safety - TB CARE I
advertisement

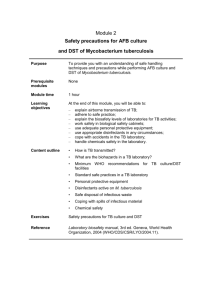
Module 2 Safety precautions for AFB culture and DST of M. tuberculosis 1 Learning objectives At the end of this module, you will be able to: explain airborne transmission of TB; adhere to safe practice; explain the biosafety levels of laboratories for TB activities; work safely in biological safety cabinets; use adequate protective personal equipment; use appropriate disinfectants; cope with accidents in the TB laboratory; handle chemicals safely in the laboratory . 2 Content outline • • • • • • • • • Transmission of TB Biohazards in a TB laboratory Minimum WHO recommendations for TB culture / DST facilities Standard safe practice in a TB laboratory Personal protective equipment Disinfectants active against M. tuberculosis Safe disposal of infectious waste Coping with accidents Chemical safety 3 Transmission of tuberculosis Mycobacterium tuberculosis is almost always transmitted by patients with active pulmonary disease: • • • • TB patient expels bacilli in small droplets of respiratory secretions. Secretions quickly evaporate leaving “droplet nuclei” less than 5 μm in diameter. Droplet nuclei of this size, containing 1–3 bacilli, can remain suspended in the air. Following inhalation, droplet nuclei are able to reach deep into the lungs to produce infection. 4 Aerosol formation: spread of droplets Coughing Sneezing Talking Singing 5 Specimens must be collected outside the laboratory 6 Biohazards in the laboratory: be aware! • • • Inhalation hazards: handling of liquids containing TB bacill generates infectious aerosols: – pipetting – working with loops – centrifugation – opening tubes – vortexing suspensions Ingestion hazards Inoculation hazards 7 Importance of laboratory safety for preventing laboratory-acquired infection 8 Conclusion of the survey: •DST is associated with the higher risk. •Smear microscopy alone does not pose a higher risk than clerical work. 9 Medical fitness of laboratory staff • In accordance with national laws and practices, health surveillance of TB laboratory workers should be performed: – before enrolment in the TB laboratory; – at regular intervals thereafter; – after any biohazard incident. • Workers should be educated about the symptoms of TB and provided with ready access to free medical care if symptoms arise. • Confidential HIV counselling and testing should be offered. Reassignment of HIV-positive workers away from high-risk environments should be considered. [to be adjusted to local policy] 10 Biological safety cabinet The biological safety cabinet, or BSC, is the single most important equipment for containing and quickly eliminating infectious aerosols generated during culture/DST procedures. For proper functioning, the BSC must be well maintained. 11 HEPA filter • HEPA = high-efficiency particulate air. • Traps and removes 99.97% of airborne particles equal to or larger than 0.3 µm in diameter. • Evaluation of the performance of the HEPA filter and regular maintenance of the BSC are critical for protection 12 Work in a BSC BSC work zone should be divided into three areas to minimize contamination over items: – a clean area: supplies; – working area: specimen; – contaminated area: waste container. 13 Work in a BSC • Organize a realistic workload in the BSC. Do not overload, e.g. no more than 6–8 specimens for processing at a time, according to centrifuge capacity. • All needed material should be present in the BSC so that work is not interrupted and moves in and out of the BSC are minimized. 14 Is flame allowed in the BSC? • Avoid continuous flame = permanent source of heat • Use intermittent burner • Can be used in BSC I or II 15 Biosafety levels 16 WHO recommendations for BSL2 (specimen processing for TB cultures) • BSCs should be ducted or vented to the outside. • Air from BSCs must not be allowed to recirculate into the room in TB laboratories. • An adequate budget for regular maintenance and servicing is essential. 17 WHO recommendations for handling TB cultures In addition to BSL2 recommendations: • Isolation of the laboratory (containment room). • Anteroom with a double-door entry; may consist of a BSL2 room • Ventilation: directional airflow, controlled ventilating system. • Autoclave on site (but not mandatory in the containment room). 18 Laboratory for handling TB cultures 19 Which biosafety level for TB laboratory activities? Microscopy in a well-ventilated room Culture = specimen processing in a BSC in a BSL2 Culture identification and DST = BSL2 containment room with ventilation: directional airflow from functionally clean to dirty areas, controlled ventilating system ensuring 6 to 12 air exchanges per hour. 20 Standard practices • Limited access to the laboratory. • No eating, drinking, smoking, etc. • No mouth-pipetting, no chewing pencils, etc. • Assume that ALL specimens are potentially infectious. 21 Standard practices • Hand-washing (dry with disposable paper). • Work surfaces to be decontaminated at least once a day. 22 Good microbiological techniques • Good microbiological techniques (GMT): working methods applied to minimize exposure to pathogens via, for example, aerosols, splashes, accidental inoculation. • GMT are fundamental to laboratory safety. • Specialized equipment may support good laboratory practice but does not replace it. 23 Personnel qualifications: proper training For culture procedure: • • • • • • • • • • • TB disease and transmission; wearing and use of protective equipment and clothing; handling of infectious materials; laboratory design, including air flow conditions; use of BSC, centrifuge (operation, identification of malfunctions, maintenance); preventing and coping with incidents; good laboratory practice and good microbiological techniques; organization of work flow procedures; waste management; importance of laboratory results for patient management; importance of laboratory results for the national TB programme. 24 Personal protective equipment • Masks/respirators • Gloves • Gowns 25 Personal protective equipment – masks • Surgical masks prevent the spread of microorganisms from the wearer (protection from exhalation). • Masks do not provide protection to the wearer against inhaling small infectious aerosols. 26 Personal protective equipment – respirators N95/FFP2 respirators effectively filter out more than 95% (98% for FFP3) of particles 0.3 µm or more in diameter. Respirators have to be fitted to the face. Facial hair causes the respirator to be ineffective. N95/FFP2 FFP3 27 Personal protective equipment – respirators Respirators may be worn in settings of high MDR-TB and/or HIV prevalence, where staff may be HIV-infected and highly susceptible to infectious aerosols. Respirators must be available in all culture/DST labs for coping with spillages outside the BSC. 28 Personal protective equipment – gloves • Gloves should always be worn while specimen processing and handling TB cultures. • Wearing gloves can give technicians a false sense of safety. • Frequent hand-washing and care in the handling of contaminated materials are good laboratory practices. • Gloves should be removed at every interruption of work and should not be reused. Hands should be washed after removal of gloves. 29 Personal protective equipment – gowns • Gowns must always be worn inside the laboratory (but never outside) and should be changed regularly, at least weekly. • Gowns should preferably be fully buttoned, longsleeved with narrow cuffs, and back-opening. 30 Removing PPE Remove PPE in the following order: 1.Disposable gloves 1.Respirator/mask 1.Gown/coat/suit/overalls 31 Personal protective equipment – conclusion • Hand-washing and GMT are acceptable practices for most countries. • Each country must evaluate the risks and decide on the level of personal protection equipment that is appropriate, given the available resources. 32 Disinfectants • A disinfectant is a chemical or mixture of chemicals used to kill microorganisms. • Disinfectants are usually applied to surfaces or inanimate objects. • Disinfectants may be used for pre-decontamination treatment, before autoclaving. Because of their specific cell wall structure, TB bacilli are resistant to most standard disinfectants, e.g. quaternary ammonium compounds are ineffective. 33 Disinfectants The only adequate disinfectants against TB bacilli are: • Phenol, 2–5%: very irritant to skin, use derivatives. • Hypochlorite (bleach): corrosive to metals. • Alcohol 70%, no residue, use on skin and work surfaces. • Iodophores, 3–5%, iodine plus inert polymer. • Glutaraldehyde, requires an activator, highly irritant to skin. 34 Disinfectants • Diluted solutions should be prepared daily. • Stock solutions should be stored according to manufacturer's recommendations. • Use commercial solutions for “dirty or worst possible situations”. • Follow national chemical safety guidelines. [to be adjusted to local policy] 35 Waste disposal • All infected materials, including closed specimen containers, should be placed in the BSC in autoclavable bags. • All cultures and related materials should be autoclaved. • All material handled in the BSC should be considered as infected. 36 Incident: spill 37 Spill in the BSC – what to do • Cover the spill with absorbent paper towel. • Pour over disinfectant and leave for at least 2 hours. • Discard absorbent tissue and all clean-up material in an autoclavable bag and autoclave. 38 Spill outside the BSC • EVACUATE the room and stay outside with the door closed for at least 2 hours. • Using appropriate respiratory protection devices, return to the accident area to clean the spill. • Cover the spill with paper towel and pour over disinfectant. Leave for at least 2 hours. • Once disinfection is complete, discard all waste into suitable waste containers and autoclave. 39 Spill outside the BSC Emergency spill kit should be available in all culture/DST laboratories, with: •all personal protective equipment (overalls, overshoes, gloves, respirators); •Paper towels; •large quantities of disinfectant. 40 Chemical safety • Alcohols are flammable: avoid flame • Phenol is corrosive: – avoid direct contact with the skin or mucous membranes; – limit exposure to phenolic fumes. 41 Chemical safety: handling acids ALWAYS ADD ACID TO WATER NEVER ADD WATER TO ACID WATER ACID WATER ACID 42 SAFETY FIRST! 43 True and false exercise 1. Surgical masks protect you from TB infection. 2. Remove personal protective equipment in the following order: respirator/mask disposable gloves gowns/coats/suits/overalls. 3. In case of spills outside the BSC, you should evacuate the room and stay outside with the door closed for at least 30 minutes. 44 Module review: take-home messages Never smoke, eat, or drink in the laboratory. Wash your hands frequently with soap and water before and after performing any procedures. Avoid hazards in a TB laboratory by paying careful attention to safety procedures. Always work carefully and in a safe manner following good microbiological technique. The additional protection conferred by respirators must be assessed for each setting. 45 Self-assessment • How is TB transmitted from person to person? • What are the sources of infectious aerosols in a laboratory? • What is the critical equipment for safe culture and DST? • What personal protective equipment is recommended for TB laboratory activities? • What are the most efficient disinfectants in TB laboratories? • What procedures should be followed when coping with accidents? • What precautions should be taken when handling acids? 46