Plasma-Based (Leumeta TM )
advertisement
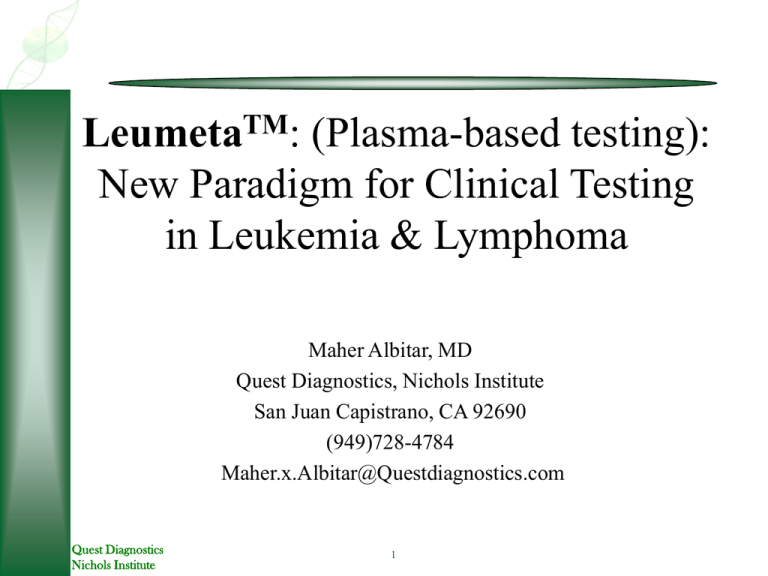
LeumetaTM: (Plasma-based testing): New Paradigm for Clinical Testing in Leukemia & Lymphoma Maher Albitar, MD Quest Diagnostics, Nichols Institute San Juan Capistrano, CA 92690 (949)728-4784 Maher.x.Albitar@Questdiagnostics.com Quest Diagnostics Nichols Institute 1 Cancer is Not a Physiologic Process •High uncontrolled proliferation rate •High relative turnover of cells •Heterogeneity within the tumor cells Quest Diagnostics Nichols Institute 2 Circulating Cellular Debris Contains Fingerprints of Tumor Cells Plasma Quest Diagnostics Nichols Institute 3 Hypothesis •Plasma (or serum) contains the “fingerprints” of cancer cells •Plasma (or serum) is enriched by tumorspecific DNA, RNA and cellular proteins. •Every cell-based test can also be performed using plasma (LeumetaTM). Quest Diagnostics Nichols Institute 4 Why Hematologic Diseases? •Neoplastic cells “swim” in plasma/serum. •Hematologic diseases can be patchy •Reticuloendothlial system is frequently damaged in hematologic diseases Quest Diagnostics Nichols Institute 5 Example of Heterogeneity in Bone Marrow in a Patients with CML Quest Diagnostics Nichols Institute 6 Marrow Fibrosis and Poor Aspiration Quest Diagnostics Nichols Institute 7 Plasma-Based (LeumetaTM ) DNA Tests •Mutations •Chromosomal translocations •Chromosomal aberrations (deletions, amplification) •Minimal Residual disease Quest Diagnostics Nichols Institute 8 Plasma is More Sensitive in Detecting JAK2 Mutation and Homozygous/Hemizygous Patients Patient #1 Forward Cells Reverse Forward Plasma Reverse Quest Diagnostics Nichols Institute 9 Patient #2 Patients with Homozygous/Hemizygous JAK2 as Detected Using Plasma Have More Aggressive Disease Blas ts <20% Cumulative Proportion Surviving 1.0 0.9 0.8 0.7 P=0.05 0.6 0.5 P=0.5 0.4 He t JAK2 M utant (n=23) 0.3 He m i/hom ozygous JAK2 M utant (n=19) 0.2 Unm utate d (n=42) 0.1 0.0 0 26 52 78 104 130 156 182 208 234 260 286 312 338 Wee k s Quest Diagnostics Nichols Institute 10 Plasma is More Sensitive than Cells in Detecting TP53 Mutations Quest Diagnostics Nichols Institute 11 Plasma is More Sensitive in Detecting Ras Oncogene Mutations Quest Diagnostics Nichols Institute 12 Detection of 5q Deletion in the Plasma of a Patients with AML Using LOH Quest Diagnostics Nichols Institute 13 Plasma is more Sensitive than Peripheral Blood Cells in Detecting NPM1 Mutations in AML Quest Diagnostics Nichols Institute 14 Plasma-Based (LeumetaTM ) RNA Tests •Mutations •Chromosomal translocations •Expression and quantification •Minimal Residual disease Quest Diagnostics Nichols Institute 15 Plasma is More Sensitive than Cells in Detecting ABL Kinase Mutations 931T>C (F311L) 758A>T (Y253F) F PB R F BM R F Plasma R Quest Diagnostics Nichols Institute 16 944C>T (T315I) Plasma is More Sensitive in Detecting T315I Mutation Using ASO Assay Quest Diagnostics Nichols Institute ID TYPE SEQ.RESULT % Mut of total 1003 PB Wt 0 1003P 1004 PLASMA BM Wt Wt 15 3 992P PLASMA Mut (T) 100 992 991 CELL BM C/T C/T 53 61 17 Plasma is More Sensitive in Monitoring BCR-ABL Transcript in Patients with CML BCR-ABL: ABL Ratio (Log) 10 1 0.1 0.01 0.001 1e -4 Ce lls Plasma 1e -5 Bas e line Quest Diagnostics Nichols Institute 3 M onths 6 M onths 9 M onths 12 M onths 18 Plasma-Based (LeumetaTM ) Protein Tests •Protein levels •Phosphorylation and modification •Enzymatic activity •Tumor markers •Diagnosis and classification Quest Diagnostics Nichols Institute 19 Membrane Attachment of CD20 and CD52 CD52 GPI Anchor CD20 N Quest Diagnostics Nichols Institute Carbohydrate C 20 High levels of cCD20 in NHL but not in Hodgkin’s Disease Pre-therapy 1100 ±1.96*Std. Err. ±1.00*Std. Err. Mean 900 cCD20 (nM/L) P<0.0001 700 500 300 100 HD (37) Quest Diagnostics Nichols Institute NHL (65) 21 Normal (15) High Levels of cCD52 in NHL but not in Hodgkin’s Disease Pre-therapy 360 ±1.96*Std. Err. ±1.00*Std. Err. Mean 300 P<0.0001 cCD52 (nM/L) 240 180 120 60 0 HD (37) Quest Diagnostics Nichols Institute NHL (65) 22 Normal (15) 0.8 0.6 0.4 0.2 Probability of Survival 1.0 Shorter Survival in Patients with Lymphoma and High Levels of cCD20 0.0 sCD20 M/ml Pat. <= 424.8 26 > 424.8 39 p-value = 0.008 0 Quest Diagnostics Nichols Institute 50 100 23 Died 14 32 150 Time (months) 200 0.6 0.4 Low b2m, Low CD52 Low b2m, High CD52 High b2m, Low CD52 High b2m, High CD52 0.2 Probability of Survival 0.8 1.0 Levels of cCD52 (23n Cut-off) and b2M (3.5 cut-off) Are Useful in Stratifying Patients with CLL 0.0 p-value=<0.0001 0 1 2 3 Time (years) Quest Diagnostics Nichols Institute 24 4 High Levels of cCD20 in CLL Correlate with Short Survival 1.0 Cumulative Proportion Surviving 0.9 0.8 0.7 0.6 0.5 cCD20 (nM/L) <1875 0.4 0.3 Pts 149 Died 30 >1875 19 P=0.01 7 0.2 0.1 0.0 0 10 20 30 Months Quest Diagnostics Nichols Institute 25 40 50 60 70 Cell-Free Circulating Stem Cell Marker (CD34) in Patients with Leukemia cCD34 in AM L and M DS Cumulative Proportion Surviving 1.0 0.9 cCD34(U/ul) Pats. Died <10845 71 24 0.8 >10845 68 P=0.01 0.7 35 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 16 32 48 64 80 96 112 128 144 160 176 192 208 We e k s Quest Diagnostics Nichols Institute 26 Cell-Free Circulating CD4 as a Biomarker in Patients with Myelodysplastic Syndrome cCD4 in M DS Cumulative Proportion Surviving 1.0 0.9 cCD4 (U/ul) Pats. Died <1029 19 13 0.8 >1029 25 P=0.04 0.7 11 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 16 32 48 64 80 96 112 128 144 160 176 192 208 We e k s Quest Diagnostics Nichols Institute 27 Plasma Proteasome Activity as a Biomarker in Patients with Acute Myeloid Leukemia 1.2 p = 0.002 1 Censored Casp >= 2.4 Probability 0.8 Casp < 2.4 0.6 0.4 E/N=65/94 0.2 E/N=80/94 0 0 Quest Diagnostics Nichols Institute 100 200 Tim e of follow -up (w eeks) 28 300 400 Plasma BCR-ABL Protein in Patients with CML (Pre-Rx) BCR-ABL levels in Previously Untreated CML Patients A 2.6e6 2.4e6 2.2e6 Mol/10 ul Plasma (100 beads) 2e6 1.8e6 1.6e6 1.4e6 1.2e6 1e6 8e5 6e5 4e5 2e5 0 0 2 1 Quest Diagnostics Nichols Institute 4 3 6 5 8 7 9 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44 46 48 50 52 54 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 29 Plasma Levels of Phospho-BCR-ABL Protein in Patients with CML (Pre-Rx) B Thr(735) and Tyr(245) phosphorylation in previously untreated CML Patients 2.4 Phospho:Total BCR-ABL Ratio 2.0 Phospho-Thr(735):BCR-ABL Ratio Phospho-Tyr(245):BCR-ABL Ratio 1.6 1.2 0.8 0.4 0.0 0 2 1 Quest Diagnostics Nichols Institute 4 3 6 5 8 7 9 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44 46 48 50 52 54 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 30 Currently Available Leumeta Tests Plasma Cells 16031X/ 16029X abl Kinase Domain Mutation in CML 17679X/ 14991X t(11;14) bcl-1/JH(MCL) Real Time PCR 17690X/ 15007X t(14;18) bcl-2/JH Real Time PCR 17702X/ 15480X IgVH Mutation Analysis 16101X/ 16102X JAK2 Mutation (V617F) 16104X/ 16106X c-kit Mutation Analysis 16119X/ 14868X B-cell gene rearrangement, Qual., PCR 16118X/ 16005X B-cell gene rearrangement, Quant., PCR 16127X/ 16128X ras Mutation Analysis, Plasma-based, 17862X/ 15930X T-Cell Receptor (TCR) Gene Rearrangement, Qualitative PCR 17861X/ 16025X T-Cell Receptor (TCR) Gene Rearrangement, Quantitative PCR 17853X/ 15052X bcr/abl Gene Rearrangement, Quantitative PCR, Plasma-based 19783X/ 19782X ABL T3151 Mutation in CML 16159X/ 16158X NPM(Exon 12) Mutation Analysis Quest Diagnostics Nichols Institute 31 Leumeta™ - Summary New Paradigm in Testing • Plasma contains the fingerprint of tumor cell (Leukemia/lymphoma) • Plasma is frequently more sensitive than cell samples (less dilution by normal cells). • Plasma-based testing reduce the need for biopsies • Most of Plasma-based assays are quantitative, easier to standardize and more objective. • There is a need for the development of more plasma-based tests to more significantly reduce the need for biopsies. Quest Diagnostics Nichols Institute 32 References 1.Manshouri T, Do KA, Wang X et al. Circulating CD20 is detectable in the plasma of patients with chronic lymphocytic leukemia and is of prognostic significance. Blood. 101(7), 2507-2513 (2003). 2.Giles FJ, Vose JM, Do KA et al. Circulating CD20 and CD52 in patients with non-Hodgkin's lymphoma or Hodgkin's disease. Br J Haematol. 123(5), 850-857 (2003). 3.Albitar M, Do KA, Johnson MM et al. Free circulating soluble CD52 as a tumor marker in chronic lymphocytic leukemia and its implication in therapy with anti-CD52 antibodies. Cancer. 101(5), 999-1008 (2004). 4.Jilani I, Kantarjian H, Faraji H et al. Measurement of free circulating Bcr-Abl fusion protein and its phosphorylation in patients with chronic myeloid leukemia. Blood. abstract 2006. 5.Rogers A, Joe Y, Dey A et al. Relative increase in leukemia-specific DNA in peripheral blood plasma from patients with acute myeloid leukemia and myelodysplasia. Blood. 103(7), 2799-2801 (2004). 6.Ahmed M, Giles F, Joe Y et al. Use of plasma DNA in detection of loss of heterozygosity in patients with multiple myeloma. Eur J Haematol. 71(3), 174-178 (2003). 7.Ma W, Kantarjian H, Verstovsek S et al. Hemizygous/homozygous and heterozygous JAK2 mutation detected in plasma of patients with myeloproliferative diseases: correlation with clinical behaviour. Br J Haematol. 134(3), 341-343 (2006). 8.Ma W, Tseng R, Gorre M et al. Plasma RNA as an alternative to cells for monitoring molecular response in patients with chronic myeloid leukemia. Haematologica. 92(2), 170-175 (2007). 9.Ma W, Kantarjian H, Jilani I et al. Heterogeneity in detecting Abl kinase mutations and better sensitivity using circulating plasma RNA. Leukemia. 20(11), 1989-1991 (2006). 10.Ma W, Jilani I, Gorre M et al. Plasma as a source of mRNA for determining IgVH mutation status in patients with chronic lymphocytic leukaemia. Br J Haematol. 133(6), 690-692 (2006). Quest Diagnostics Nichols Institute 33