3) Thrombocytes-platelets. B. Blood is the most commonly examined tissue in the body. It is used to determine what illness a patient has. 1. In a lab, blood is spun in a centrifuge. This pushes the heavier formed elements to the bottom of the tube and the less dense plasma remains at the top. a. Erythrocytes settle at the bottom of the tube; thus producing a red mass at the base of the tube. Hematocrit-the percentage of erythrocytes to total blood volume. b. Buffy Coat-a thin, white layer at the top of the erythrocyte layer. The buffy coat contains leukocytes and platelets. c. Plasma-sits above the buffy coat and it makes up about 55% of blood volume. V. BLOOD PLASMA-the liquid portion of blood. A. Plasma is a straw-colored, sticky fluid. B. Plasma is Composed of: 1. Water-accounts for over 90% of total plasma volume. Water serves as a dissolving and suspending medium for blood solutes. a. Water is also involved in absorbing heat and heat transfers. 2. Plasma Proteins-account for 8% of total plasma volume. Plasma Proteins Include: a. Albumin-accounts for 60% of plasma proteins. 1) This protein is produced by the human liver. 2) Functions of Albumin include: a) Carrying some molecules through the body. b) Acting as a blood buffer. c) Creating osmotic pressure, which acts to maintain water balance between blood and tissues. b. Globulins-account for 36% of plasma proteins. 1) Types of Globulins in the Body: a) Alpha, Beta Globulins-produced by the liver. 1) These are transport proteins that attach to and transport lipids, metal ions and fat-soluble vitamins. b) Gamma Globulins-antibodies released primarily by plasma cells during an immune response. c) Clotting Proteins-make up 4% of plasma proteins. 1) This includes fibrinogen and prothrombin which are involved in blood clotting. Both of these proteins are produced in the liver. c. Metabolic enzymes d. Antibacterial proteins 3. Non-protein Nitrogenous Substances-this includes by-products of cellular metabolism such as lactic acid, urea, uric acid, creatinine and ammonium salts. 4. Nutrients-this includes materials absorbed in the digestive tract. Some of these materials include glucose and other simple sugars, amino acids, fatty acids, cholesterol and vitamins. 5. Electrolytes-this includes ions such as potassium, calcium, sodium and phosphate. a. Bicarbonate is also an electrolyte. Recall, that bicarbonate is a major buffer. b. Many electrolytes help maintain proper blood osmotic pressure. 6. Respiratory Gases-including oxygen and carbon dioxide. a. Most oxygen is bound to hemoglobin in erythrocytes. Some oxygen is dissolved in plasma. b. Carbon dioxide is transported attached to hemoglobin in erythrocytes and as bicarbonate dissolved in plasma. VI. FORMED ELEMENTS-cells and cell fragments in blood. A. 3 Formed Elements in Human Blood: 1. Erythrocytes 2. Leukocytes 3. Thrombocytes B. Erythrocytes-Red Blood Cells 1. Erythrocytes are small (7.5 micrometers in diameter), biconcave discs with depressed centers. 2. Cellular Structure of Erythrocytes: a. Are bound by a true cellular membrane. b. They lack a nucleus and they do not contain cellular organelles. Why is this? c. Erythrocytes contain Hemoglobin (Hb). What is this compound? 3. Erythrocytes contribute greatly to blood viscosity. a. Women contain 4.3-5.2 million cells per mm3 and Men contain 5.1-5.8 cells per mm3. This leads to about 2.5 trillion erythrocytes in a healthy adult. b. An increase in erythrocyte number increases blood viscosity; thus, blood flow slows. The opposite is true as well. 4. Erythrocytes transport oxygen and carbon dioxide through the body. Much of the oxygen is carried by hemoglobin which is stored in erythrocytes. 5. Hemoglobin-transports most of the oxygen through the body. It can also carry carbon dioxide. a. Males usually contain 13-18 g of hemoglobin per 100 ml of blood; females contain slightly less than this. b. Hemoglobin is composed of: 1) Globin-a complex protein. 2) Heme-a ring-shaped structure that binds to the globin molecule. a) There are 4 heme groups in every hemoglobin molecule. b) Each of the heme groups contains an iron atom. 1) Iron easily combines with oxygen. Therefore, each hemoglobin molecule can transport 4 oxygen molecules. c) A single red blood cell contains 250 million hemoglobin molecules, so each erythrocyte can carry about 1 billion oxygen molecules. c. Hemoglobin picks up oxygen in the lungs. 1) The oxygen is then transported to body tissues where it is released for use by tissue cells. 2) When oxygen binds to iron, the hemoglobin is known as oxyhemoglobin. The oxygen changes the shape of hemoglobin which now becomes bright red. 3) When oxygen releases from iron, hemoglobin returns to its original shape. At this point, the hemoglobin is known as deoxyhemoglobin and it becomes dark red in color. d. About 20% of the carbon dioxide transported in blood combines with hemoglobin. Carbon dioxide attaches to the globin portion of hemoglobin to form carbaminohemoglobin. 1) Carbon dioxide uptake occurs in body tissues. a) The carbon dioxide is carried to the lungs where it is eliminated from the body. 6. Erythrocyte Production a. Hemopoiesis/Hematopoiesis-blood cell formation. 1) This occurs in red bone marrow. Recall that red bone marrow is in irregular bones and in the epiphyses of long bones. b. Erythropoiesis-red blood cell formation. Erythrocytes do not have the ability to divide. c. Hemocytoblasts (Hematopoietic Stem Cells)-located in red bone marrow. 1) These mature into all types of blood cells. 2) Once these start developing into a particular type of blood cell, they cannot stop. d. Events in Erythropoiesis 1) Hemocytoblasts develop into myeloid stem cells which are then transformed into proerythroblasts. 2) The proerythroblasts then develop into erythroblasts. 3) Erythroblasts produce huge numbers of ribosomes which are involved in protein production. a) Hemoglobin formation and iron accumulation also occurs in the erythroblast. 4) Next, the erythroblast develops into a normoblast. a) A normoblast begins to turn pink-red in color as more hemoglobin is produced. A normoblast also loses all cellular organelles. It also begins to assume the typical biconcave shape. 5) Normoblasts develop into reticulocytes which are essentially young erythrocytes. Reticulocytes enter the bloodstream to begin transporting oxygen and carbon dioxide. Reticulocytes become mature erythrocytes within about two days. a) Reticulocytes account for 2-3% of all erythrocytes in a healthy human. b) Reticulocyte counts are used clinically as an index of the rate of erythrocyte formation. e. The body must maintain a constant number of erythrocytes. 1) Too few erythrocytes can lead to hypoxia (oxygen deprivation) and too many erythrocytes increases blood viscosity. 2) Healthy individuals produce about 2 million new erythrocytes every second. f. Hormonal Control of Erythropoiesis: 1) Erythropoietin (EPO)-hormone produced primarily by the kidneys. a) Some can be produced by the liver. b) This hormone directly regulates erythropoiesis. c) When cells in the kidney become hypoxic, they increase their erythropoietin production. What causes this hypoxia? 1) Reduced number of erythrocytes due to blood loss. 2) Reduced oxygen availability. 3) Increased tissue demand for oxygen-as would occur during exercise. d) Excess oxygen in the bloodstream or too many erythrocytes depresses erythropoietin production. e) Oxygen availability regulates erythropoietin production-not the number of erythrocytes. f) Renal dialysis patients are often given genetically engineered erythropoietin to regulate erythrocyte formation. 1) Some athletes have illegally used this product to improve their stamina and performance; however, this may increase blood viscosity and lead to dehydration. g. Dietary Requirements for Erythopoiesis: 1) Iron-needed for hemoglobin production. Free iron is toxic in the body, so iron is stored in other forms (ferritin or hemosiderin). 2) B Complex Vitamins-including B12 and folic acid. 7. Erythrocyte destruction and removal a. Since erythrocytes cannot divide, they become old and lose their ability to carry oxygen. They have a useful life span of about 120 days. b. Old erythrocytes are often trapped in the spleen where they are destroyed by macrophages. 1) The heme is pulled off of globin. The iron in the heme is stored in the body for future use. The remainder of the heme molecule is broken down into bilirubin which is a yellow pigment that leaves the body via feces. 2) The globin portion of hemoglobin is broken down into amino acids that are used by the body to produce other proteins. This is an example of internal recycling. 8. Erythrocyte Disorders: a. Anemias-condition in which the blood has an abnormally low oxygencarrying capacity. In anemia, blood oxygen levels are inadequate to support normal metabolism. 1) Characteristics of anemia include shortness of breath, pale skin, fatigue. 2) Causes of Anemia: a) Insufficient Numbers of Erythrocyte-caused by blood loss, bone marrow failure and erythrocyte destruction. 1) Hemorrhagic anemias-result from blood loss. 2) Hemolytic anemias-erythrocytes rupture prematurely. Some infections cause this. 3) Aplastic anemia-results from damage to bone marrow. b) Decreased Hemoglobin Content-often results from poor nutrition. 1) Iron-deficiency anemia-low iron content. 2) Pernicious anemia-caused by a vitamin B-12 deficiency. c) Abnormal Hemoglobin-usually genetic in nature. 3 Examples of this include: 1) Thalassemias-occur when one of the globin chains is faulty or absent. 2) Sickle-cell anemia-occurs when erythrocytes are sickle-shaped. These blood cells rupture easily; thus, reducing their capacity to carry oxygen. Is often treated with a blood transfusion. 3) Polycythemia-an abnormally high number of erythrocytes. This increases blood viscosity which causes the blood to flow sluggishly. a) Polycythemia vera-common in patients who have bone marrow cancer. The erythrocyte count is exceptionally high. b) Severe polycythemia is treated by blood dilution-that is, removing some blood and replacing it with saline. C. Leukocytes-white blood cells. 1. General Features of Leukocytes: a. They are complete cells-leukocytes contain a nucleus and organelles. b. They can divide to reproduce. c. On average, there are 4000-11,000 leukocytes per mm3 of blood. They account for less than 1% of total blood volume. d. Leukocytes help fight disease and they protect us from damage by bacteria, viruses, parasites, toxins and tumor cells. 1) To carry out this function, leukocytes can leave capillaries and enter tissues (a process known as diapedesis). Leukocytes move through tissues by amoeboid motion. a) Leukocytes can follow chemical trails secreted by damaged cells. This is known as positive chemotaxis. b) Whenever an infection occurs, the body increases its leukocyte production. Leukocytosis-a leukocyte count greater than 11,000 cells per mm3. This is common during bacterial and viral infection. 2. Leukocytes are Classified into 2 Major Categories a. Granulocytes-contain membrane-bound cytoplasmic granules. b. Agranulocytes-do not contain membrane-bound cytoplasmic granules. 3. Granulocytes a. Characteristics: 1) Are spherical in shape and contain lobed nuclei. 2) Stain with Wright’s Stain. 3) All granulocytes are phagocytic. b. Types of Granulocytes: 1) Neutrophils-most numerous leukocyte in the body. a) Are twice as large as erythrocytes. b) Are referred to as neutrophils because their granules take up basic (blue) and acidic (red) dyes. c) Their granules have a lilac color. d) The granules of neutrophils contain defensins which are antibiotic type proteins and enzymes. e) Neutrophil nuclei contain 3 to 6 lobes. f) Neutrophils are chemically attracted to sites of inflammation. g) Neutrophils are involved in: 1) Attacking bacteria and fungi via phagocytosis. 2) Producing defensins which “spear” bacteria. 3) Using oxygen to produce hydrogen peroxide which kills bacteria. h) Neutrophil numbers increase greatly during bacterial infection. 2) Eosinophils-account for 1-4% of all leukocytes and are similar in size to neutrophils. a) Their nuclei stain red and they contain 2 lobes that are connected by a thin band of nuclear material. b) Eosinophils contain large granules that are filled with a variety of digestive enzymes. c) Functions of Eosinophils: 1) Fight parasitic worms (roundworms, flatworms). a) Eosinophils accomplish this by secreting enzymes that digest the covering around the worm. 2) Inactivate/phagocytize chemicals or molecules that lead to allergies. 3) Basophils-account for 0.5% of all leukocytes (are the rarest of all leukocytes). They are similar in size to neutrophils. a) They contain large granules that stain purple to black. b) Their granules contain histamine. 1) Histamine acts as a vasodilator during an inflammatory response. Histamine also attracts leukocytes to an inflamed site. c) The nucleus of basophils is generally U or S-shaped with two or three constrictions. 4. Agranulocytes a. Characteristics 1) These lack visable cytoplasmic granules. 2) Their nuclei are spherical or kidney shaped. b. Types of Agranulocytes 1) Lymphocytes-2nd most abundant type of leukocyte. a) They have a large nucleus that stains deep purple. 1) The nucleus almost fills the entire cell. b) Most lymphocytes are found in lymphoid tissues (such as the spleen and lymph nodes). Only a few lymphocytes are actually in the bloodstream. c) Types of Lymphocytes: 1) T Lymphocytes-involved in immune responses. Specifically, T lymphocytes act directly against viruses and tumor cells. 2) B Lymphocytes-give rise to plasma cells which can produce antibodies that are released into the blood. 2) Monocytes-account for 4-8% of all leukocytes in the body. a) Their nucleus stains dark purple and it has a distinct U or kidney shape. b) Monocytes can differentiate into Macrophages which are phagocytic cells on viruses and bacteria. 5. Leukopoiesis-production of leukocytes. a. This process is regulated by hormones known as colony-stimulating factors (CSF’s). These stimulate the formation of new leukocytes. Can be given to some patients in an effort to increase the functioning of the immune system. b. Granulocyte Formation: 1) Hemocytoblast Myeloid Stem Cell Myeloblast Precursor cells Neutrophils Eosinophils Basophils c. Agranulocyte Formation 1) Hemocytoblast ↓ Myeloid Stem Cell ↓ Monoblast ↓ Monocyte Lymphoid Stem Cell ↓ Lymphoblast ↓ Lymphocyte ↓ Plasma Cells 6. Leukocyte disorders: a. Leukopenia-abnormally low white blood cell count. This can be induced by some drugs (such as steroids) and cancer treatments. b. Leukemia-refers to a group of cancerous conditions involving leukocytes. 1) Normally, the leukocytes remain unspecialized and impair bone marrow function. 2) Treatments include radiation, drug therapy, bone marrow transplants. 3) Leukemias are often named for the type of cell that is involved. c. Infectious mononucleosis-caused by the Epstein-Barr virus. 1) Signs/Symptoms include: fatigue, aches, sore throat, low-grade fever 2) Characterized by an excessive number of agranulocytes. 3) There is no cure at present-it usually runs its course in a few weeks. D. Thrombocytes (Platelets)-are cell fragments, not true cells. 1. Platelets contain many small, purple-staining granules. a. These granules contain chemicals that are involved in blood clotting. The chemicals include:serotonin, Ca+, ATP, enzymes, clot factors. 2. Platelets begin forming clots when blood vessels are broken. They stick to the damaged site to form a plug which stops blood loss. 3. They live for only about 10 days if they are not involved in clot formation. 4. Platelet formation-is regulated by the hormone thrombopoietin. a. Steps in this process: 1) Hemocytoblast Megakaryoblast Megakaryocyte Fragments to form thrombocytes VII. HEMOSTASIS-“stoppage of bleeding” A. This is the process of clot formation. Hemostasis prevents blood loss. This is a rapid, localized response to damaged blood vessels. B. 3 Phases in Hemostasis: 1. Vascular spasm 2. Platelet plug formation 3. Coagulation (blood clotting) C. Events in Hemostasis: 1. Vascular Spasm a. Immediately after an injury, damaged blood vessels constrict (vasoconstrict). b. This constriction is known as vascular spasm. Vascular spasm is an attempt to reduce blood loss so that platelet plug formation and blood clotting can occur. c. Factors that lead to vascular spasm: 1) Injury to vascular smooth muscle 2) Chemicals released by endothelial cells of blood vessels 3) Platelets 4) Reflexes associated with pain receptors. 2. Platelet Plug Formation a. Platelets form a plug that temporarily seals the break in the vessel wall. b. Normally, platelets do not stick together. However this changes when a blood vessel is broken. When a blood vessel is damaged, underlying collagen fibers are exposed. This forces platelets to undergo the following changes: 1) Platelets swell and from spiked processes. 2) Platelets become sticky and attach to the exposed collagen. 3) Once attached, the platelets begin to release: a) Serotonin-enhances vascular spasm. b) Adenosine diphosphate-attracts more platelets to the injury site. (ADP). 4) Within minutes a platelet plug is formed. 5) Prostacyclin-produced by endothelial cells. This chemical prevents platelets from attaching to each other outside the injury site. 6) Finally, the platelet plug is reinforced with fibrin (protein) threads. 3. Coagulation-blood clotting; occurs when blood is converted from a liquid to a gel. a) Coagulation occurs through 3 distinct phases: 1) Phase 1-Formation of Prothrombin Activator-can occur through 1 of 2 pathways: a) Intrinsic Pathway-occurs immediately after an injury. 1) Is a very slow process and it involves several intermediate compounds. b) Extrinsic Pathway-is initiated by a compound known as tissue thromboplastin(which is released by damaged cells). 2) Phase II-Prothrombin activator converts prothrombin into thrombin a) Prothrombin activator converts the protein prothrombin into the active enzyme thrombin. 3) Phase III-Formation of the Fibrin mesh a) Thrombin (from above) converts the protein fibrinogen into long protein threads known as fibrin. b) Fibrin-a long, fibrous protein. 1) Fibrin threads function by: a) Providing a surface for platelets to attach to. This helps form the bulk of a clot. b) Forcing plasma to become gel-like. This traps formed elements and other blood components. b) Clot Retraction and Repair 1) Clot retraction helps to stabilize newly formed clots. 2) Platelets contain the contractile proteins actin and myosin. a) These two proteins contract and pull on the fibrin threads. b) This tightening pulls broken blood vessels closer together and it forces serum (plasma) from the forming clot. c) Fibrinolysis-process that removes unneeded blood clots when healing has occurred. This process also helps to remove small clots that form in blood vessels. This is an important process for body homeostasis. 1) Plasmin-enzyme that can digest blood clots. It is activated by the protein plasminogen which is in all clots. 2) Fibrinolysis begins about 2 days after clot formation. d) Several mechanisms in the body prevent clots from becoming too large. These include: 1) Removal of clot factors by the body 2) Absorption of thrombin by the body (slows clot formation) 3) Heparin-anticoagulant contained in the granules of basophils and mast cells. Heparin inhibits the activity of thrombin. D. Disorders of Hemostasis-can be classified into 2 Major Categories: 1. Thromboembolytic conditions-these result from conditions that cause undesirable clot formation. a. Thrombus-clot that develops and persists in an unbroken blood vessel. 1) A large thrombus may block circulation, causing blockage or death. b. Embolus-a free floating molecule in the blood. A thrombus can break apart to form an embolus. The embolus can form an embolism when the molecule reaches a blood vessel that is to small for passage. 1) Problems arise when an embolus reaches a blood vessel that is too narrow for the embolus to pass through. Again, this is deadly. 2) Heparin, Coumadin and aspirin can serve as anticoagulants. 2. Bleeding disorders-occur when clotting is affected. Examples include: a. Thrombocytopenia-condition in which the number of circulating platelets is deficient. This can cause widespread hemorrhage. This often results from bone marrow damage. Small purple patches on the skin are a sign of this. Typically, a platelet count less than 50,000/mm3 is used to diagnose this. b. Hemophilia-this refers to several disorders in which the blood does not clot properly. In most cases, it is the result of a deficiency of clot factors. It is genetic in nature. Hemophilia is treated with transfusions of plasma and clot factors. VIII. TRANSFUSION AND BLOOD REPLACEMENT A. A loss of 30% of blood volume can be fatal. Transfusions are now done to prevent problems when blood is lost. B. Human erythrocytes are covered by special identity proteins. 1. Humans must be given blood that contains similar proteins to their own. If blood is detected as being foreign, then the transfused cells will agglutinate (clump) and be destroyed. C. ABO Blood Groups 1. Agglutinogens-proteins found on the cell membranes of erythrocytes. These can lead to immune responses. Human blood groups are based on the presence/absence of two agglutinogens (A and B). 2. Agglutinins-preformed antibodies in human blood. These act against erythrocytes carrying agglutinogens that are not present on a person’s own erythrocytes. 3. Human Blood Type Agglutinogen Agglutinins Type A A b Type B B a Type O None a and b Type AB A and B None 4. Type AB individuals-do not produce agglutinins; therefore, they can receive blood from anyone-safely. They are known as Universal Recipients. 5. Type O Individuals-do not contain agglutinogens; therefore, their blood will not cause an immune response. They are known as Universal Donors for this reason. D. Rh Blood Groups 1. Rh Factors-Rh agglutinogens (are at least 8 of these). This is named for the Rhesus monkey (where it was first discovered). a. Most Americans are Rh+-they contain the Rh antigen. 2. If an Rh negative person is given Rh+ blood; they will begin to produce Rh antibodies. a. However, a transfusion reaction does not occur in the first event. Reactions occur in later events when Rh+ blood is given to the Rh- person. 3. Problems can arise when a pregnant Rh- mother is carrying an Rh+ baby. In this case, Rh+ agglutinogens will pass into the mother’s bloodstream via the placenta. The mother will then build antibodies against the Rh+ blood. This does not harm the first pregnancy; however, if the same situation develops again, problems can arise. a. In this case, a second baby can become anemic and hypoxic. Brain damage and even death can occur. This is known as Hemolytic Disease of the Newborn or Erythroblastosis fetalis. This is treated with RhoGAM which prevents an immune response by the mother. E. Transfusion Reactions-occurs from mismatched blood. In these, foreign erythrocytes clump (agglutinate). This is treatable. F. Blood Typing-is done by adding a or b agglutinins to a blood sample. G. Specific Tests on Blood Samples: 1. Microscopic studies-to observe shape/size of erythrocytes. 2. Differential White Blood Cell Count-to determine what type of infection a person has. 3. Complete Blood Count-gives full blood chemistry. 4. Platelet count IX. RELATED CLINICAL TERMS-Know the following: A. Blood chemistry tests B. Blood fraction C. Bone marrow biopsy D. Exchange transfusion E. Hematology F. Hematoma G. Hemochromatosis H. Plasmapheresis I. Septicemia